Tuesday Poster Session
Category: Liver
P6112 - Persistent Ascites After Liver Transplantation in the Absence of Obstruction: A Diagnostic Challenge of Sinusoidal Dysfunction and Immune-Mediated Injury
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ishan Antony, MD
Beth Israel Lahey Health
Burlington, MA
Presenting Author(s)
Ishan Antony, MD1, Karim Osman, MD2, Narinderjeet Kaur, MD, MS3, Ming V.. Lin, MD2
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Post liver transplantation (LT) ascites is uncommon and often signals vascular (e.g. hepatic flow obstruction), hepatic (e.g. acute cellular rejection), or extrahepatic (e.g. cardiac failure) complications. We present a case of persistent ascites after deceased donor LT (DDLT), raising suspicion for sinusoidal obstruction syndrome (SOS) related to immune-mediated injury and potentially calcineurin inhibitor toxicity.
Case Description/
Methods: A 53-year-old man with MASH cirrhosis and prior TIPS for variceal bleeding underwent DDLT following TIPS-related encephalopathy. He had persistent cholestasis in the early post-op period without biliary stenosis on ERCP, attributed to ischemic reperfusion injury. Three weeks later, he developed new large-volume ascites requiring frequent paracenteses. Lab showed AST 157 U/L, ALT 79 U/L, ALP 1681 U/L, bilirubin 5 mg/dL. Hepatic veins and IVC were patent on CT hepatic venography. Hepatic venous pressure gradient (HVPG) was 21 mmHg, consistent with portal hypertension. Ascites was transudative (SAAG 1.3) with normal cell count and negative cultures. Initial liver biopsy showed sinusoidal congestion without rejection or fibrosis. Cardiac evaluation was unrevealing. Mycophenolate was stopped due to suspected SOS, but symptoms persisted. Ascites remained despite IVC dilation, biliary drainage, and diuresis. He developed weight loss, hyponatremia, AKI, and hypoalbuminemia requiring TPN. Repeat biopsy showed mild pericellular fibrosis with negative C4d staining. Donor-specific antibody was intermittently positive but without a clear pattern of antibody-mediated rejection (AMR). Tacrolimus trough level peaked at 21.7 ng/mL. He had 3 sessions of plasmapheresis with IVIG for suspected immune-mediated injury without improvement. His course was complicated by VRE peritonitis and duodenal ulcer bleeding, leading to respiratory decompensation and hospice transition 211 days post-LT.
Discussion: This case highlights the challenge of managing post-LT ascites without large-vessel obstruction. Despite patent outflow, elevated HVPG and histology suggested sinusoidal or microvascular dysfunction. Early post-LT ascites with elevated HVPG and immunologic activation (e.g., DSA, borderline rejection) should raise concern for SOS-spectrum injury. Tacrolimus toxicity and subclinical AMR were considered, but treatment yielded no benefit. This case suggests that the combination of post-LT ascites and AMR, even when subtle, may indicate severe endothelial injury and poor prognosis.
