Monday Poster Session
Category: Liver
P3681 - Temporal Trends and Disparities in Hepatocellular Carcinoma Mortality Among Cirrhotic Patients in the United States: Insights From CDC Wonder Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Jaan, MD
Unity Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3
1Unity Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Hepatocellular carcinoma (HCC), predominantly arising in the setting of cirrhosis, constitutes a formidable oncologic burden, with mortality patterns shaped by evolving epidemiological factors. Delineating mortality patterns and demographic differentials is imperative for addressing underlying inequities and informing precise public health strategies.
Methods: The CDC WONDER database was queried for deaths attributed to HCC with concomitant cirrhosis in adults (≥25 years) from 1999 to 2020. Age-adjusted mortality rates (AAMRs), standardized per 1,000,000 individuals, were examined, and joinpoint regression analysis was employed to compute annual percent changes (APCs), with particular emphasis on disparities stratified by sex, race, and geographic region.
Results: Between 1999 and 2020, HCC mortality among cirrhotic patients exhibited a substantial rise, with AAMR escalating from 6.9 to 15.2 per 1,000,000, corresponding to an average annual percent change (AAPC) of 3.64 (95% CI: 3.41-3.95, p< 0.000001). Gender disparities were pronounced, with males bearing a consistently elevated mortality burden throughout the study period (average AAMR males: 18.8 vs females: 4). Nonetheless, the overarching progression remained analogous between genders (AAPC males: 3.56 vs females: 3.94, p< 0.000001), characterized by a notably steep inflation following 2005. Racial heterogeneity was also evident, wherein non-Hispanic White individuals exhibited a uniquely upward trajectory throughout the study period (AAPC: 4.13, p < 0.000001), contrary to Asians who experienced a marginal, insignificant decline (AAPC -0.05, p =0.96). Despite an initial regression, Hispanic individuals, overall, exhibited the highest mortality rate (AAMR: 22.3), abruptly ascending between 2007 and 2018 (APC: 4.37, p< 0.000001), while Black individuals also showed an overall increase (AAPC 3.20, p=0.000001). Geographically, AAMRs spanned from 6 in Mississippi to 20.4 in Texas, and the Western Region exhibited the highest average AAMR at 14.3.
Discussion: These findings reveal a concerning rise in HCC-related mortality in patients with cirrhosis over the past two decades, driven by a disproportionate burden, underscoring the need for targeted surveillance and equitable care to mitigate the growing impact of HCC in the United States.
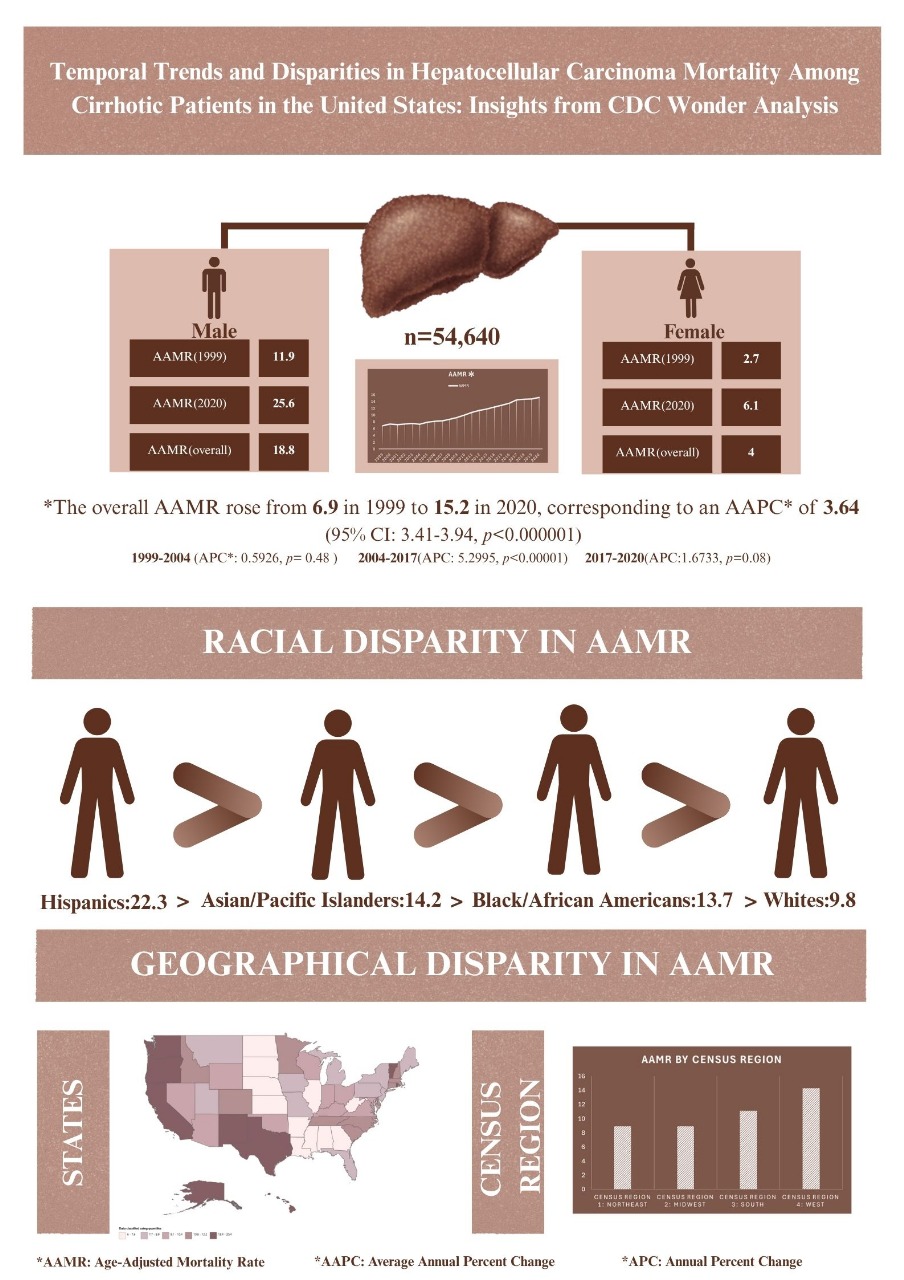
Figure: Demographic Profiles and Disparities in Hepatocellular Carcinoma(HCC)-Related Mortality among Cirrhotic adults (≥ 25) in United States, 1999 to 2020
