Tuesday Poster Session
Category: Liver
P6031 - Liver's Backdoor Intrusion: A Rare Case of Hepatogastric Fistula
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Samuel Cheong, DO
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Samuel Cheong, DO1, Sabrina Ho, MD1, Mohamad Omar Diab, MD2, Franklin Liu, MD3, Natasha Khona, DO1, Brandon Witten, MD1, Rolando J. Leal, MD4
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3University of Arizona College of Medicine, Tucson, AZ; 4Banner University Medical Center, Tucson, AZ
Introduction: Hepatocellular carcinoma (HCC) is the most common primary liver cancer. It most commonly metastasizes to the lungs, followed by regional lymph nodes and then bones. Metastasis to the gastrointestinal (GI) tract is rare, occurring in 0.5% to 2% of patients. We present a case of a hepatogastric fistula caused by HCC, likely secondary to Y-90 embolization.
Case Description/
Methods: A 60-year-old male with a history of cirrhosis secondary to MASH complicated by HCC, status post Y-90 radioembolization to segments II and III, and grade III esophageal varices status post banding, presented to the hospital with hematochezia and a hemoglobin (Hgb) of 6.8 g/dL on outpatient labs (baseline 8.0–10.0 g/dL). In the emergency department, repeat labs showed an Hgb of 7.3 g/dL, for which the patient received 1 unit of packed red blood cells. CT angiography (CTA) of the abdomen and pelvis revealed air foci within the previously treated liver cavity with tethering to the stomach, raising concern for a hepatogastric fistula.
EGD revealed grade II medium-sized esophageal varices with red wale signs, as well as two non-bleeding, cratered gastric ulcers concerning for fistulas, which were closed with Ovesco clips. He was subsequently discharged. A month later, he returned with shortness of breath and an outpatient Hgb of 5.5 g/dL. EGD showed similar findings, but the previously placed clips were no longer intact. Attempts to re-close the fistulous openings were unsuccessful due to tissue friability. Biopsies confirmed hepatocellular carcinoma with background gastric ulceration and necrosis. The patient was discharged with close multidisciplinary team follow-up. He was deemed unfit for surgery or liver transplantation and was initiated on systemic therapy with lenvatinib.
Discussion: The predisposing factors for HCC metastasis to the GI tract remain poorly defined due to its rarity. However, proposed risk factors include an exophytic growth pattern, larger tumor size ( >5 cm), and subcapsular location, particularly in the left lobe. Additionally, several reports suggest that loco-regional treatments such as Y-90 radio-embolization or trans-arterial chemo-embolization (TACE) may provoke an inflammatory response in adjacent GI structures, facilitating tumor invasion. HCC may also reach the GI tract via hematogenous spread, in which tumor thrombi enter the portal venous system and disseminate through hepatofugal flow. This case highlights a rare complication of loco-regional treatments in patients with HCC.
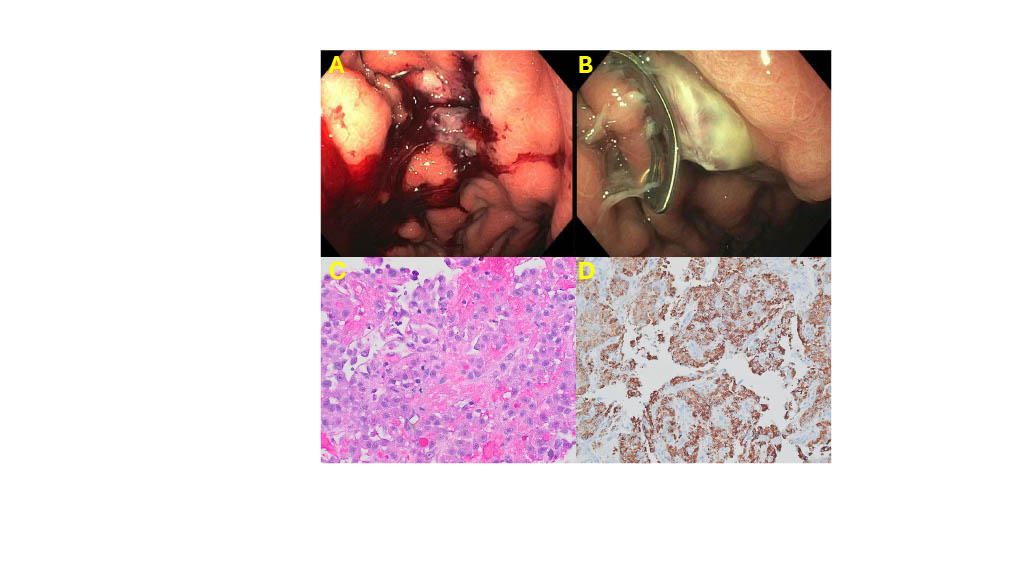
Figure: A. A 9 mm ulcer with fistula found in the gastric body with adherent clot and oozing of blood.
B. Hepatocellular carcinoma protruding through the gastric body with Ovesco clip (which did not close the defect).
C. Gastric biopsy showing an infiltrate of malignant cells (high nuclear-to-cytoplasmic ratios with large prominent nucleoli) arranged in a pseudo-glandular pattern.
D. HepPar1 immunohistochemical stain is positive in the malignant cells consistent with liver primary.
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Rolando Leal indicated no relevant financial relationships.
