Tuesday Poster Session
Category: Liver
P6041 - Isavuconazonium-Induced Vanishing Bile Duct Syndrome in a Chronic Granulomatous Disease Patient: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ifeoma P. Kwentoh, MD (she/her/hers)
New York Institute of Technology College of Osteopathic Medicine
Kent, CT
Presenting Author(s)
Ifeoma P. Kwentoh, MD1, Mohammed Rifat Shaik, MD2, Theo Heller, MD3
1New York Institute of Technology College of Osteopathic Medicine, Kent, CT; 2National Institutes of Health, Bethesda,, MD; 3National Institutes of Health, Bethesda, MD
Introduction: Vanishing bile duct syndrome (VBDS) is an uncommon, acquired and potentially life-threatening disorder resulting in progressive destruction and loss of small intrahepatic bile ducts. The resultant cholestasis, and progressive biliary cirrhosis usually start off as a complication of acute drug induced liver injury. VBDS can progress to severe loss of >50% of intrahepatic bile ducts and eventual liver failure requiring liver transplantation (LT) or death. We report one of the first few cases of water-soluble form of a prodrug isavuconazonium induced VBDS.
Case Description/
Methods: 40 y/o man with X-linked Chronic Granulomatous Disease (CGD) complicated by recurrent pneumonias and MRSA liver abscess, adrenal insufficiency, dilated cardiomyopathy was admitted with sepsis and pneumonia. Hepatology was consulted for a cholestatic pattern of liver enzyme elevation. Physical exam revealed jaundiced skin and mild right upper quadrant abdominal tenderness. Labs revealed ALT 211 U/L, AST 214 U/L, ALP 4673 U/L and total Bilirubin of 27.3 with direct > 20 mg/dL. At the prior consultation, ALP ranged from 135-306 U/L with normal ALT/AST. He had been on trimethoprim/sulfamethoxazole and hydrocortisone long term but started Isavuconazonium ~1 month prior to ALP peak. Abdominal MRI showed no biliary duct dilation but revealed enlarged portal vein and splenomegaly (Image). Work up for viral and autoimmune etiologies for liver disease was unrevealing. Liver biopsy confirmed findings of acute cholestatic hepatitis with severe ductopenia, pigmented Kuffer cells (consistent with known CGD), other immune mediated injury with recent infection and low T cell count. Clinical presentation and histology were in keeping with VBDS confirmed by duct paucity and biliary metaplasia on CK7 immunostain.
Discussion: VBDS can develop following an episode of severe cholestatic hepatitis as seen in our case, and often the duct destruction and injury progress despite discontinuing the offending medication. The syndrome generally manifests within 1 to 6 months of initial injury. Patients are mostly asymptomatic and discovered incidentally based on elevated liver enzymes, or may be symptomatic with pruritus, fatigue and jaundice in cases of severe cholestatic hepatitis. Biopsy is confirmatory. Management remains challenging with LT as the only definitive treatment. The NIH maintains an updated, unbiased database of medications known to cause VBDS. This may be the first reported case of VBDS due to isavuconazonium, an antifungal agent.
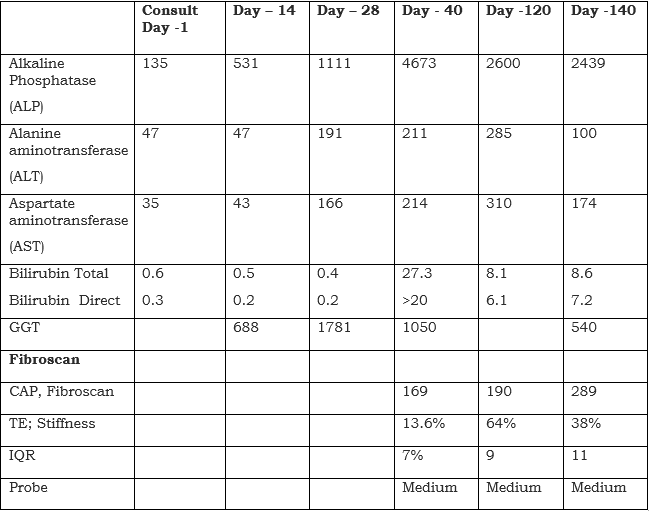
Figure: Liver associated enzyme weekly trend during admission and routine follow up
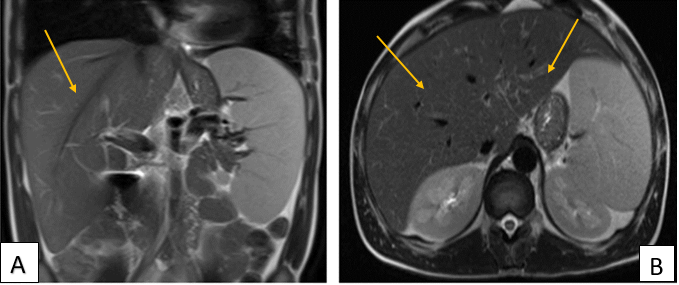
Figure: Fig A and B -T2 weighted image Abdominal MRI that does not show any alteration of caliber of the intrahepatic ducts (Yellow arrows).
Disclosures:
Ifeoma Kwentoh indicated no relevant financial relationships.
Mohammed Rifat Shaik indicated no relevant financial relationships.
Theo Heller indicated no relevant financial relationships.
