Monday Poster Session
Category: Liver
P3686 - SGLT-2 Inhibitors: A Game Changer for Cirrhosis? Examining Mortality, Hepatocellular Cancer, and Liver Transplantation Rates
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chidera Onwuzo, MBBS (he/him/his)
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Sara Bourdages, MD1, Eloho Olojakpoke, MBBS1, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Al-Aman Shaukat, MBBS1
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Cleveland Clinic Foundation, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA; 5University of Florida College of Medicine, Jacksonville, FL
Introduction: Cirrhosis is a chronic liver condition characterized by progressive hepatic dysfunction and complications, including the need for liver transplantation. Emerging evidence suggests that sodium-glucose cotransporter-2 (SGLT-2) inhibitors, originally developed for managing type 2 diabetes, may offer benefits in patients with cirrhosis. This study aims to provide insights into the impact of SGLT-2 therapy on key clinical outcomes, including liver transplantation, hepatocellular carcinoma (HCC), and all-cause mortality.
Methods: We conducted a retrospective analysis using deidentified, aggregate patient data from the TriNetX research network. The cohort comprised patients ≥18 years old with a diagnosis of cirrhosis. Patients who commenced SGLT-2 inhibitors after the diagnosis of cirrhosis were identified. Primary outcomes included liver transplantation, HCC, and all-cause mortality. Variables such as age, sex, race, comorbidities (e.g., diabetes, obesity, chronic kidney disease, hypertension), and lifestyle factors (e.g., tobacco use, alcohol dependence) underwent 1:1 propensity matching to reduce confounding. Odds ratios (OR) with 95% confidence intervals (CI) were reported for the matched cohorts.
