Tuesday Poster Session
Category: Liver
P6036 - Diagnostic Masquerade: Cryptococcal Meningitis Unveiling as Altered Mental Status in Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rhett Harmon, MD (he/him/his)
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Rhett Harmon, MD1, Sherif Shoucri, MD2, Shaun Chandna, DO2
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Cryptococcal meningitis (CM) is a life-threatening infection primarily seen in immunocompromised individuals. Patients with cirrhosis are immunocompromised due to impaired immune function predisposing to opportunistic infections. High mortality with CM necessitates early diagnosis and management. Differentiating cryptococcal meningitis from hepatic encephalopathy (HE) in cirrhosis represents an uncommon yet important diagnostic challenge.
Case Description/
Methods: A 37-year-old male with alcohol associated cirrhosis decompensated by HE and ascites presented to the emergency department with acute encephalopathy, managed as HE with lactulose and rifaximin. Paracentesis was negative for spontaneous bacterial peritonitis. Minimal improvement was seen despite adequate bowel movements on HE treatment. New left-sided headache and neck pain on Day 6 prompted CT head revealing multifocal subcortical hypodensities and ventriculomegaly. Lumbar puncture (LP) was performed and returned positive for Cryptococcus neoformans by PCR and culture, despite negative serum cryptococcal antigen (CrAg) testing. Antifungal therapy was initiated. The patient unfortunately developed a cerebellar infarct, likely due to Cryptococcal meningitis related vasculitis. Due to further clinical deterioration, the patient was transitioned to comfort care.
Discussion: Cryptococcal meningitis diagnosis in cirrhosis can be challenging due to the clinical presentation's overlap with HE. Infection and alternative etiologies should be sought in potential cases of HE. CM classically includes headache, altered mentation, and focal neurological findings. Serum CrAg testing is less sensitive in diagnosing CM in patients without HIV. Falsely negative results can be due to the prozone (Hook) effect, and in cases with subcapsular or acapsular subspecies of Cryptococcus. A high index of suspicion for fungal meningitis with early imaging, serum testing, confirmatory diagnostics with LP and cryptococcal cerebrospinal fluid PCR testing, and prompt antifungal treatment is necessary in cirrhotic patients with neurological symptoms to improve outcomes. Clinicians should be aware of CM in the differential of cirrhosis with altered mentation.
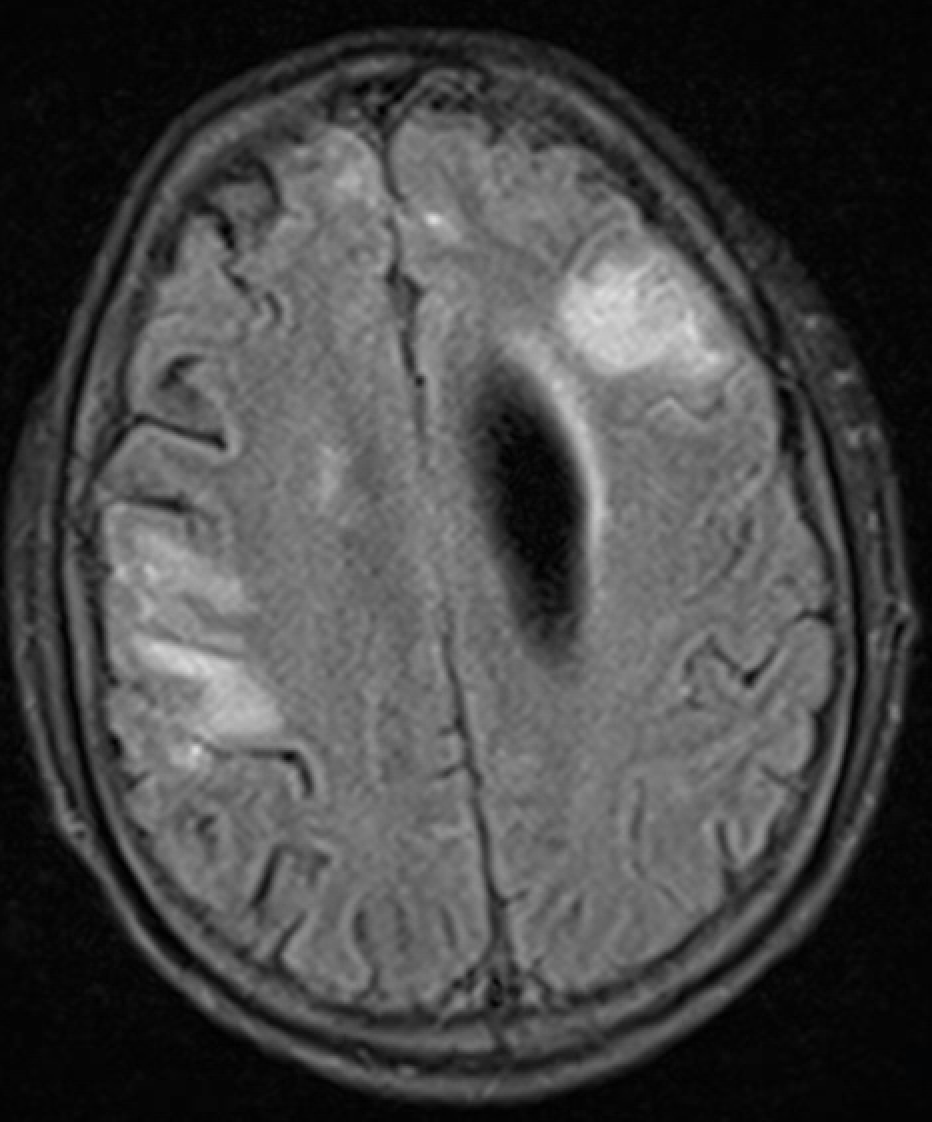
