Tuesday Poster Session
Category: Liver
P6042 - To Transplant or Not to Transplant: A Case of Epithelioid Hemangioendothelioma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Rita Rehana, MD
Henry Ford Health
Royal Oak, MI
Presenting Author(s)
Rita Rehana, MD1, Mohammed Barawi, MD2, Larisa Greenberg, MD3, Rahim Jiwani, MD3
1Henry Ford Health, Royal Oak, MI; 2Henry Ford Health, Detroit, MI; 3Allegheny General Hospital, Pittsburgh, PA
Introduction: Gastrointestinal malignancies encompass different cancers within the digestive tract/related organs and therapies are tailored accordingly. In some instances, liver transplant is a viable option for treatment. One malignancy in particular known as a rare vascular sarcoma called epithelioid hemangioendothelioma (EHE). This vascular tumor arises from the lining of blood vessels and occurs in various tissues and organs. In the liver, it can present as multifocal lesions mimicking metastatic disease or sometimes be misdiagnosed as cirrhosis. Usually, the findings are incidental on imaging. Due to the unpredictability of EHE, patients can experience indolent disease progression, while others suffer from aggressive metastasis or complications. We present a patient with EHE who underwent liver transplant.
Case Description/
Methods: A 72 year old man with presumed cryptogenic cirrhosis, esophageal varices, and lung nodules presented for further evaluation of liver disease. He was found to have abnormal liver biochemistries on routine labs. Comprehensive liver workup was unremarkable. US showed a lobulated liver with multiple areas of heterogeneity. Subsequent MRI showed multiple hepatic masses concerning for malignancy. Recent bidirectional endoscopy reported small esophageal varices and a hyperplastic colon polyp. PET-CT showed innumerable hypermetabolic hypoattenuating hepatic masses concerning for malignancy and multiple pulmonary nodules measuring up to 7 mm. Recommendation was for liver biopsy to establish tissue diagnosis and discuss management at multidisciplinary tumor board. Biopsy showed EHE. Prior MRI was reviewed again with radiology which demonstrated a confluent process with well-defined MRI characteristics of EHE consistent with biopsy results. Standard treatment was for liver transplant due to risks of proliferation of disease with other treatment options. Additional staging with CT chest showed stable small lung nodules. The transplant committee listed the patient as active for transplant. He underwent an uncomplicated deceased donor transplant 12 months later. 1 year posttransplant a surveillance CT showed new and enlarging pulmonary nodules. He underwent wedge resection. Final pathology showed metastatic EHE.
Discussion: Liver transplant remains the primary treatment for localized unresectable EHE. The unpredictable clinical course and variable prognosis underscores the importance of further prospective analysis on EHE and liver transplant.
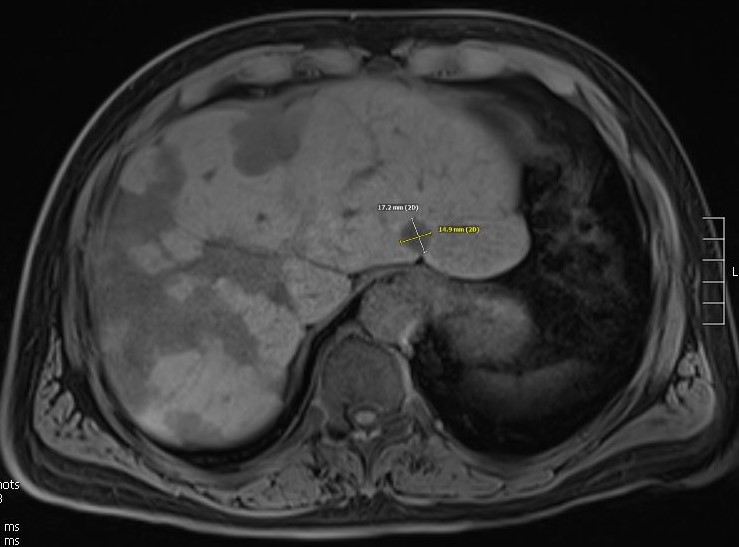
Figure: MRI Liver: Enlarged and macrolobulated although not necessarily cirrhotic in morphology. Subtotal replacement of the liver by multiple mainly centrally necrotic hypointense metastatic lesions. Trace perihepatic ascites.
