Monday Poster Session
Category: Interventional Endoscopy
P3570 - Gangliocytic Paraganglioma of the Distal Duodenum: A Case for Endoscopic Submucosal Dissection (ESD) Over Surgery
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Ritu Channagiri, BS
Florida Atlantic University Charles E. Schmidt College of Medicine
Boca Raton, FL
Presenting Author(s)
Ritu Channagiri, BS1, Allison Chin, MD2, Zoilo K.. Suarez, MD3, Jalal Samhoun, MD1, David Forcione, MD4
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL; 3University of Arizona, Chandler, AZ; 4Baptist Health, Boca Raton, FL
Introduction: Gangliocytic paragangliomas (GPs) are rare neuroendocrine tumors typically located in the second portion of the duodenum. Classical presentation includes nonspecific gastrointestinal symptoms, and due to their histologic similarity to well-differentiated neuroendocrine tumors (WDNETs) or carcinoid tumors, they are frequently misdiagnosed. Therefore, further investigation into this disease course is warranted to optimize management of these tumors. This case describes a rare presentation of distal, duodenal GP in a patient with gastrointestinal bleeding.
Case Description/
Methods: A 50-year-old male with a history of testicular cancer presented with a week-long history of melena, fatigue, lightheadedness, and exertional dyspnea. Laboratory testing revealed a hemoglobin level of 5.7 g/dL in the setting of intermittent nonsteroidal anti-inflammatory drug (NSAID) use for migraines. Esophagogastroduodenoscopy (EGD) revealed no active bleeding, however capsule endoscopy revealed a lesion in the distal duodenum. Endoscopic ultrasound identified a 2.7 cm mural mass in the third portion of the duodenum which resulted as a GP with positive staining for progesterone receptors in epithelioid cells per fine-needle aspiration without evidence of lymphadenopathy or distant metastasis per CT Enterography. Per shared decision making and given submucosal involvement, endoscopic submucosal dissection (ESD) was performed to achieve complete excision of the mass with clip closure.
Discussion: GP of the duodenum is a rare neuroendocrine tumor (NET) that usually arises in the second portion of the duodenum and usually presents with gastrointestinal bleeding, anemia, or abdominal pain. Its diagnosis is often challenging due to its submucosal location and shared histological features with other NETs. Although generally considered benign, metastatic features have been reported in 11–15% of cases. In our case, a localized and non-invasive GP was successfully resected with ESD, allowing en-bloc resection with clear margins. The purpose of this case is to highlight the importance of including a GP in the differential diagnosis of duodenal submucosal masses presenting with bleeding. It also supports ESD as a safe, effective treatment in selected patients.
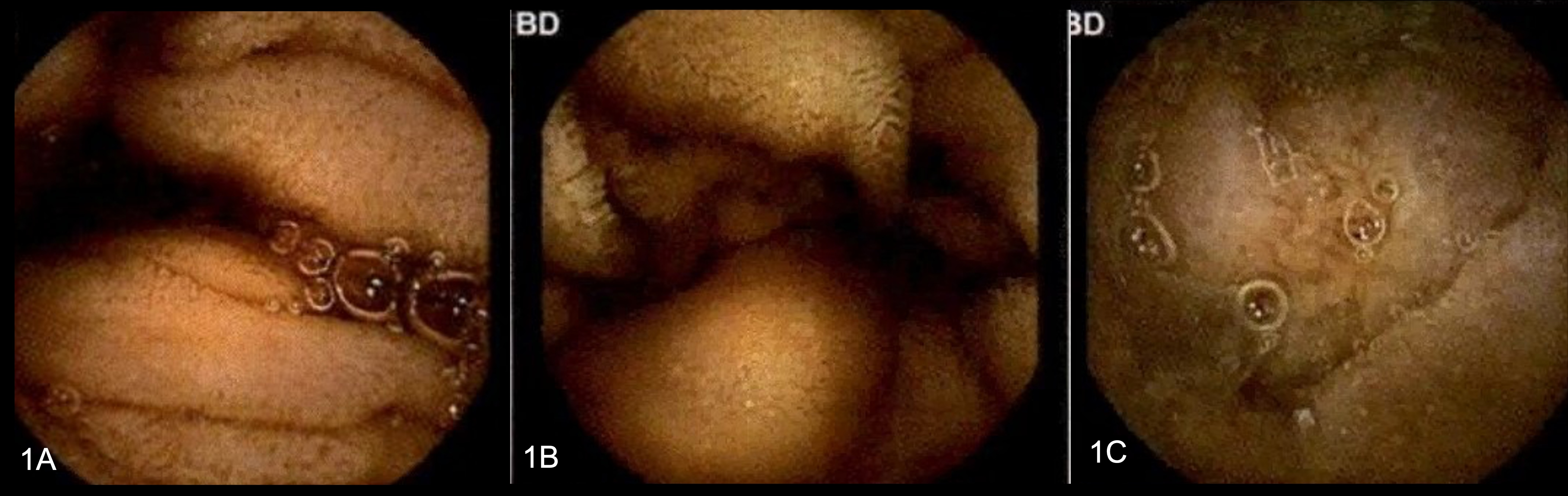
Figure: Figures 1A, 1B, and 1C above are from capsule endoscopy revealing mass in the duodenum and showing scalloping of the mucosa.
Disclosures:
Ritu Channagiri indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
Zoilo Suarez indicated no relevant financial relationships.
Jalal Samhoun indicated no relevant financial relationships.
David Forcione indicated no relevant financial relationships.
