Tuesday Poster Session
Category: Liver
P6035 - Rapidly Progressive Vanishing Bile Duct Syndrome in Classical Hodgkin Lymphoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rhett Harmon, MD (he/him/his)
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Rhett Harmon, MD1, Andrew Gregg, MD2, Payman Fathizadeh, MD3, Deepthi Karunasiri, MD3, Simon Beaven, MD, PhD3, Shaun Chandna, DO3
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Vanishing bile duct syndrome (VBDS) is a severe condition characterized by progressive loss of intrahepatic bile ducts resulting in cholestatic liver injury and possible liver failure. Although VBDS may result from drug reactions, infections, and autoimmune diseases, its association with lymphoproliferative disorders comes with particular diagnostic and management challenges. In patients with Hodgkin lymphoma (HL), VBDS may present as a paraneoplastic phenomenon or develop as a consequence of therapy; however, early recognition is important as the condition is likely to progress rapidly despite intervention.
Case Description/
Methods: 31-year-old previously healthy male presented with 4 months of progressive left cervical lymphadenopathy and 10-day history of diffuse abdominal pain. Labs revealed cholestatic pattern of liver injury. Cervical lymph node biopsy confirmed classic Hodgkin lymphoma of nodular sclerosis type. MRCP revealed a patent biliary tree. Initial liver tests included an elevated INR 1.6, AST 214, ALT 182, total bilirubin 18, and alkaline phosphatase 403 which worsened with progressive cholestasis despite initiation of chemotherapy including cyclophosphamide and dexamethasone. Liver biopsy revealed ductopenia over 50% of portal tracts, consistent with VBDS. No histologic evidence of direct lymphomatous invasion or other causes of liver injury, such as viral hepatitis or autoimmune processes, were found on work up. Due to rapid deterioration and limited response to standard lymphoma therapy, the patient was transferred for liver transplant evaluation.
Discussion: Vanishing bile duct syndrome is a difficult diagnosis necessitating liver biopsy to confirm the absence of bile ducts. This condition can be linked to Hodgkin lymphoma, where it may appear as a paraneoplastic syndrome. Pathophysiology is complex, involving autoimmune, inflammatory, and regenerative factors which play a role in bile duct destruction though precise mechanisms are unclear. Treatment with corticosteroids and ursodeoxycholic acid may reduce inflammation and stimulate bile secretion, preventing apoptosis of cholangiocytes. Liver transplantation is reserved for advanced or refractory cases. When VBDS is associated with HL, treating the lymphoma may lead to improvement in some patients. This rare disease and its variable presentation contribute to ongoing difficulties in early diagnosis and effective management.
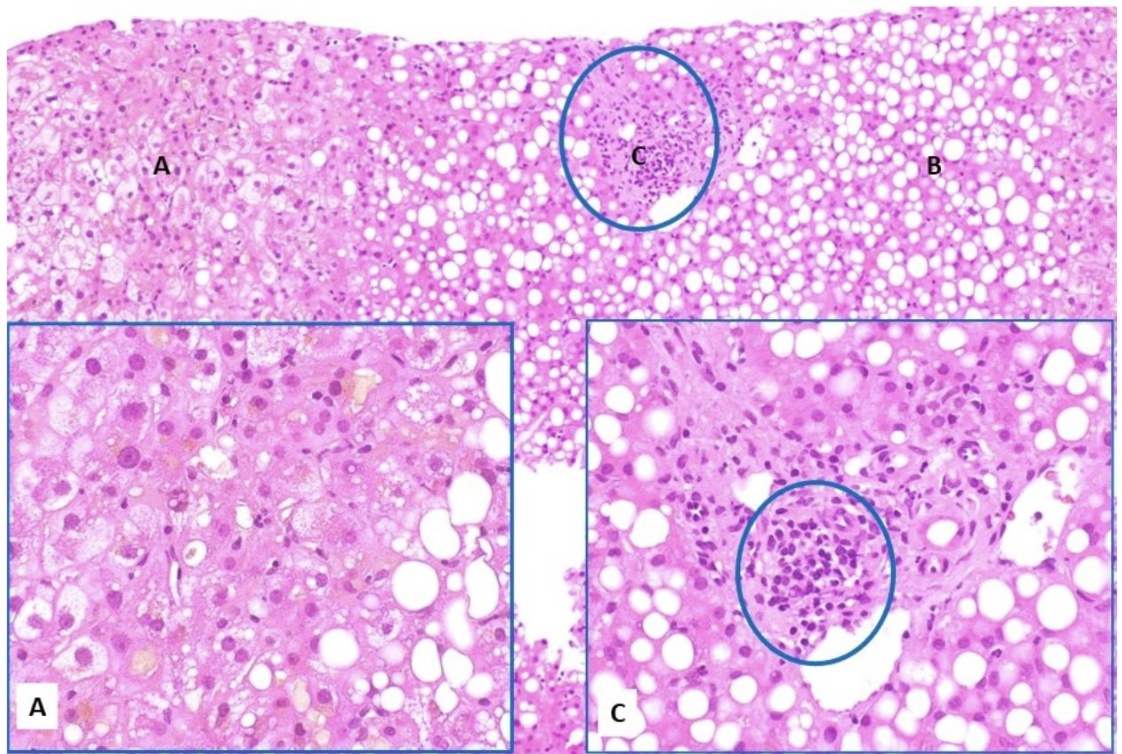
