Tuesday Poster Session
Category: Liver
P6033 - From Mystery to Clarity: A Case of a Neuroendocrine G-NET Mimicking Adenocarcinoma on Esophagogastroduodenoscopy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

McKenna Andrews, MD
East Tennessee State University
Kingsport, TN
Presenting Author(s)
McKenna Andrews, MD1, David W. Berry, DO2, Usama Abu-Heija, MBBS2, Noah Hall, MD3
1East Tennessee State University, Kingsport, TN; 2East Tennessee State University, Johnson City, TN; 3Mountain Home VA Medical Center, Jonesborough, TN
Introduction: Gastric neuroendocrine tumors (G-NETs) are rare neoplasms originating from enterochromaffin-like cells in the gastric mucosa. While often small and asymptomatic, some G-NETs can present with aggressive behavior and mimic more common malignancies such as gastric adenocarcinoma. G-NETs are classified into types I, II, and III based on clinical features and underlying pathophysiology. Accurate diagnosis depends on histopathology and immunohistochemistry.
Case Description/
Methods: A 72-year-old male with a history of prostate cancer, type II diabetes, and prior alcohol use presented with fatigue, anorexia, and melena. CT imaging revealed an ulcerated gastric mass and extensive liver metastases. Esophagogastroduodenoscopy demonstrated a 3–4 cm ulcerated, infiltrative mass in the gastric body, raising suspicion for gastric adenocarcinoma based on gross morphology (Image 1). However, biopsy revealed a well-differentiated neuroendocrine tumor (NET) characterized by trabecular architecture, round to oval nuclei, and moderate cytoplasm. Giemsa stain was negative for H. pylori. A targeted liver lesion biopsy confirmed metastatic NET of the same histology.
Laboratory evaluation revealed hemoglobin of 9.6 g/dL, elevated serum gastrin at 1432 pg/mL, and urinary 5-HIAA of 2.4 mg/24 hrs. Despite hypergastrinemia, histology did not show chronic atrophic gastritis, arguing against type I or II G-NETs. After holding proton pump inhibitor (PPI) therapy, repeat serum gastrin decreased to 312 pg/mL, and the pH of gastric aspirate was 4.0—findings that do not support Zollinger-Ellison syndrome (ZE). The absence of gastric atrophy, lack of MEN1/ZE, and presence of metastatic disease supported a diagnosis of type III G-NET, a sporadic, gastrin-independent subtype with more aggressive behavior. Nuclear Medicine Positron Emission Tomography Computed Tomography (NM PET-CT) showed multiple areas of somatostatin receptor overexpression (Image 2).
Discussion: This case illustrates the diagnostic challenge of G-NETs, which may visually mimic adenocarcinoma on endoscopy. Type III G-NETs often present as large, ulcerated lesions with early metastatic spread and carry the worst prognosis among G-NETs. In contrast, type I G-NETs are associated with autoimmune atrophic gastritis and hypergastrinemia, typically presenting as small lesions with low malignant potential. Type II G-NETs occur in the setting of MEN1 and Zollinger-Ellison syndrome, also associated with hypergastrinemia but with intermediate malignant potential.

