Tuesday Poster Session
Category: Liver
P6116 - Non-Cirrhotic Portal Hypertension Due to Prolonged Intrahepatic Cholestasis: Diagnostic Challenges and Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Stuti Manandhar, MD
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Stuti Manandhar, MD, Esteban Verduzco, MD, MMSc, Mohamed K.. Osman, MD, MPH, Joan A.. Culpepper-Morgan, MD, FACG
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Non-cirrhotic portal hypertension is a challenging diagnosis. We present a case of intractable ascites due to non-cirrhotic portal hypertension caused by prolonged intrahepatic cholestasis due to drug-induced liver injury (DILI) and sepsis due to cholecystitis and osteomyelitis.
Case Description/
Methods: A 56-year-old man with T2DM presented with AKI on CKD and calcaneal osteomyelitis and cellulitis. He was placed on antibiotics. By hospital month 3, he was cholestatic with bilirubin of 5, ALK of 2251 and normal ALT and AST (fig.1). WBC was elevated to 11.36. Liver biopsy favored DILI but HIDA showed acute cholecystitis. CT-guided cholecystostomy lowered bilirubin to 0.3 and ALK to 806. After tube removal, bilirubin and ALK rose again to 6.5 and 2126 by month 8. A cholecystostomy tube was placed again, but WBC remained high with left shift. Large volume ascites first appeared on CT. By month 10, he underwent cholecystectomy with decrease in WBC to 5.18. He defervesced despite development of gallbladder fossa abscess. Bilirubin normalized quickly but ALK remained high with normal AST, ALT, and INR. Autoimmune diseases: PSC, PBC and IgG4-related disease were ruled out by antibodies and MRCP favoring DILI. By month 12 platelet count dropped to between 29 and 91 x103 /mcl suggesting hypersplenism. Ascites became intractable requiring bi-monthly large volume paracentesis (10-12 L/month). Transudative ascitic fluid favored new cirrhosis. However, liver biopsy at month 18 only showed minimal cholestasis and no lobular inflammation or fibrosis (fig.2). Yet, wedged hepatic-venous pressure gradient (WHVPG) rose to 14 mmHg. Fibroscan at month 21 showed stage 4 fibrosis and stage 3 steatosis. Yet, CT month 21 did not reveal cirrhosis. Cardiac function was normal on echo. At month 22 he had TIPS for refractory ascites with pre-TIPS WHVPG 7 mmHg and has not since needed paracentesis.
Discussion: The differential for non-cirrhotic portal hypertension includes congestive hepatopathy, Budd Chiari, portal vein thrombosis, veno-occlusive disease, and schistosomiasis. Rarely does prolonged cholestatic injury cause portal hypertension without evidence of fibrosis by reticulin or trichrome stains on biopsy. We posit that defenestration of hepatic sinusoids due to sepsis and DILI-induced cholestasis resulted in portal hypertension. The low albumin due to nephrosis put him at risk for intractable ascites. TIPS redirected fluid volume and decreased need for repeated paracentesis. Liver function stayed normal.