Samuel Cheong, DO1, Sabrina Ho, MD1, Mohamad Omar Diab, MD2, Franklin Liu, MD3, Natasha Khona, DO1, Brandon Witten, MD1, Rolando J. Leal, MD4. P6031 - Liver's Backdoor Intrusion: A Rare Case of Hepatogastric Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3University of Arizona College of Medicine, Tucson, AZ; 4Banner University Medical Center, Tucson, AZ
Introduction: Hepatocellular carcinoma (HCC) is the most common primary liver cancer. It most commonly metastasizes to the lungs, followed by regional lymph nodes and then bones. Metastasis to the gastrointestinal (GI) tract is rare, occurring in 0.5% to 2% of patients. We present a case of a hepatogastric fistula caused by HCC, likely secondary to Y-90 embolization.
Case Description/
Methods: A 60-year-old male with a history of cirrhosis secondary to MASH complicated by HCC, status post Y-90 radioembolization to segments II and III, and grade III esophageal varices status post banding, presented to the hospital with hematochezia and a hemoglobin (Hgb) of 6.8 g/dL on outpatient labs (baseline 8.0–10.0 g/dL). In the emergency department, repeat labs showed an Hgb of 7.3 g/dL, for which the patient received 1 unit of packed red blood cells. CT angiography (CTA) of the abdomen and pelvis revealed air foci within the previously treated liver cavity with tethering to the stomach, raising concern for a hepatogastric fistula.
EGD revealed grade II medium-sized esophageal varices with red wale signs, as well as two non-bleeding, cratered gastric ulcers concerning for fistulas, which were closed with Ovesco clips. He was subsequently discharged. A month later, he returned with shortness of breath and an outpatient Hgb of 5.5 g/dL. EGD showed similar findings, but the previously placed clips were no longer intact. Attempts to re-close the fistulous openings were unsuccessful due to tissue friability. Biopsies confirmed hepatocellular carcinoma with background gastric ulceration and necrosis. The patient was discharged with close multidisciplinary team follow-up. He was deemed unfit for surgery or liver transplantation and was initiated on systemic therapy with lenvatinib.
Discussion: The predisposing factors for HCC metastasis to the GI tract remain poorly defined due to its rarity. However, proposed risk factors include an exophytic growth pattern, larger tumor size ( >5 cm), and subcapsular location, particularly in the left lobe. Additionally, several reports suggest that loco-regional treatments such as Y-90 radio-embolization or trans-arterial chemo-embolization (TACE) may provoke an inflammatory response in adjacent GI structures, facilitating tumor invasion. HCC may also reach the GI tract via hematogenous spread, in which tumor thrombi enter the portal venous system and disseminate through hepatofugal flow. This case highlights a rare complication of loco-regional treatments in patients with HCC.
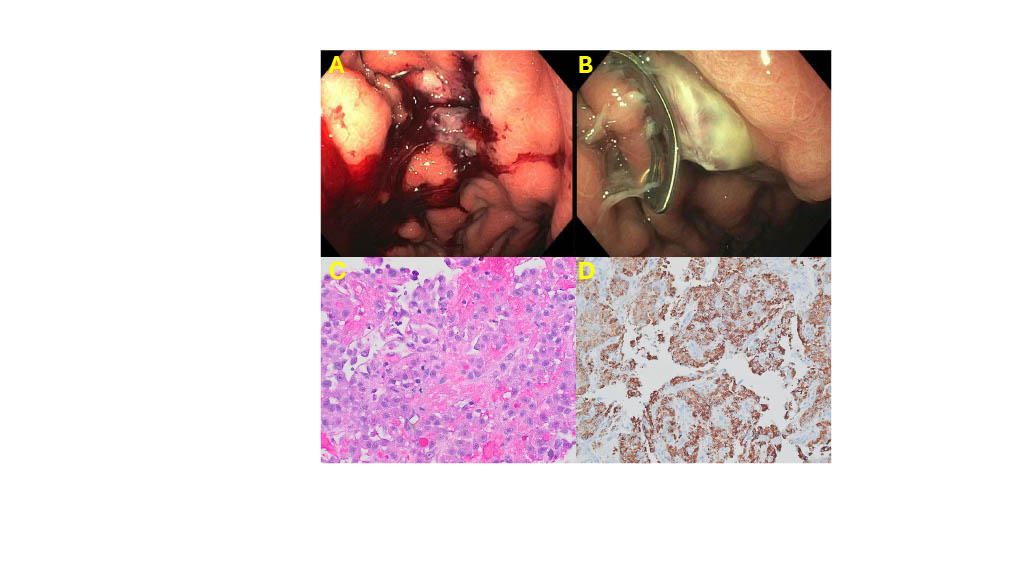
Figure: A. A 9 mm ulcer with fistula found in the gastric body with adherent clot and oozing of blood.
B. Hepatocellular carcinoma protruding through the gastric body with Ovesco clip (which did not close the defect).
C. Gastric biopsy showing an infiltrate of malignant cells (high nuclear-to-cytoplasmic ratios with large prominent nucleoli) arranged in a pseudo-glandular pattern.
D. HepPar1 immunohistochemical stain is positive in the malignant cells consistent with liver primary.
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Rolando Leal indicated no relevant financial relationships.
Samuel Cheong, DO1, Sabrina Ho, MD1, Mohamad Omar Diab, MD2, Franklin Liu, MD3, Natasha Khona, DO1, Brandon Witten, MD1, Rolando J. Leal, MD4. P6031 - Liver's Backdoor Intrusion: A Rare Case of Hepatogastric Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