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Kamran Qureshi indicated no relevant financial relationships.
Wing-Kin Syn indicated no relevant financial relationships.
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3. P3681 - Temporal Trends and Disparities in Hepatocellular Carcinoma Mortality Among Cirrhotic Patients in the United States: Insights From CDC Wonder Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Unity Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Hepatocellular carcinoma (HCC), predominantly arising in the setting of cirrhosis, constitutes a formidable oncologic burden, with mortality patterns shaped by evolving epidemiological factors. Delineating mortality patterns and demographic differentials is imperative for addressing underlying inequities and informing precise public health strategies.
Methods: The CDC WONDER database was queried for deaths attributed to HCC with concomitant cirrhosis in adults (≥25 years) from 1999 to 2020. Age-adjusted mortality rates (AAMRs), standardized per 1,000,000 individuals, were examined, and joinpoint regression analysis was employed to compute annual percent changes (APCs), with particular emphasis on disparities stratified by sex, race, and geographic region.
Results: Between 1999 and 2020, HCC mortality among cirrhotic patients exhibited a substantial rise, with AAMR escalating from 6.9 to 15.2 per 1,000,000, corresponding to an average annual percent change (AAPC) of 3.64 (95% CI: 3.41-3.95, p< 0.000001). Gender disparities were pronounced, with males bearing a consistently elevated mortality burden throughout the study period (average AAMR males: 18.8 vs females: 4). Nonetheless, the overarching progression remained analogous between genders (AAPC males: 3.56 vs females: 3.94, p< 0.000001), characterized by a notably steep inflation following 2005. Racial heterogeneity was also evident, wherein non-Hispanic White individuals exhibited a uniquely upward trajectory throughout the study period (AAPC: 4.13, p < 0.000001), contrary to Asians who experienced a marginal, insignificant decline (AAPC -0.05, p =0.96). Despite an initial regression, Hispanic individuals, overall, exhibited the highest mortality rate (AAMR: 22.3), abruptly ascending between 2007 and 2018 (APC: 4.37, p< 0.000001), while Black individuals also showed an overall increase (AAPC 3.20, p=0.000001). Geographically, AAMRs spanned from 6 in Mississippi to 20.4 in Texas, and the Western Region exhibited the highest average AAMR at 14.3.
Discussion: These findings reveal a concerning rise in HCC-related mortality in patients with cirrhosis over the past two decades, driven by a disproportionate burden, underscoring the need for targeted surveillance and equitable care to mitigate the growing impact of HCC in the United States.