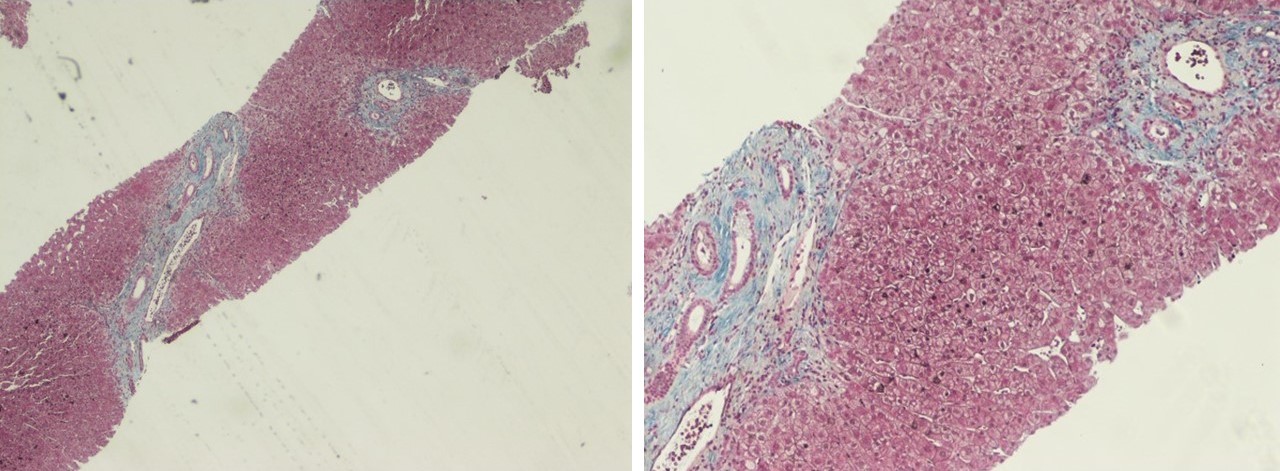
Figure: Figure1. Liver function tests and CBC
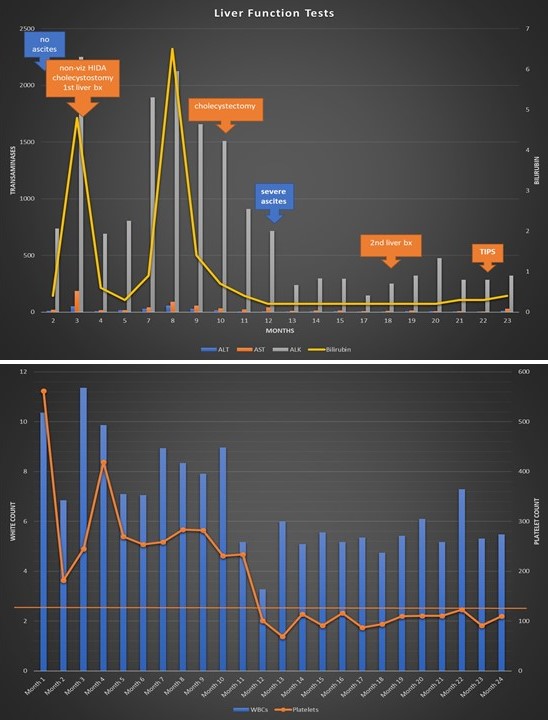
Figure: Figure2. Two portal tracts with no bridging fibrosis
Disclosures:
Stuti Manandhar indicated no relevant financial relationships.
Esteban Verduzco indicated no relevant financial relationships.
Mohamed Osman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Stuti Manandhar, MD, Esteban Verduzco, MD, MMSc, Mohamed K.. Osman, MD, MPH, Joan A.. Culpepper-Morgan, MD, FACG. P6116 - Non-Cirrhotic Portal Hypertension Due to Prolonged Intrahepatic Cholestasis: Diagnostic Challenges and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Non-cirrhotic portal hypertension is a challenging diagnosis. We present a case of intractable ascites due to non-cirrhotic portal hypertension caused by prolonged intrahepatic cholestasis due to drug-induced liver injury (DILI) and sepsis due to cholecystitis and osteomyelitis.
Case Description/
Methods: A 56-year-old man with T2DM presented with AKI on CKD and calcaneal osteomyelitis and cellulitis. He was placed on antibiotics. By hospital month 3, he was cholestatic with bilirubin of 5, ALK of 2251 and normal ALT and AST (fig.1). WBC was elevated to 11.36. Liver biopsy favored DILI but HIDA showed acute cholecystitis. CT-guided cholecystostomy lowered bilirubin to 0.3 and ALK to 806. After tube removal, bilirubin and ALK rose again to 6.5 and 2126 by month 8. A cholecystostomy tube was placed again, but WBC remained high with left shift. Large volume ascites first appeared on CT. By month 10, he underwent cholecystectomy with decrease in WBC to 5.18. He defervesced despite development of gallbladder fossa abscess. Bilirubin normalized quickly but ALK remained high with normal AST, ALT, and INR. Autoimmune diseases: PSC, PBC and IgG4-related disease were ruled out by antibodies and MRCP favoring DILI. By month 12 platelet count dropped to between 29 and 91 x103 /mcl suggesting hypersplenism. Ascites became intractable requiring bi-monthly large volume paracentesis (10-12 L/month). Transudative ascitic fluid favored new cirrhosis. However, liver biopsy at month 18 only showed minimal cholestasis and no lobular inflammation or fibrosis (fig.2). Yet, wedged hepatic-venous pressure gradient (WHVPG) rose to 14 mmHg. Fibroscan at month 21 showed stage 4 fibrosis and stage 3 steatosis. Yet, CT month 21 did not reveal cirrhosis. Cardiac function was normal on echo. At month 22 he had TIPS for refractory ascites with pre-TIPS WHVPG 7 mmHg and has not since needed paracentesis.