Figure: Image 1. EGD revealing 3-4 cm ulcerated mass in the gastric body with mild oozing.
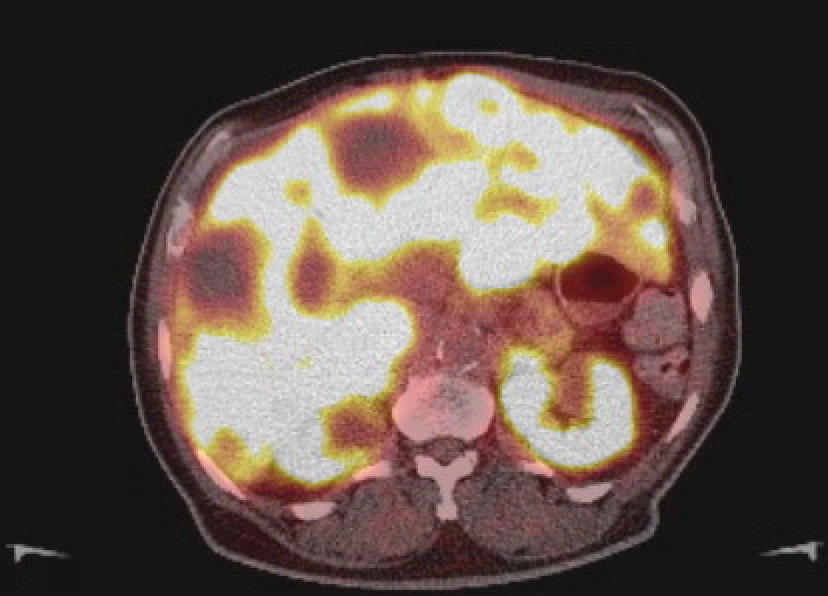
Figure: Image 2. NM PET CT showing innumerable, largely low-attenuation hepatic foci. Innumerable, smaller, non-measurable hepatic foci show somatostatin receptor overexpression consistent with metastasis.
Disclosures:
McKenna Andrews indicated no relevant financial relationships.
David Berry indicated no relevant financial relationships.
Usama Abu-Heija indicated no relevant financial relationships.
Noah Hall indicated no relevant financial relationships.
McKenna Andrews, MD1, David W. Berry, DO2, Usama Abu-Heija, MBBS2, Noah Hall, MD3. P6033 - From Mystery to Clarity: A Case of a Neuroendocrine G-NET Mimicking Adenocarcinoma on Esophagogastroduodenoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Tennessee State University, Kingsport, TN; 2East Tennessee State University, Johnson City, TN; 3Mountain Home VA Medical Center, Jonesborough, TN
Introduction: Gastric neuroendocrine tumors (G-NETs) are rare neoplasms originating from enterochromaffin-like cells in the gastric mucosa. While often small and asymptomatic, some G-NETs can present with aggressive behavior and mimic more common malignancies such as gastric adenocarcinoma. G-NETs are classified into types I, II, and III based on clinical features and underlying pathophysiology. Accurate diagnosis depends on histopathology and immunohistochemistry.
Case Description/
Methods: A 72-year-old male with a history of prostate cancer, type II diabetes, and prior alcohol use presented with fatigue, anorexia, and melena. CT imaging revealed an ulcerated gastric mass and extensive liver metastases. Esophagogastroduodenoscopy demonstrated a 3–4 cm ulcerated, infiltrative mass in the gastric body, raising suspicion for gastric adenocarcinoma based on gross morphology (Image 1). However, biopsy revealed a well-differentiated neuroendocrine tumor (NET) characterized by trabecular architecture, round to oval nuclei, and moderate cytoplasm. Giemsa stain was negative for H. pylori. A targeted liver lesion biopsy confirmed metastatic NET of the same histology.
Laboratory evaluation revealed hemoglobin of 9.6 g/dL, elevated serum gastrin at 1432 pg/mL, and urinary 5-HIAA of 2.4 mg/24 hrs. Despite hypergastrinemia, histology did not show chronic atrophic gastritis, arguing against type I or II G-NETs. After holding proton pump inhibitor (PPI) therapy, repeat serum gastrin decreased to 312 pg/mL, and the pH of gastric aspirate was 4.0—findings that do not support Zollinger-Ellison syndrome (ZE). The absence of gastric atrophy, lack of MEN1/ZE, and presence of metastatic disease supported a diagnosis of type III G-NET, a sporadic, gastrin-independent subtype with more aggressive behavior. Nuclear Medicine Positron Emission Tomography Computed Tomography (NM PET-CT) showed multiple areas of somatostatin receptor overexpression (Image 2).
Discussion: This case illustrates the diagnostic challenge of G-NETs, which may visually mimic adenocarcinoma on endoscopy. Type III G-NETs often present as large, ulcerated lesions with early metastatic spread and carry the worst prognosis among G-NETs. In contrast, type I G-NETs are associated with autoimmune atrophic gastritis and hypergastrinemia, typically presenting as small lesions with low malignant potential. Type II G-NETs occur in the setting of MEN1 and Zollinger-Ellison syndrome, also associated with hypergastrinemia but with intermediate malignant potential.

Figure: Image 1. EGD revealing 3-4 cm ulcerated mass in the gastric body with mild oozing.
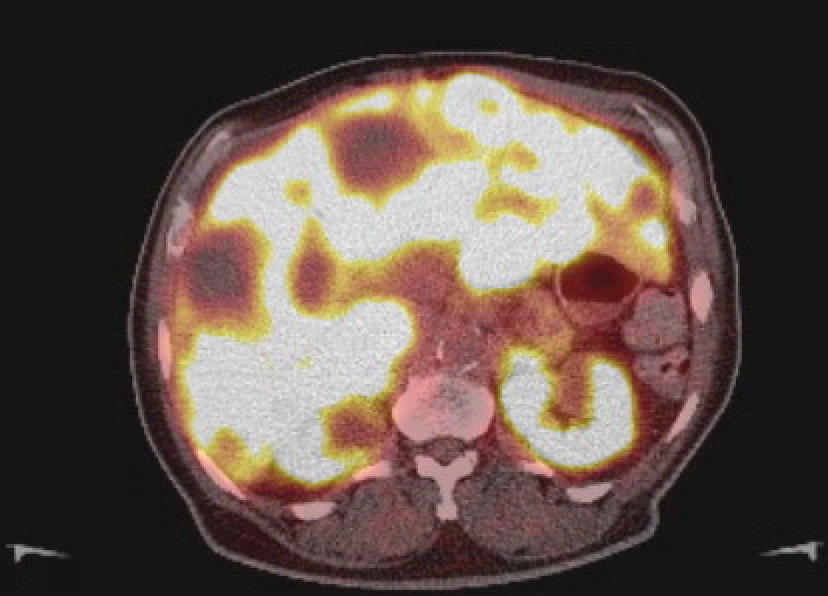
Figure: Image 2. NM PET CT showing innumerable, largely low-attenuation hepatic foci. Innumerable, smaller, non-measurable hepatic foci show somatostatin receptor overexpression consistent with metastasis.
Disclosures:
McKenna Andrews indicated no relevant financial relationships.
David Berry indicated no relevant financial relationships.
Usama Abu-Heija indicated no relevant financial relationships.
Noah Hall indicated no relevant financial relationships.
McKenna Andrews, MD1, David W. Berry, DO2, Usama Abu-Heija, MBBS2, Noah Hall, MD3. P6033 - From Mystery to Clarity: A Case of a Neuroendocrine G-NET Mimicking Adenocarcinoma on Esophagogastroduodenoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