Results: The matched cohort analysis demonstrated a significant reduction in the necessity for liver transplantation (OR 0.666, 95% CI 0.542–0.818) and all-cause mortality (OR 0.321, 95% CI 0.304–0.340) among patients receiving SGLT-2 inhibitors. Furthermore, a noteworthy decrease in the incidence of hepatocellular carcinoma was observed (OR 0.933, 95% CI 0.859–1.013), highlighting the potential protective effects of SGLT-2 therapy in this patient population. These findings underscore the clinical significance of SGLT-2 inhibitors in improving outcomes for individuals with cirrhosis.
Discussion: This study provides solid evidence that using SGLT-2 inhibitors is associated with reduced the need for liver transplantation and lowers all-cause mortality in cirrhosis patients. Furthermore, the observed decrease in hepatocellular carcinoma incidence implies that SGLT-2 inhibitors may have a preventive impact, underscoring their value in cirrhosis therapy. These findings emphasize the necessity to consider SGLT-2 therapy as a vital component in maximizing patient outcomes and enhancing the overall care of cirrhosis patients.
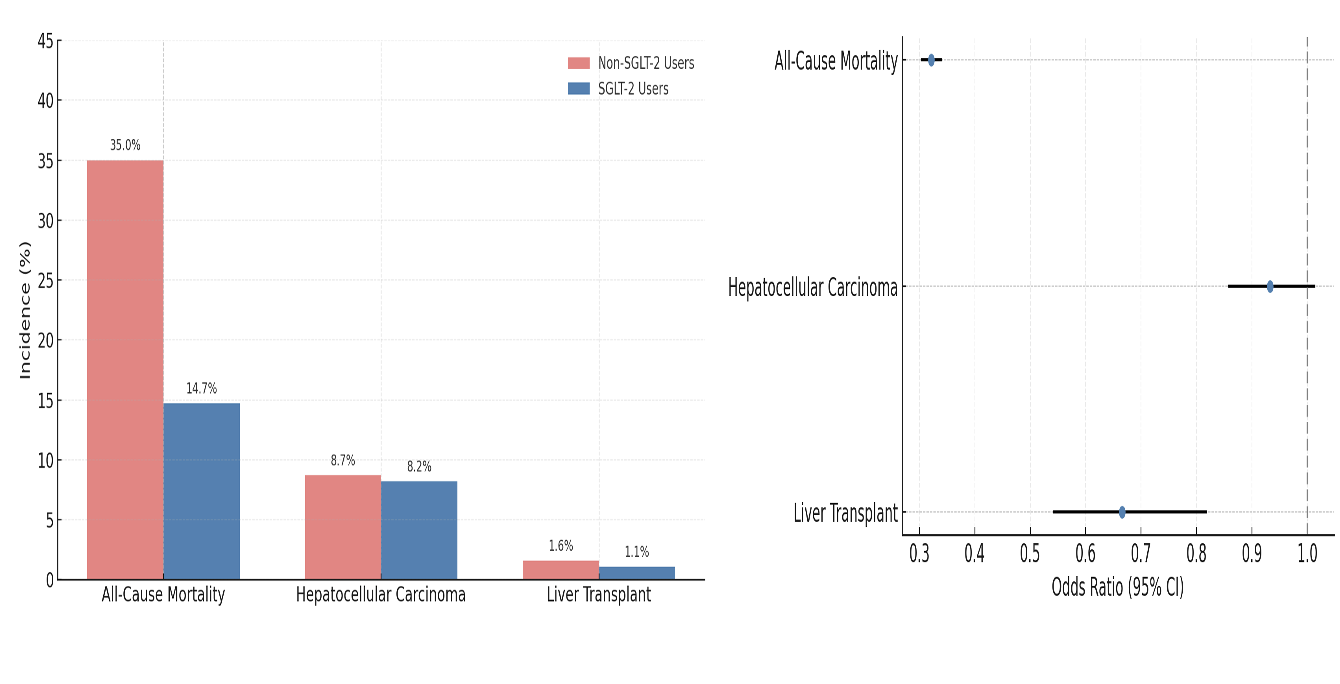
Figure: Table 1: Comparison of Demographics and Comorbidities of SGLT-2 Inhibitors Group vs Non SGLT-2 Inhibitors Group Before and After Propensity Score Matching
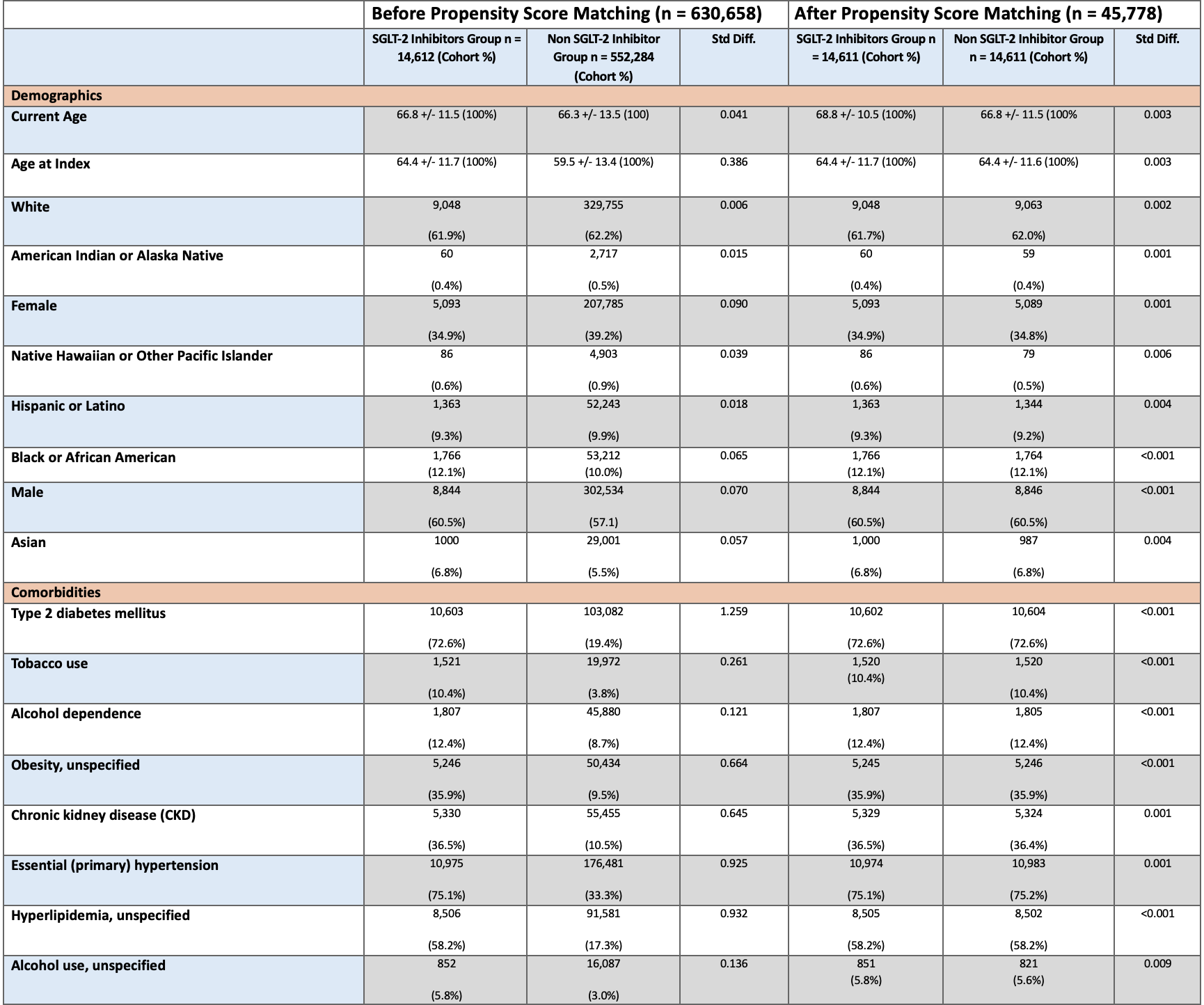
Figure: Figure 1: Comparative Risk and Odds Ratio of Adverse Outcomes with SGLT-2 Inhibitor Use in Cirrhosis
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Sara Bourdages indicated no relevant financial relationships.
Eloho Olojakpoke indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Al-Aman Shaukat indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Sara Bourdages, MD1, Eloho Olojakpoke, MBBS1, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Al-Aman Shaukat, MBBS1. P3686 - SGLT-2 Inhibitors: A Game Changer for Cirrhosis? Examining Mortality, Hepatocellular Cancer, and Liver Transplantation Rates, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Sara Bourdages, MD1, Eloho Olojakpoke, MBBS1, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Al-Aman Shaukat, MBBS1
