Monday Poster Session
Category: Liver
P3674 - Unveiling Disparities in Liver Cirrhosis–Related Mortality in the United States: A 24-Year Longitudinal Analysis (1999–2023)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rahul Kumar, MD (he/him/his)
North Central Bronx Hospital
Bronx, NY
Presenting Author(s)
Rahul Kumar, MD1, Avinash Nankani, MBBS2, Osman Wafai, MBBS3,Mujtaba Hyder, MBBS2, Diksha Kajal, MD4, FNU Murlidhar, MBBS, MD5, Karan J.. Yagnik, MD6, Joo Hee Park, MD1, Fnu Vikash, MD7
1North Central Bronx Hospital, Bronx, NY; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Jinnah Medical and Dental College, Karachi, Sindh, Pakistan; 4Florida State University, Cape Coral, FL; 5Mayo Clinic, Rochester, MN; 6Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 7Cleveland Clinic Foundation, New York, NY
Introduction: Liver cirrhosis remains a significant cause of morbidity and mortality in the United States. Although previous studies have reported national death rates related to cirrhosis, the rising burden of nonalcoholic fatty liver disease and the continued impact of alcohol-associated liver disease, highlight the importance of updated analyses. This study aims to characterize temporal trends and regional variations in cirrhosis-related mortality of different demographic populations.
Methods: We performed a retrospective analysis study of U.S. adults using the CDC WONDER Multiple Cause of Death database from 1999 to 2023. Liver cirrhosis deaths were identified via ICD-10 codes K70.3 and K74. Annual age-adjusted mortality rates per 100,000 population were calculated using the direct standardization method, applying the 2000 U.S. standard population. We stratified analyses by sex, race/ethnicity, and U.S. Census region. Joinpoint regression identified inflection points in the trend lines and computed Annual Percent Change (APC) with 95% confidence intervals.
Results: The overall age-adjusted mortality rate (AAMR) rose from 13.7 (95% CI: 13.5–13.8) in 1999 to 15.9 (95% CI: 15.8–16.1) in 2023, peaking at 16.8 (95% CI: 16.7-17) in 2021. Joinpoint analysis revealed significant nationwide acceleration from 2018 to 2021 (APC: 6.74). Women experienced a steeper increase during this period (APC: 8.33) followed by a plateau, while men showed a significant steady increase from 2008 to 2023 (APC 1.80). Notable racial disparities included a marked increase among American Indian/Alaska Native individuals from 2018–2020 (APC 12.34), followed by Black individuals for the same period (APC 6.30), and a steady rise for White individuals from 2008 to 2020 (APC 2.34). In contrast, Asian/Pacific Islanders saw a decline from 1999 to 2015 (APC -1.81). Geographically, the West had the sharpest recent increase from 2018 to 2021 (APC 9.03), while the South and Midwest demonstrated sustained upward trends beginning in 2008 and 2009, respectively.
Discussion: These findings underscore a growing national burden of cirrhosis-related mortality, particularly among women, American Indian/Alaska Native, and Black populations, and in Western regions, highlighting the need for targeted public health interventions focused on modifiable risk factors such as nonalcoholic fatty liver disease and alcohol use.
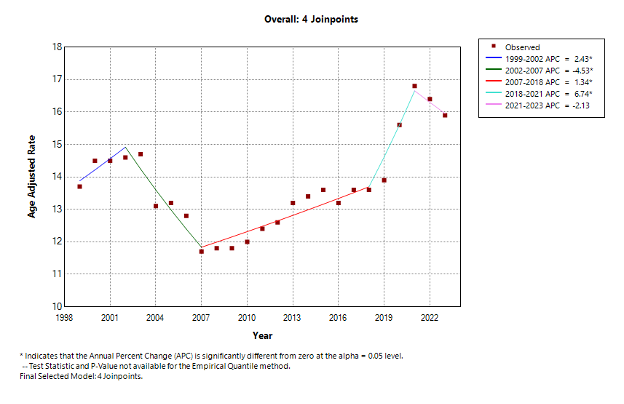
Figure: JoinPoint Model Overall
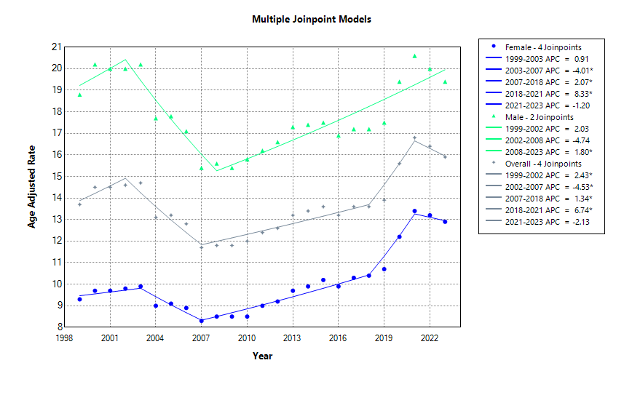
Figure: JoinPoint Model Male vs Female
Disclosures:
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Osman Wafai indicated no relevant financial relationships.
Mujtaba Hyder indicated no relevant financial relationships.
Diksha Kajal indicated no relevant financial relationships.