Discussion: The differential for non-cirrhotic portal hypertension includes congestive hepatopathy, Budd Chiari, portal vein thrombosis, veno-occlusive disease, and schistosomiasis. Rarely does prolonged cholestatic injury cause portal hypertension without evidence of fibrosis by reticulin or trichrome stains on biopsy. We posit that defenestration of hepatic sinusoids due to sepsis and DILI-induced cholestasis resulted in portal hypertension. The low albumin due to nephrosis put him at risk for intractable ascites. TIPS redirected fluid volume and decreased need for repeated paracentesis. Liver function stayed normal.
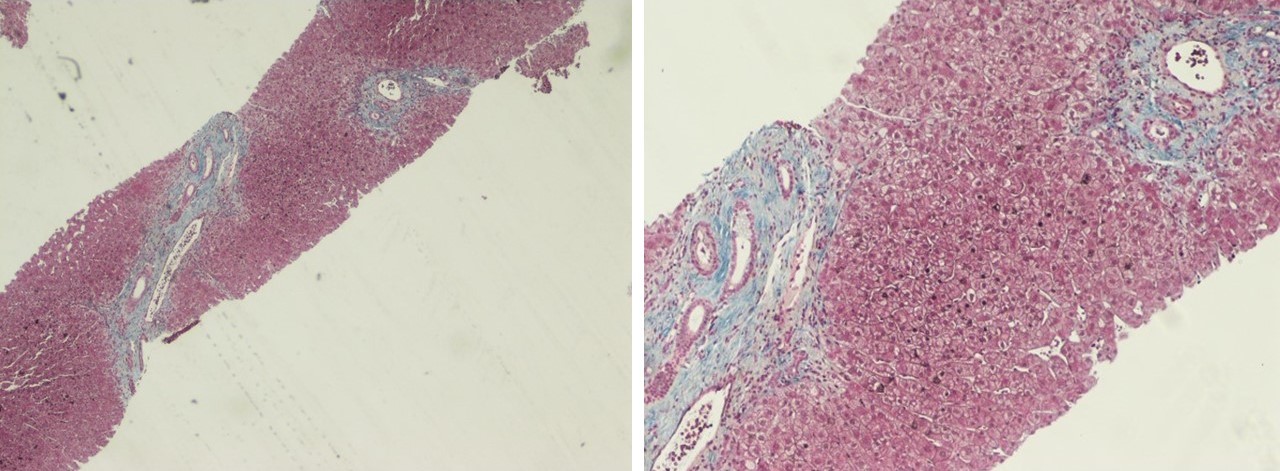
Figure: Figure1. Liver function tests and CBC
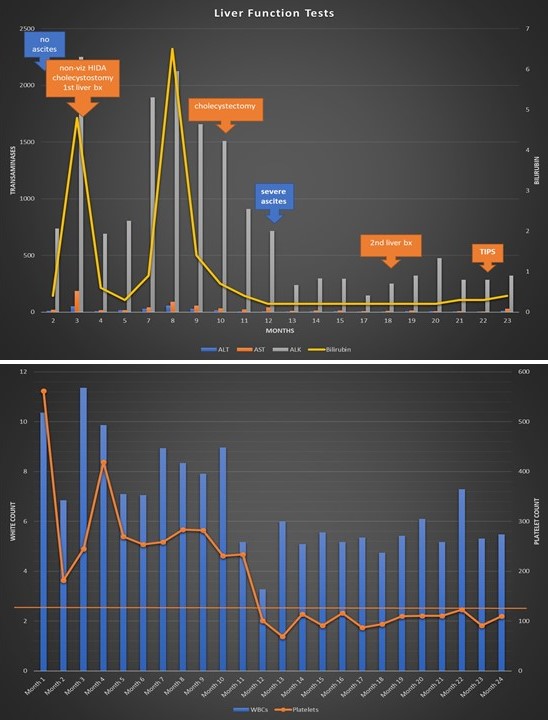
Figure: Figure2. Two portal tracts with no bridging fibrosis
Disclosures:
Stuti Manandhar indicated no relevant financial relationships.
Esteban Verduzco indicated no relevant financial relationships.
Mohamed Osman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Stuti Manandhar, MD, Esteban Verduzco, MD, MMSc, Mohamed K.. Osman, MD, MPH, Joan A.. Culpepper-Morgan, MD, FACG. P6116 - Non-Cirrhotic Portal Hypertension Due to Prolonged Intrahepatic Cholestasis: Diagnostic Challenges and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