Figure: Liver core biopsies demonstrate canalicular cholestasis (A), approximately 70% macrovesicular steatosis (B), and significant bile duct loss (C). The few remaining bile ducts exhibit evidence of injury and degenerative changes. These histologic findings are consistent with ductopenia/vanishing bile duct syndrome, which may be associated with drug-induced liver injury or the patient's documented history of Hodgkin lymphoma. The concurrent macrovesicular steatosis may also represent a manifestation of drug-related hepatotoxicity. No evidence of lymphomatous infiltration is identified. The histologic features do not suggest extrahepatic biliary obstruction.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Andrew Gregg indicated no relevant financial relationships.
Payman Fathizadeh indicated no relevant financial relationships.
Deepthi Karunasiri indicated no relevant financial relationships.
Simon Beaven: Alnylam – Speakers Bureau.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Andrew Gregg, MD2, Payman Fathizadeh, MD3, Deepthi Karunasiri, MD3, Simon Beaven, MD, PhD3, Shaun Chandna, DO3. P6035 - Rapidly Progressive Vanishing Bile Duct Syndrome in Classical Hodgkin Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Vanishing bile duct syndrome (VBDS) is a severe condition characterized by progressive loss of intrahepatic bile ducts resulting in cholestatic liver injury and possible liver failure. Although VBDS may result from drug reactions, infections, and autoimmune diseases, its association with lymphoproliferative disorders comes with particular diagnostic and management challenges. In patients with Hodgkin lymphoma (HL), VBDS may present as a paraneoplastic phenomenon or develop as a consequence of therapy; however, early recognition is important as the condition is likely to progress rapidly despite intervention.
Case Description/
Methods: 31-year-old previously healthy male presented with 4 months of progressive left cervical lymphadenopathy and 10-day history of diffuse abdominal pain. Labs revealed cholestatic pattern of liver injury. Cervical lymph node biopsy confirmed classic Hodgkin lymphoma of nodular sclerosis type. MRCP revealed a patent biliary tree. Initial liver tests included an elevated INR 1.6, AST 214, ALT 182, total bilirubin 18, and alkaline phosphatase 403 which worsened with progressive cholestasis despite initiation of chemotherapy including cyclophosphamide and dexamethasone. Liver biopsy revealed ductopenia over 50% of portal tracts, consistent with VBDS. No histologic evidence of direct lymphomatous invasion or other causes of liver injury, such as viral hepatitis or autoimmune processes, were found on work up. Due to rapid deterioration and limited response to standard lymphoma therapy, the patient was transferred for liver transplant evaluation.
Discussion: Vanishing bile duct syndrome is a difficult diagnosis necessitating liver biopsy to confirm the absence of bile ducts. This condition can be linked to Hodgkin lymphoma, where it may appear as a paraneoplastic syndrome. Pathophysiology is complex, involving autoimmune, inflammatory, and regenerative factors which play a role in bile duct destruction though precise mechanisms are unclear. Treatment with corticosteroids and ursodeoxycholic acid may reduce inflammation and stimulate bile secretion, preventing apoptosis of cholangiocytes. Liver transplantation is reserved for advanced or refractory cases. When VBDS is associated with HL, treating the lymphoma may lead to improvement in some patients. This rare disease and its variable presentation contribute to ongoing difficulties in early diagnosis and effective management.