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Cleveland Clinic Foundation, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA; 5University of Florida College of Medicine, Jacksonville, FL
Introduction: Cirrhosis is a chronic liver condition characterized by progressive hepatic dysfunction and complications, including the need for liver transplantation. Emerging evidence suggests that sodium-glucose cotransporter-2 (SGLT-2) inhibitors, originally developed for managing type 2 diabetes, may offer benefits in patients with cirrhosis. This study aims to provide insights into the impact of SGLT-2 therapy on key clinical outcomes, including liver transplantation, hepatocellular carcinoma (HCC), and all-cause mortality.
Methods: We conducted a retrospective analysis using deidentified, aggregate patient data from the TriNetX research network. The cohort comprised patients ≥18 years old with a diagnosis of cirrhosis. Patients who commenced SGLT-2 inhibitors after the diagnosis of cirrhosis were identified. Primary outcomes included liver transplantation, HCC, and all-cause mortality. Variables such as age, sex, race, comorbidities (e.g., diabetes, obesity, chronic kidney disease, hypertension), and lifestyle factors (e.g., tobacco use, alcohol dependence) underwent 1:1 propensity matching to reduce confounding. Odds ratios (OR) with 95% confidence intervals (CI) were reported for the matched cohorts.
Results: The matched cohort analysis demonstrated a significant reduction in the necessity for liver transplantation (OR 0.666, 95% CI 0.542–0.818) and all-cause mortality (OR 0.321, 95% CI 0.304–0.340) among patients receiving SGLT-2 inhibitors. Furthermore, a noteworthy decrease in the incidence of hepatocellular carcinoma was observed (OR 0.933, 95% CI 0.859–1.013), highlighting the potential protective effects of SGLT-2 therapy in this patient population. These findings underscore the clinical significance of SGLT-2 inhibitors in improving outcomes for individuals with cirrhosis.