FNU Murlidhar indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Rahul Kumar, MD1, Avinash Nankani, MBBS2, Osman Wafai, MBBS3, Mujtaba Hyder, MBBS2, Diksha Kajal, MD4, FNU Murlidhar, MBBS, MD5, Karan J.. Yagnik, MD6, Joo Hee Park, MD1, Fnu Vikash, MD7. P3674 - Unveiling Disparities in Liver Cirrhosis–Related Mortality in the United States: A 24-Year Longitudinal Analysis (1999–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1North Central Bronx Hospital, Bronx, NY; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Jinnah Medical and Dental College, Karachi, Sindh, Pakistan; 4Florida State University, Cape Coral, FL; 5Mayo Clinic, Rochester, MN; 6Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 7Cleveland Clinic Foundation, New York, NY
Introduction: Liver cirrhosis remains a significant cause of morbidity and mortality in the United States. Although previous studies have reported national death rates related to cirrhosis, the rising burden of nonalcoholic fatty liver disease and the continued impact of alcohol-associated liver disease, highlight the importance of updated analyses. This study aims to characterize temporal trends and regional variations in cirrhosis-related mortality of different demographic populations.
Methods: We performed a retrospective analysis study of U.S. adults using the CDC WONDER Multiple Cause of Death database from 1999 to 2023. Liver cirrhosis deaths were identified via ICD-10 codes K70.3 and K74. Annual age-adjusted mortality rates per 100,000 population were calculated using the direct standardization method, applying the 2000 U.S. standard population. We stratified analyses by sex, race/ethnicity, and U.S. Census region. Joinpoint regression identified inflection points in the trend lines and computed Annual Percent Change (APC) with 95% confidence intervals.
Results: The overall age-adjusted mortality rate (AAMR) rose from 13.7 (95% CI: 13.5–13.8) in 1999 to 15.9 (95% CI: 15.8–16.1) in 2023, peaking at 16.8 (95% CI: 16.7-17) in 2021. Joinpoint analysis revealed significant nationwide acceleration from 2018 to 2021 (APC: 6.74). Women experienced a steeper increase during this period (APC: 8.33) followed by a plateau, while men showed a significant steady increase from 2008 to 2023 (APC 1.80). Notable racial disparities included a marked increase among American Indian/Alaska Native individuals from 2018–2020 (APC 12.34), followed by Black individuals for the same period (APC 6.30), and a steady rise for White individuals from 2008 to 2020 (APC 2.34). In contrast, Asian/Pacific Islanders saw a decline from 1999 to 2015 (APC -1.81). Geographically, the West had the sharpest recent increase from 2018 to 2021 (APC 9.03), while the South and Midwest demonstrated sustained upward trends beginning in 2008 and 2009, respectively.
Discussion: These findings underscore a growing national burden of cirrhosis-related mortality, particularly among women, American Indian/Alaska Native, and Black populations, and in Western regions, highlighting the need for targeted public health interventions focused on modifiable risk factors such as nonalcoholic fatty liver disease and alcohol use.
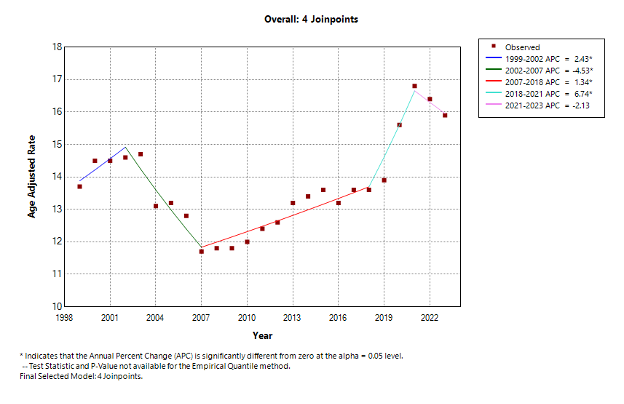
Figure: JoinPoint Model Overall
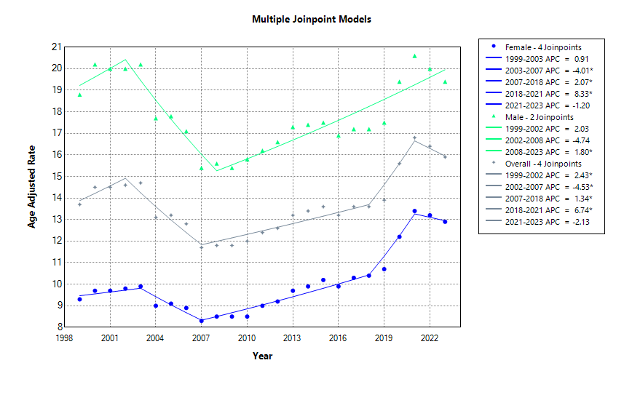
Figure: JoinPoint Model Male vs Female
Disclosures:
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Osman Wafai indicated no relevant financial relationships.
Mujtaba Hyder indicated no relevant financial relationships.
Diksha Kajal indicated no relevant financial relationships.
FNU Murlidhar indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Rahul Kumar, MD1, Avinash Nankani, MBBS2, Osman Wafai, MBBS3, Mujtaba Hyder, MBBS2, Diksha Kajal, MD4, FNU Murlidhar, MBBS, MD5, Karan J.. Yagnik, MD6, Joo Hee Park, MD1, Fnu Vikash, MD7. P3674 - Unveiling Disparities in Liver Cirrhosis–Related Mortality in the United States: A 24-Year Longitudinal Analysis (1999–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