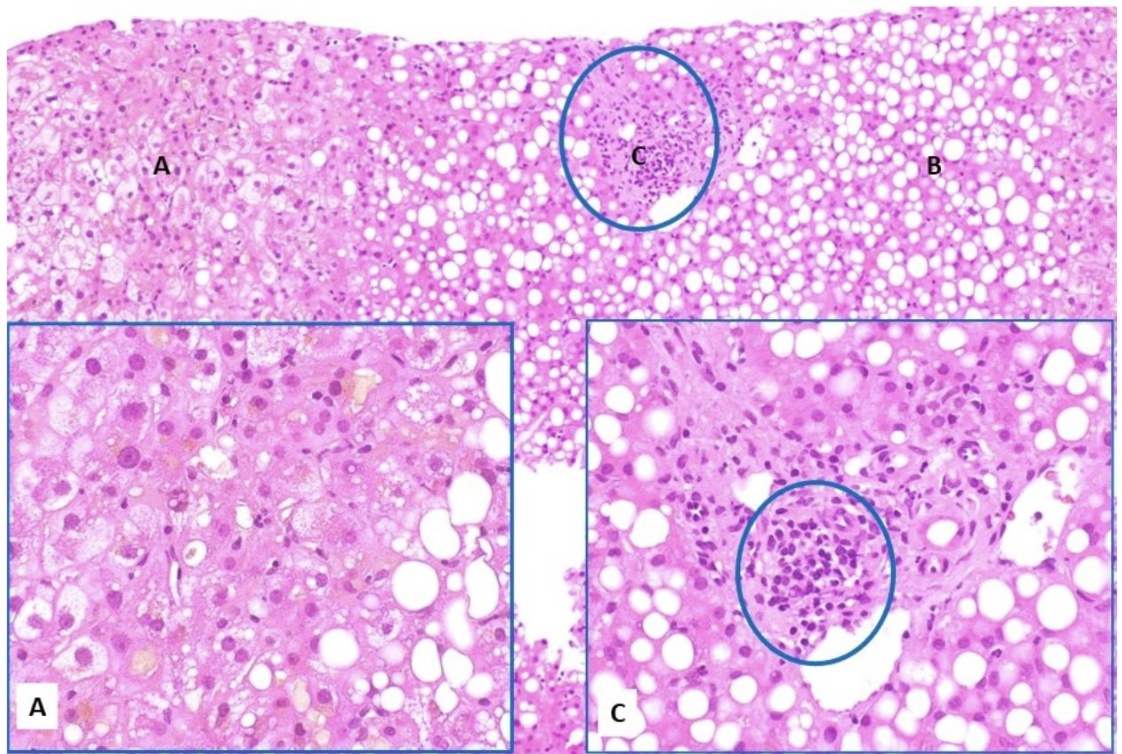
Figure: Liver core biopsies demonstrate canalicular cholestasis (A), approximately 70% macrovesicular steatosis (B), and significant bile duct loss (C). The few remaining bile ducts exhibit evidence of injury and degenerative changes. These histologic findings are consistent with ductopenia/vanishing bile duct syndrome, which may be associated with drug-induced liver injury or the patient's documented history of Hodgkin lymphoma. The concurrent macrovesicular steatosis may also represent a manifestation of drug-related hepatotoxicity. No evidence of lymphomatous infiltration is identified. The histologic features do not suggest extrahepatic biliary obstruction.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Andrew Gregg indicated no relevant financial relationships.
Payman Fathizadeh indicated no relevant financial relationships.
Deepthi Karunasiri indicated no relevant financial relationships.
Simon Beaven: Alnylam – Speakers Bureau.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Andrew Gregg, MD2, Payman Fathizadeh, MD3, Deepthi Karunasiri, MD3, Simon Beaven, MD, PhD3, Shaun Chandna, DO3. P6035 - Rapidly Progressive Vanishing Bile Duct Syndrome in Classical Hodgkin Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