Discussion: This study provides solid evidence that using SGLT-2 inhibitors is associated with reduced the need for liver transplantation and lowers all-cause mortality in cirrhosis patients. Furthermore, the observed decrease in hepatocellular carcinoma incidence implies that SGLT-2 inhibitors may have a preventive impact, underscoring their value in cirrhosis therapy. These findings emphasize the necessity to consider SGLT-2 therapy as a vital component in maximizing patient outcomes and enhancing the overall care of cirrhosis patients.
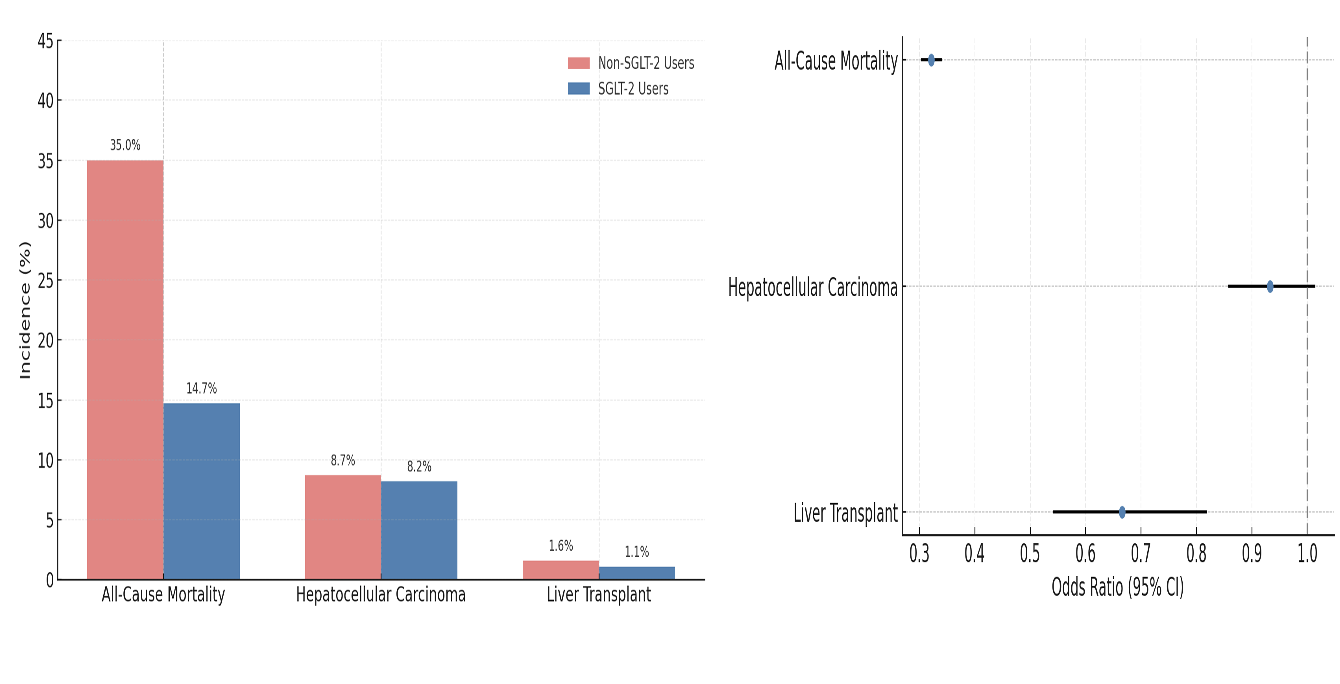
Figure: Table 1: Comparison of Demographics and Comorbidities of SGLT-2 Inhibitors Group vs Non SGLT-2 Inhibitors Group Before and After Propensity Score Matching