Figure: Cluster of enhancing lesions in the left frontal lobe and scattered
tiny enhancing lesions in the bilateral cerebral hemispheres.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Sherif Shoucri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Sherif Shoucri, MD2, Shaun Chandna, DO2. P6036 - Diagnostic Masquerade: Cryptococcal Meningitis Unveiling as Altered Mental Status in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Cryptococcal meningitis (CM) is a life-threatening infection primarily seen in immunocompromised individuals. Patients with cirrhosis are immunocompromised due to impaired immune function predisposing to opportunistic infections. High mortality with CM necessitates early diagnosis and management. Differentiating cryptococcal meningitis from hepatic encephalopathy (HE) in cirrhosis represents an uncommon yet important diagnostic challenge.
Case Description/
Methods: A 37-year-old male with alcohol associated cirrhosis decompensated by HE and ascites presented to the emergency department with acute encephalopathy, managed as HE with lactulose and rifaximin. Paracentesis was negative for spontaneous bacterial peritonitis. Minimal improvement was seen despite adequate bowel movements on HE treatment. New left-sided headache and neck pain on Day 6 prompted CT head revealing multifocal subcortical hypodensities and ventriculomegaly. Lumbar puncture (LP) was performed and returned positive for Cryptococcus neoformans by PCR and culture, despite negative serum cryptococcal antigen (CrAg) testing. Antifungal therapy was initiated. The patient unfortunately developed a cerebellar infarct, likely due to Cryptococcal meningitis related vasculitis. Due to further clinical deterioration, the patient was transitioned to comfort care.
Discussion: Cryptococcal meningitis diagnosis in cirrhosis can be challenging due to the clinical presentation's overlap with HE. Infection and alternative etiologies should be sought in potential cases of HE. CM classically includes headache, altered mentation, and focal neurological findings. Serum CrAg testing is less sensitive in diagnosing CM in patients without HIV. Falsely negative results can be due to the prozone (Hook) effect, and in cases with subcapsular or acapsular subspecies of Cryptococcus. A high index of suspicion for fungal meningitis with early imaging, serum testing, confirmatory diagnostics with LP and cryptococcal cerebrospinal fluid PCR testing, and prompt antifungal treatment is necessary in cirrhotic patients with neurological symptoms to improve outcomes. Clinicians should be aware of CM in the differential of cirrhosis with altered mentation.