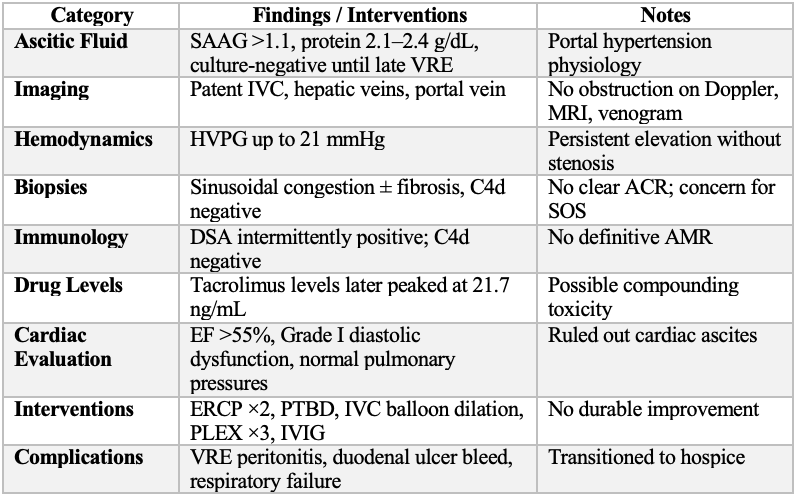
Figure: Table 1: Summary of Key Diagnostic and Therapeutic Interventions
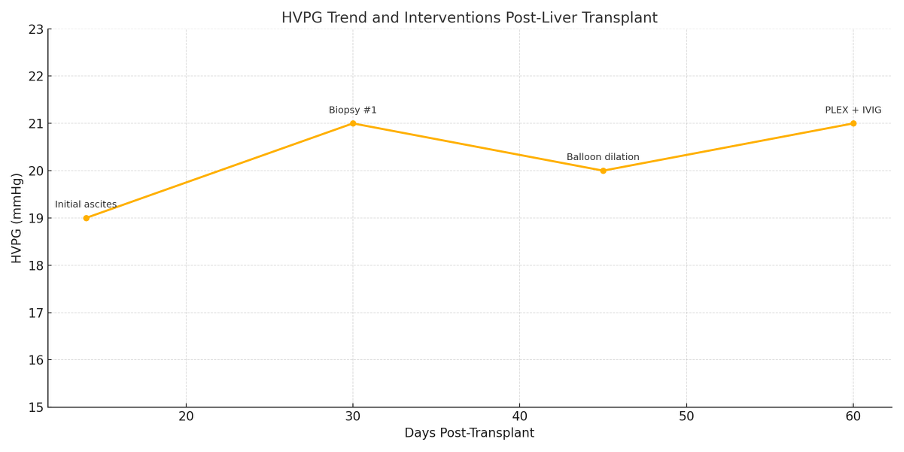
Figure: Figure 1: HVPG Trends and Interventions Following Liver Transplantation
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Karim Osman indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Ishan Antony, MD1, Karim Osman, MD2, Narinderjeet Kaur, MD, MS3, Ming V.. Lin, MD2. P6112 - Persistent Ascites After Liver Transplantation in the Absence of Obstruction: A Diagnostic Challenge of Sinusoidal Dysfunction and Immune-Mediated Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Post liver transplantation (LT) ascites is uncommon and often signals vascular (e.g. hepatic flow obstruction), hepatic (e.g. acute cellular rejection), or extrahepatic (e.g. cardiac failure) complications. We present a case of persistent ascites after deceased donor LT (DDLT), raising suspicion for sinusoidal obstruction syndrome (SOS) related to immune-mediated injury and potentially calcineurin inhibitor toxicity.
Case Description/
Methods: A 53-year-old man with MASH cirrhosis and prior TIPS for variceal bleeding underwent DDLT following TIPS-related encephalopathy. He had persistent cholestasis in the early post-op period without biliary stenosis on ERCP, attributed to ischemic reperfusion injury. Three weeks later, he developed new large-volume ascites requiring frequent paracenteses. Lab showed AST 157 U/L, ALT 79 U/L, ALP 1681 U/L, bilirubin 5 mg/dL. Hepatic veins and IVC were patent on CT hepatic venography. Hepatic venous pressure gradient (HVPG) was 21 mmHg, consistent with portal hypertension. Ascites was transudative (SAAG 1.3) with normal cell count and negative cultures. Initial liver biopsy showed sinusoidal congestion without rejection or fibrosis. Cardiac evaluation was unrevealing. Mycophenolate was stopped due to suspected SOS, but symptoms persisted. Ascites remained despite IVC dilation, biliary drainage, and diuresis. He developed weight loss, hyponatremia, AKI, and hypoalbuminemia requiring TPN. Repeat biopsy showed mild pericellular fibrosis with negative C4d staining. Donor-specific antibody was intermittently positive but without a clear pattern of antibody-mediated rejection (AMR). Tacrolimus trough level peaked at 21.7 ng/mL. He had 3 sessions of plasmapheresis with IVIG for suspected immune-mediated injury without improvement. His course was complicated by VRE peritonitis and duodenal ulcer bleeding, leading to respiratory decompensation and hospice transition 211 days post-LT.