Ritu Channagiri, BS1, Allison Chin, MD2, Zoilo K.. Suarez, MD3, Jalal Samhoun, MD1, David Forcione, MD4. P3570 - Gangliocytic Paraganglioma of the Distal Duodenum: A Case for Endoscopic Submucosal Dissection (ESD) Over Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Florida Atlantic University Charles E. Schmidt College of Medicine, Miami, FL; 3University of Arizona, Chandler, AZ; 4Baptist Health, Boca Raton, FL
Introduction: Gangliocytic paragangliomas (GPs) are rare neuroendocrine tumors typically located in the second portion of the duodenum. Classical presentation includes nonspecific gastrointestinal symptoms, and due to their histologic similarity to well-differentiated neuroendocrine tumors (WDNETs) or carcinoid tumors, they are frequently misdiagnosed. Therefore, further investigation into this disease course is warranted to optimize management of these tumors. This case describes a rare presentation of distal, duodenal GP in a patient with gastrointestinal bleeding.
Case Description/
Methods: A 50-year-old male with a history of testicular cancer presented with a week-long history of melena, fatigue, lightheadedness, and exertional dyspnea. Laboratory testing revealed a hemoglobin level of 5.7 g/dL in the setting of intermittent nonsteroidal anti-inflammatory drug (NSAID) use for migraines. Esophagogastroduodenoscopy (EGD) revealed no active bleeding, however capsule endoscopy revealed a lesion in the distal duodenum. Endoscopic ultrasound identified a 2.7 cm mural mass in the third portion of the duodenum which resulted as a GP with positive staining for progesterone receptors in epithelioid cells per fine-needle aspiration without evidence of lymphadenopathy or distant metastasis per CT Enterography. Per shared decision making and given submucosal involvement, endoscopic submucosal dissection (ESD) was performed to achieve complete excision of the mass with clip closure.
Discussion: GP of the duodenum is a rare neuroendocrine tumor (NET) that usually arises in the second portion of the duodenum and usually presents with gastrointestinal bleeding, anemia, or abdominal pain. Its diagnosis is often challenging due to its submucosal location and shared histological features with other NETs. Although generally considered benign, metastatic features have been reported in 11–15% of cases. In our case, a localized and non-invasive GP was successfully resected with ESD, allowing en-bloc resection with clear margins. The purpose of this case is to highlight the importance of including a GP in the differential diagnosis of duodenal submucosal masses presenting with bleeding. It also supports ESD as a safe, effective treatment in selected patients.
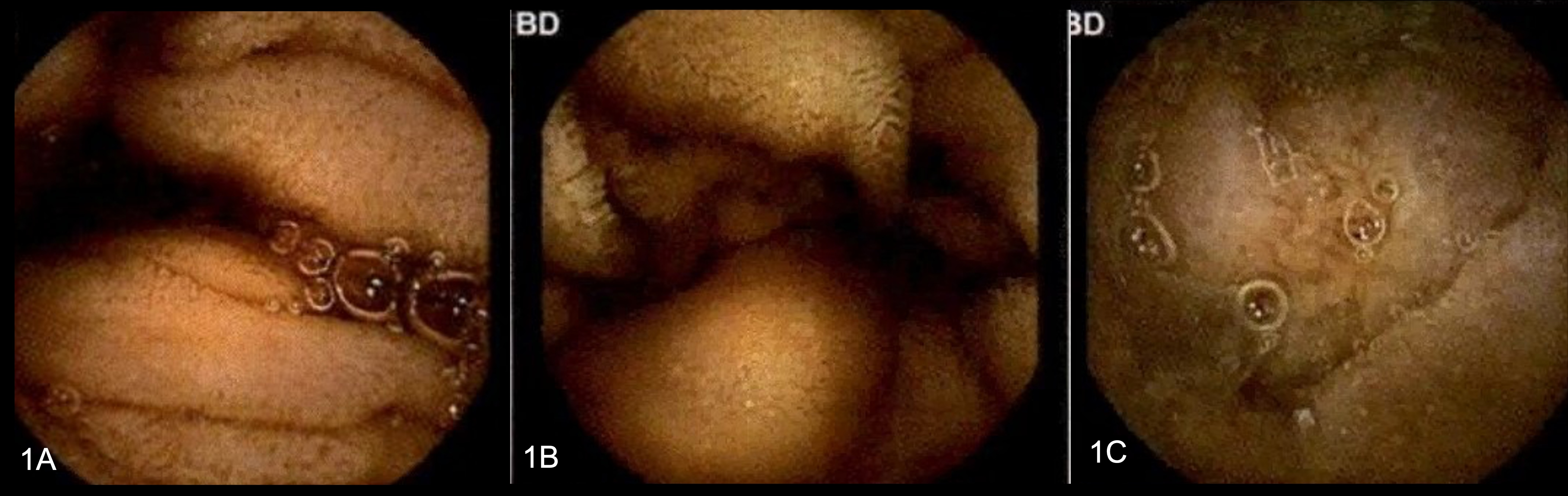
Figure: Figures 1A, 1B, and 1C above are from capsule endoscopy revealing mass in the duodenum and showing scalloping of the mucosa.
Disclosures:
Ritu Channagiri indicated no relevant financial relationships.
Allison Chin indicated no relevant financial relationships.
Zoilo Suarez indicated no relevant financial relationships.
Jalal Samhoun indicated no relevant financial relationships.
David Forcione indicated no relevant financial relationships.
Ritu Channagiri, BS1, Allison Chin, MD2, Zoilo K.. Suarez, MD3, Jalal Samhoun, MD1, David Forcione, MD4. P3570 - Gangliocytic Paraganglioma of the Distal Duodenum: A Case for Endoscopic Submucosal Dissection (ESD) Over Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