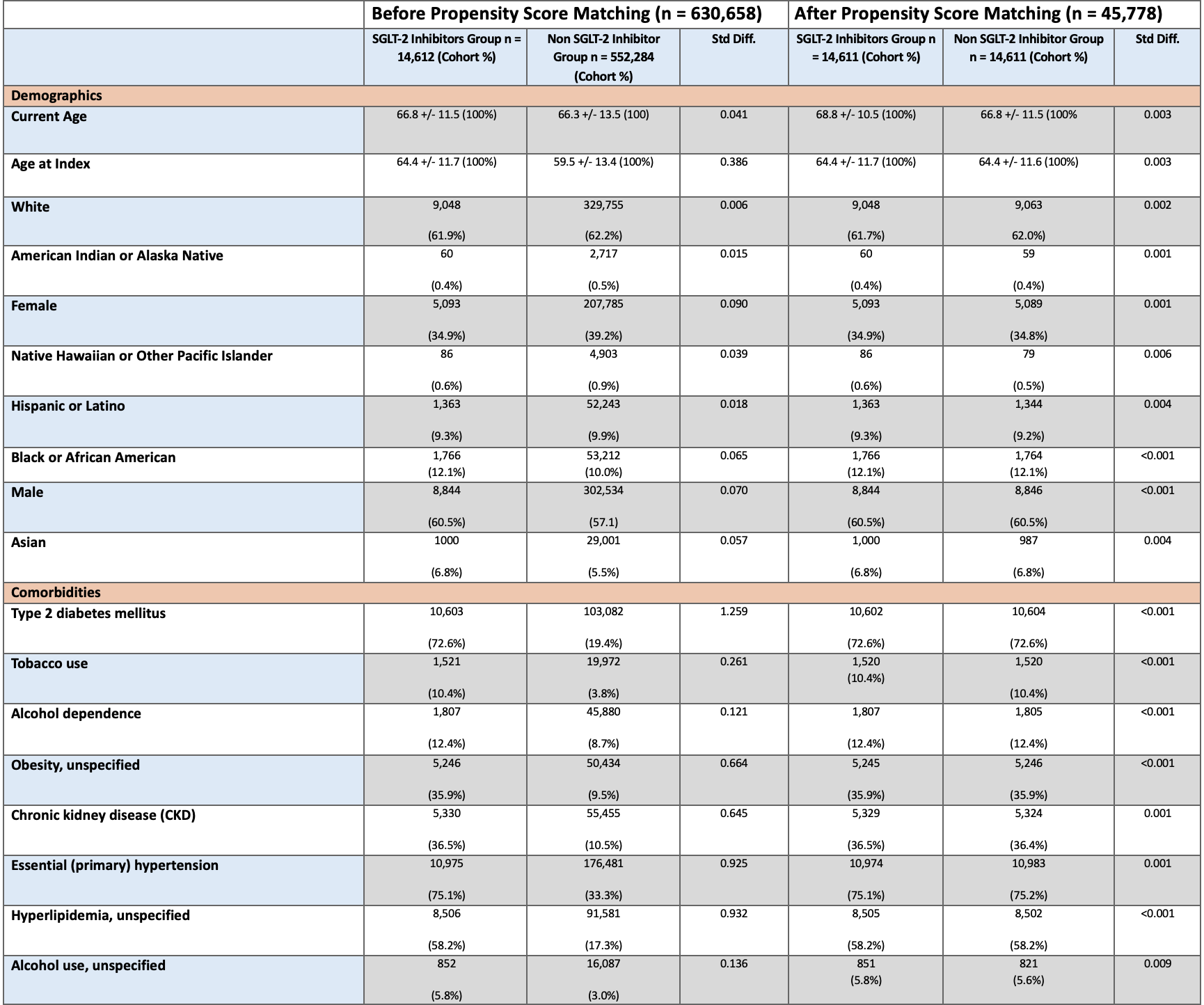
Figure: Figure 1: Comparative Risk and Odds Ratio of Adverse Outcomes with SGLT-2 Inhibitor Use in Cirrhosis
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Sara Bourdages indicated no relevant financial relationships.
Eloho Olojakpoke indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Al-Aman Shaukat indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Sara Bourdages, MD1, Eloho Olojakpoke, MBBS1, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Al-Aman Shaukat, MBBS1. P3686 - SGLT-2 Inhibitors: A Game Changer for Cirrhosis? Examining Mortality, Hepatocellular Cancer, and Liver Transplantation Rates, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