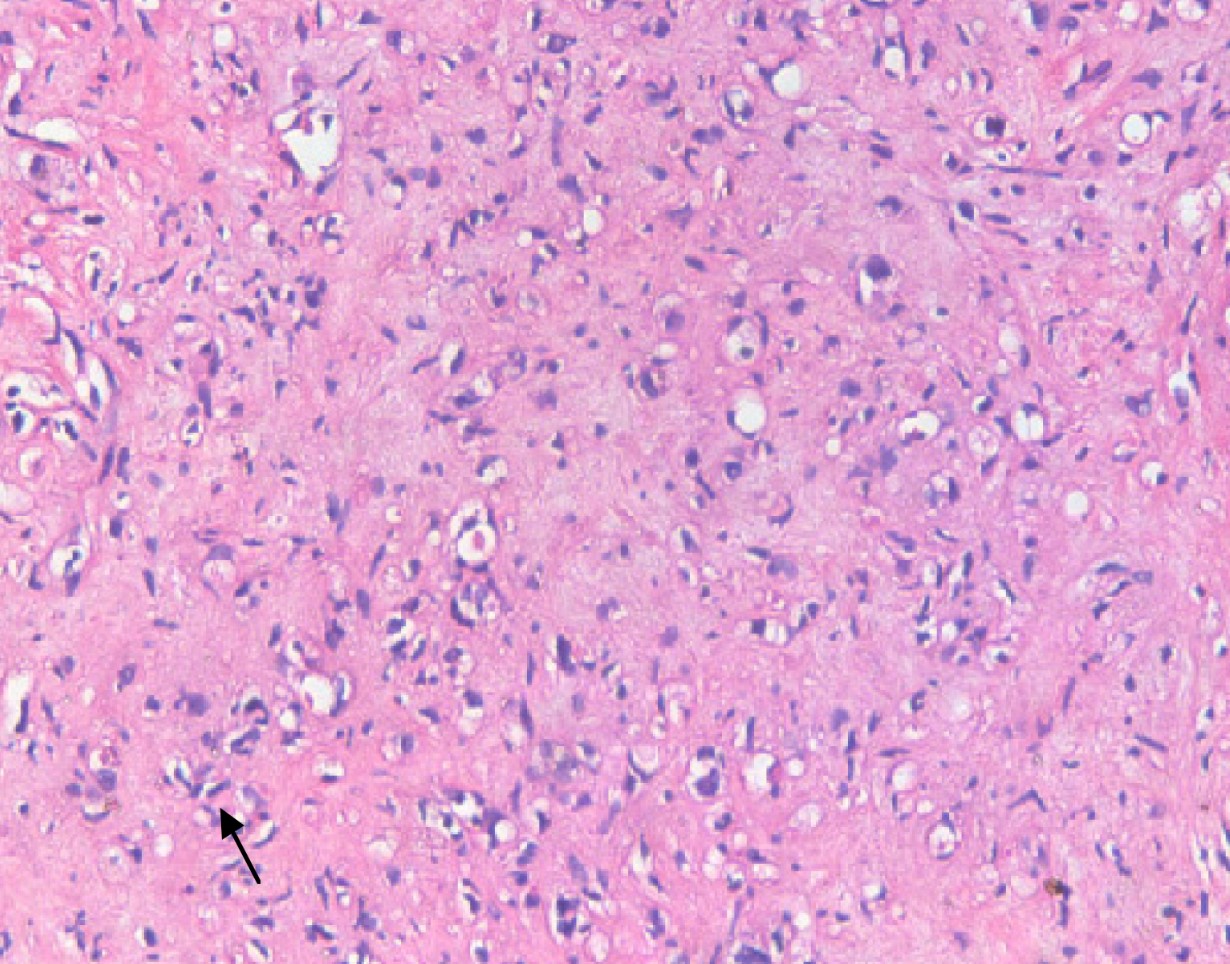
Figure: Liver Pathology: Mildly heteromorphic spindle cells (dendritic cells) with interdigitating processes (hematoxylin and eosin, 200X). Molecular testing revealed a gain of function fusion between WWTR1 and CAMTA1, which is a consistent abnormality in EHE.
Disclosures:
Rita Rehana indicated no relevant financial relationships.
Mohammed Barawi indicated no relevant financial relationships.
Larisa Greenberg indicated no relevant financial relationships.
Rahim Jiwani indicated no relevant financial relationships.