Ifeoma P. Kwentoh, MD1, Mohammed Rifat Shaik, MD2, Theo Heller, MD3. P6041 - Isavuconazonium-Induced Vanishing Bile Duct Syndrome in a Chronic Granulomatous Disease Patient: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Institute of Technology College of Osteopathic Medicine, Kent, CT; 2National Institutes of Health, Bethesda,, MD; 3National Institutes of Health, Bethesda, MD
Introduction: Vanishing bile duct syndrome (VBDS) is an uncommon, acquired and potentially life-threatening disorder resulting in progressive destruction and loss of small intrahepatic bile ducts. The resultant cholestasis, and progressive biliary cirrhosis usually start off as a complication of acute drug induced liver injury. VBDS can progress to severe loss of >50% of intrahepatic bile ducts and eventual liver failure requiring liver transplantation (LT) or death. We report one of the first few cases of water-soluble form of a prodrug isavuconazonium induced VBDS.
Case Description/
Methods: 40 y/o man with X-linked Chronic Granulomatous Disease (CGD) complicated by recurrent pneumonias and MRSA liver abscess, adrenal insufficiency, dilated cardiomyopathy was admitted with sepsis and pneumonia. Hepatology was consulted for a cholestatic pattern of liver enzyme elevation. Physical exam revealed jaundiced skin and mild right upper quadrant abdominal tenderness. Labs revealed ALT 211 U/L, AST 214 U/L, ALP 4673 U/L and total Bilirubin of 27.3 with direct > 20 mg/dL. At the prior consultation, ALP ranged from 135-306 U/L with normal ALT/AST. He had been on trimethoprim/sulfamethoxazole and hydrocortisone long term but started Isavuconazonium ~1 month prior to ALP peak. Abdominal MRI showed no biliary duct dilation but revealed enlarged portal vein and splenomegaly (Image). Work up for viral and autoimmune etiologies for liver disease was unrevealing. Liver biopsy confirmed findings of acute cholestatic hepatitis with severe ductopenia, pigmented Kuffer cells (consistent with known CGD), other immune mediated injury with recent infection and low T cell count. Clinical presentation and histology were in keeping with VBDS confirmed by duct paucity and biliary metaplasia on CK7 immunostain.
Discussion: VBDS can develop following an episode of severe cholestatic hepatitis as seen in our case, and often the duct destruction and injury progress despite discontinuing the offending medication. The syndrome generally manifests within 1 to 6 months of initial injury. Patients are mostly asymptomatic and discovered incidentally based on elevated liver enzymes, or may be symptomatic with pruritus, fatigue and jaundice in cases of severe cholestatic hepatitis. Biopsy is confirmatory. Management remains challenging with LT as the only definitive treatment. The NIH maintains an updated, unbiased database of medications known to cause VBDS. This may be the first reported case of VBDS due to isavuconazonium, an antifungal agent.
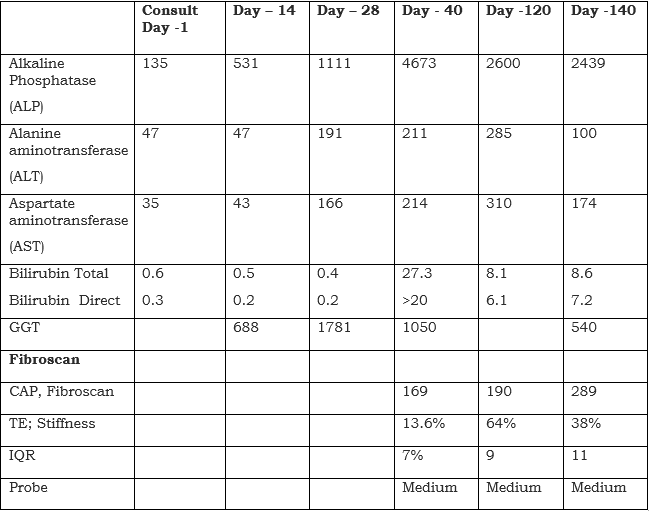
Figure: Liver associated enzyme weekly trend during admission and routine follow up
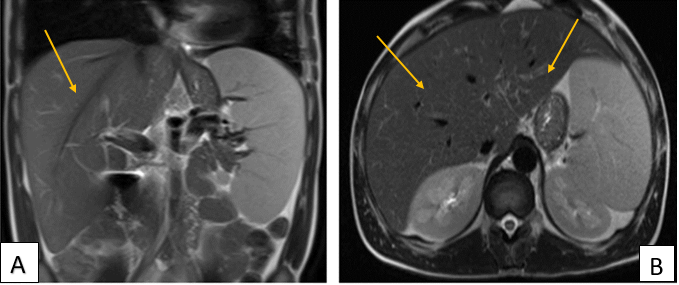
Figure: Fig A and B -T2 weighted image Abdominal MRI that does not show any alteration of caliber of the intrahepatic ducts (Yellow arrows).
Disclosures:
Ifeoma Kwentoh indicated no relevant financial relationships.
Mohammed Rifat Shaik indicated no relevant financial relationships.
Theo Heller indicated no relevant financial relationships.
Ifeoma P. Kwentoh, MD1, Mohammed Rifat Shaik, MD2, Theo Heller, MD3. P6041 - Isavuconazonium-Induced Vanishing Bile Duct Syndrome in a Chronic Granulomatous Disease Patient: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