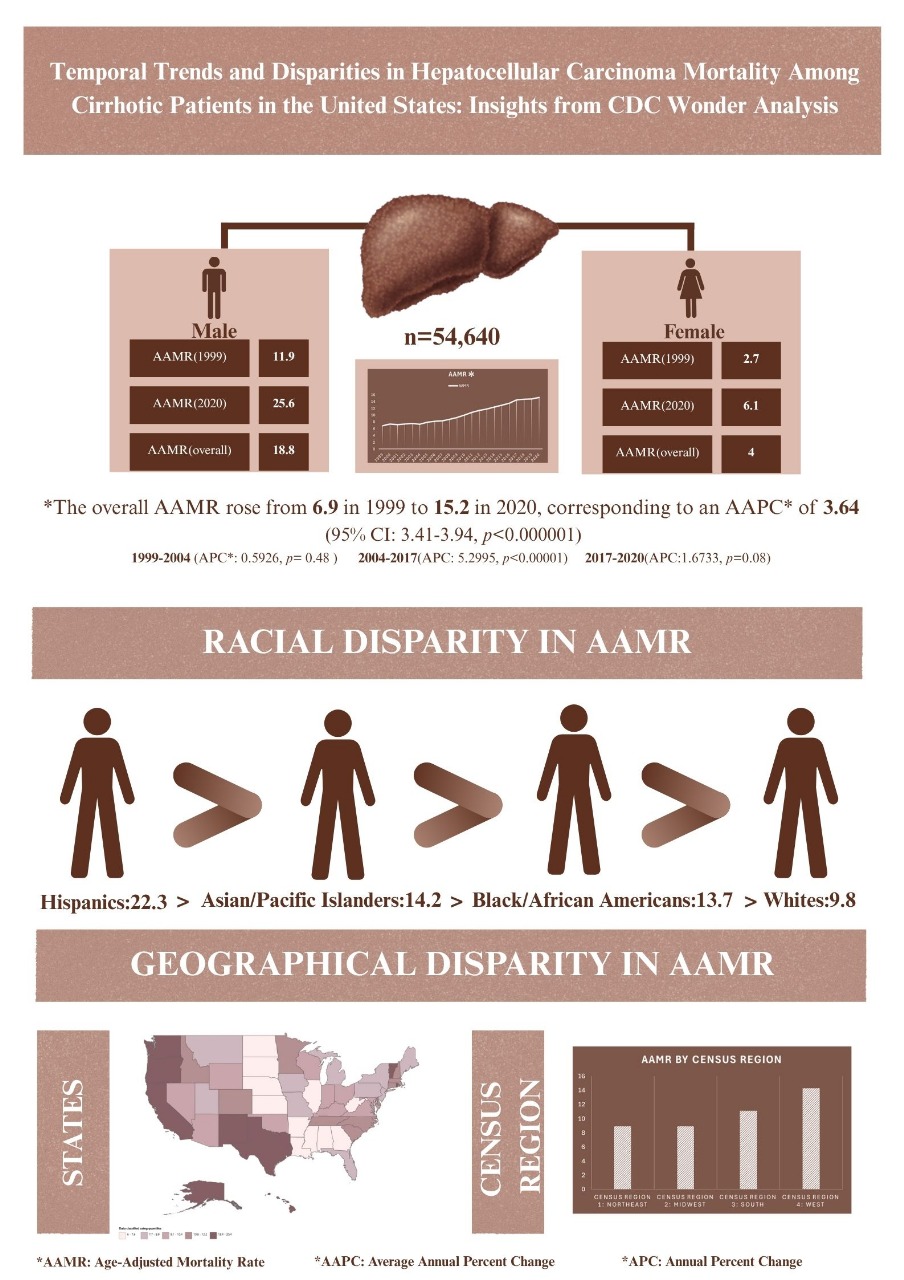
Figure: Demographic Profiles and Disparities in Hepatocellular Carcinoma(HCC)-Related Mortality among Cirrhotic adults (≥ 25) in United States, 1999 to 2020
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Kamran Qureshi indicated no relevant financial relationships.
Wing-Kin Syn indicated no relevant financial relationships.
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3. P3681 - Temporal Trends and Disparities in Hepatocellular Carcinoma Mortality Among Cirrhotic Patients in the United States: Insights From CDC Wonder Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