Rita Rehana, MD1, Mohammed Barawi, MD2, Larisa Greenberg, MD3, Rahim Jiwani, MD3. P6042 - To Transplant or Not to Transplant: A Case of Epithelioid Hemangioendothelioma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Royal Oak, MI; 2Henry Ford Health, Detroit, MI; 3Allegheny General Hospital, Pittsburgh, PA
Introduction: Gastrointestinal malignancies encompass different cancers within the digestive tract/related organs and therapies are tailored accordingly. In some instances, liver transplant is a viable option for treatment. One malignancy in particular known as a rare vascular sarcoma called epithelioid hemangioendothelioma (EHE). This vascular tumor arises from the lining of blood vessels and occurs in various tissues and organs. In the liver, it can present as multifocal lesions mimicking metastatic disease or sometimes be misdiagnosed as cirrhosis. Usually, the findings are incidental on imaging. Due to the unpredictability of EHE, patients can experience indolent disease progression, while others suffer from aggressive metastasis or complications. We present a patient with EHE who underwent liver transplant.
Case Description/
Methods: A 72 year old man with presumed cryptogenic cirrhosis, esophageal varices, and lung nodules presented for further evaluation of liver disease. He was found to have abnormal liver biochemistries on routine labs. Comprehensive liver workup was unremarkable. US showed a lobulated liver with multiple areas of heterogeneity. Subsequent MRI showed multiple hepatic masses concerning for malignancy. Recent bidirectional endoscopy reported small esophageal varices and a hyperplastic colon polyp. PET-CT showed innumerable hypermetabolic hypoattenuating hepatic masses concerning for malignancy and multiple pulmonary nodules measuring up to 7 mm. Recommendation was for liver biopsy to establish tissue diagnosis and discuss management at multidisciplinary tumor board. Biopsy showed EHE. Prior MRI was reviewed again with radiology which demonstrated a confluent process with well-defined MRI characteristics of EHE consistent with biopsy results. Standard treatment was for liver transplant due to risks of proliferation of disease with other treatment options. Additional staging with CT chest showed stable small lung nodules. The transplant committee listed the patient as active for transplant. He underwent an uncomplicated deceased donor transplant 12 months later. 1 year posttransplant a surveillance CT showed new and enlarging pulmonary nodules. He underwent wedge resection. Final pathology showed metastatic EHE.
Discussion: Liver transplant remains the primary treatment for localized unresectable EHE. The unpredictable clinical course and variable prognosis underscores the importance of further prospective analysis on EHE and liver transplant.
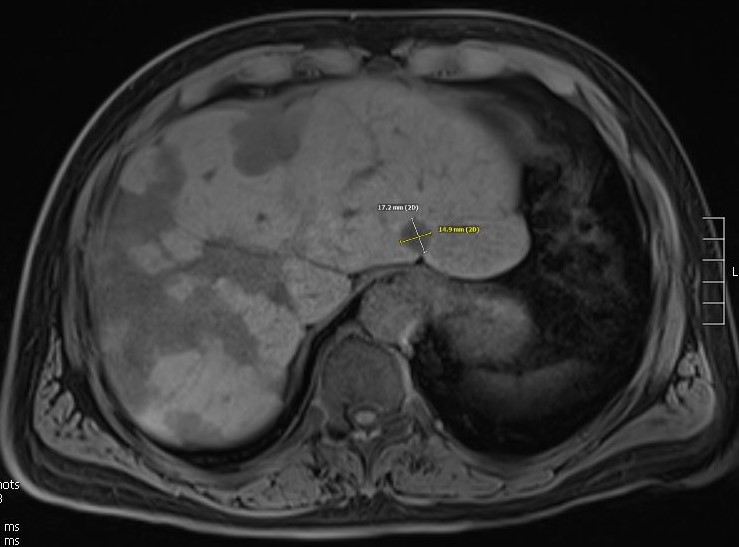
Figure: MRI Liver: Enlarged and macrolobulated although not necessarily cirrhotic in morphology. Subtotal replacement of the liver by multiple mainly centrally necrotic hypointense metastatic lesions. Trace perihepatic ascites.