Discussion: This case highlights the challenge of managing post-LT ascites without large-vessel obstruction. Despite patent outflow, elevated HVPG and histology suggested sinusoidal or microvascular dysfunction. Early post-LT ascites with elevated HVPG and immunologic activation (e.g., DSA, borderline rejection) should raise concern for SOS-spectrum injury. Tacrolimus toxicity and subclinical AMR were considered, but treatment yielded no benefit. This case suggests that the combination of post-LT ascites and AMR, even when subtle, may indicate severe endothelial injury and poor prognosis.
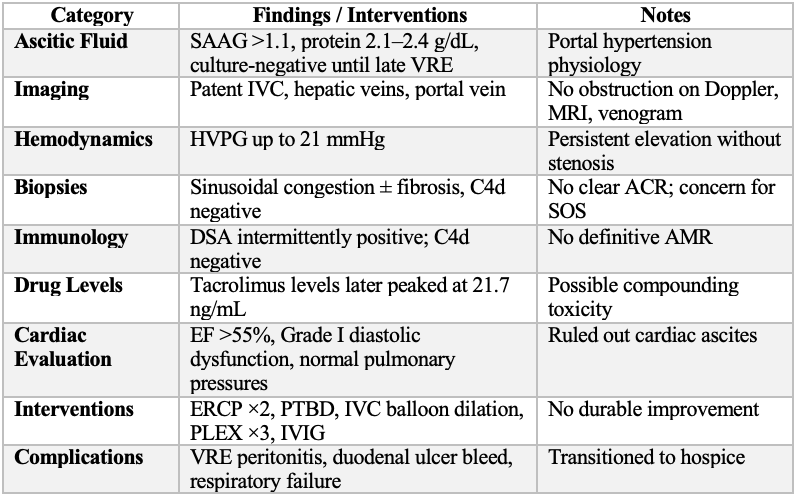
Figure: Table 1: Summary of Key Diagnostic and Therapeutic Interventions
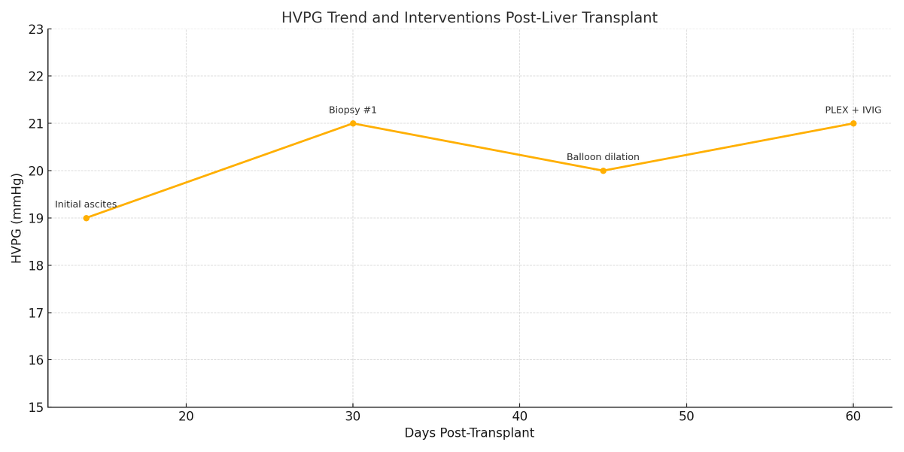
Figure: Figure 1: HVPG Trends and Interventions Following Liver Transplantation
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Karim Osman indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Ishan Antony, MD1, Karim Osman, MD2, Narinderjeet Kaur, MD, MS3, Ming V.. Lin, MD2. P6112 - Persistent Ascites After Liver Transplantation in the Absence of Obstruction: A Diagnostic Challenge of Sinusoidal Dysfunction and Immune-Mediated Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