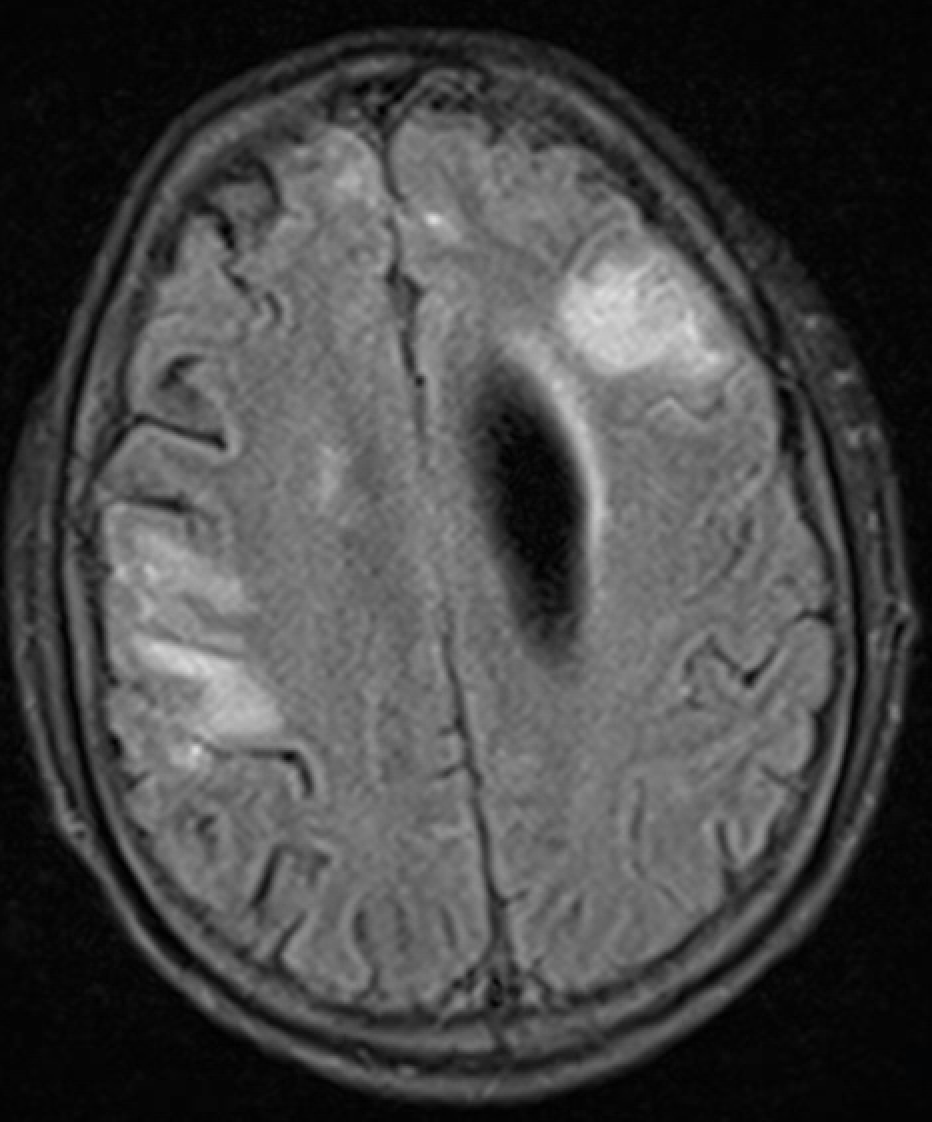
Figure: Cluster of enhancing lesions in the left frontal lobe and scattered
tiny enhancing lesions in the bilateral cerebral hemispheres.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Sherif Shoucri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Sherif Shoucri, MD2, Shaun Chandna, DO2. P6036 - Diagnostic Masquerade: Cryptococcal Meningitis Unveiling as Altered Mental Status in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