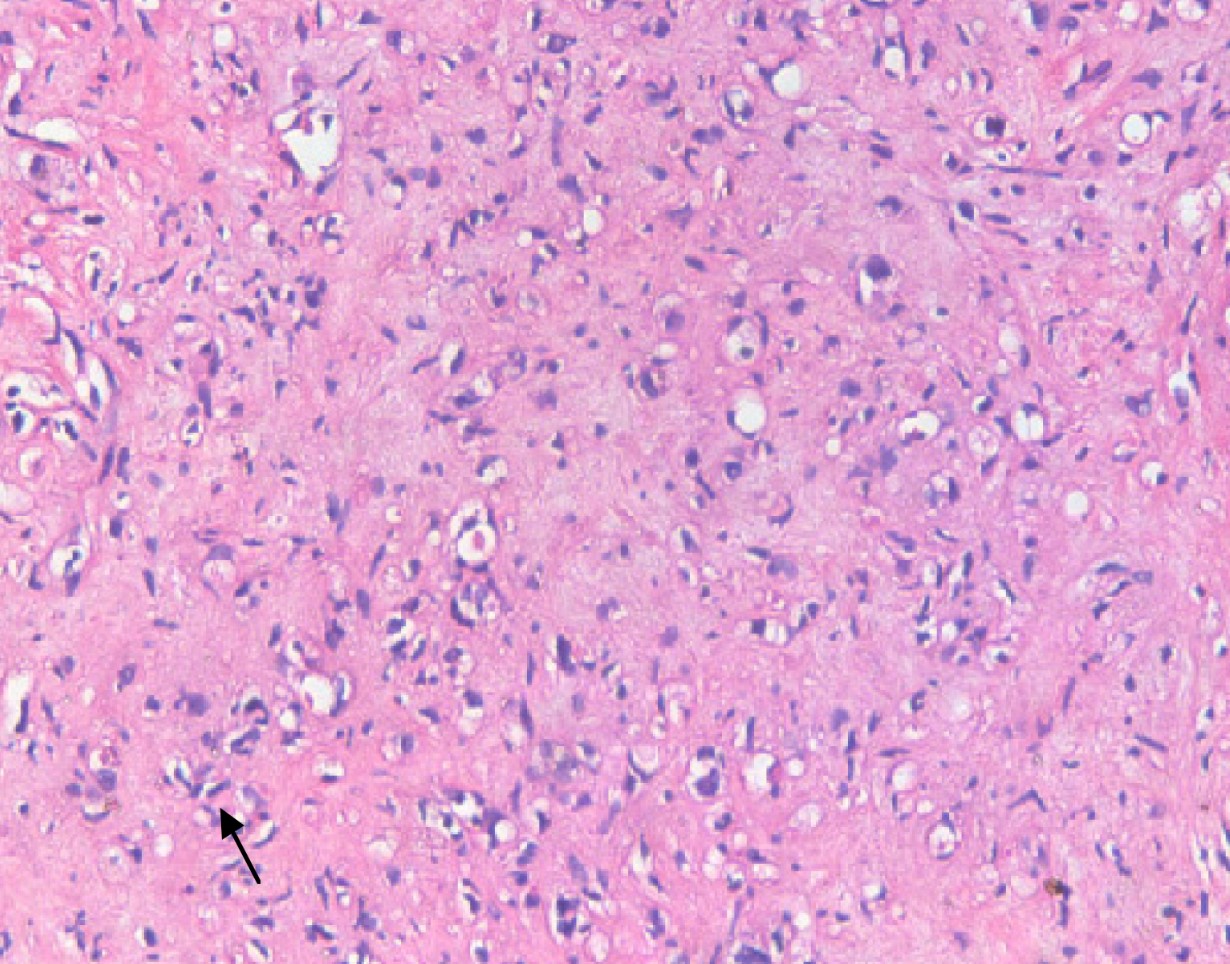
Figure: Liver Pathology: Mildly heteromorphic spindle cells (dendritic cells) with interdigitating processes (hematoxylin and eosin, 200X). Molecular testing revealed a gain of function fusion between WWTR1 and CAMTA1, which is a consistent abnormality in EHE.
Disclosures:
Rita Rehana indicated no relevant financial relationships.
Mohammed Barawi indicated no relevant financial relationships.
Larisa Greenberg indicated no relevant financial relationships.
Rahim Jiwani indicated no relevant financial relationships.
Rita Rehana, MD1, Mohammed Barawi, MD2, Larisa Greenberg, MD3, Rahim Jiwani, MD3. P6042 - To Transplant or Not to Transplant: A Case of Epithelioid Hemangioendothelioma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
