Tuesday Poster Session
Category: Small Intestine
P6239 - Bezoar-Induced Small Bowel Obstruction: A Case Highlighting the Role of Imaging and Multidisciplinary Care
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Julian Azar, MD (he/him/his)
Yale New Haven Health
New Haven, CT
Presenting Author(s)
Julian Azar, MD1, Louis J. Levine, MD, MEd2, Ira Leeds, MD3, Jose Restrepo, MD4, Petr Protiva, MD, MPH2, Amy Ogurick, MD2
1Yale New Haven Health, New Haven, CT; 2Yale Digestive Diseases, New Haven, CT; 3Department of Surgery's Division of Colon & Rectal Surgery, Yale School of Medicine, New Haven, CT; 4Veterans Affairs Connecticut Healthcare System, West Haven, CT
Introduction: Small bowel (SB) bezoars are rare, but can lead to serious complications, including ischemia and small bowel obstruction (SBO). This case highlights the importance of imaging and multidisciplinary discussion in recognizing bezoar-induced SBO.
Case Description/
Methods: A 68-year-old man with history of remote SBO due to jejunal diverticulitis status post SB resection presented with five days of generalized abdominal pain and poor oral intake. Abdominal CT showed dilated, edematous SB loops. Upon admission to the surgical team, emergent intervention was deferred given benign physical exam and labs (no leukocytosis, normal lactate). The patient initially improved with IV fluids, NPO, and nasogastric tube decompression. Upon diet resumption, abdominal pain recurred, along with nausea and vomiting. Repeat CT revealed chronically thickened SB loops, but no evidence of ongoing obstruction. Fecal calprotectin was checked due to thickened bowel loops and was elevated (2940 μg/g). However, without other signs of IBD, and concern for intermittent SBO, endoscopy was deferred. Total parenteral nutrition and IV antibiotics were initiated.
The patient later developed acute abdominal pain, distension, nausea, and obstipation. Repeat CT revealed SBO and a 3-cm bezoar in the ileum, at the transition point of the SBO. The bezoar, initially seen in the jejunum on re-review of prior imaging, had impacted the ileum, causing obstruction [Figure 1]. It was felt the bezoar was likely intermittently obstructing, causing SBO symptoms. He underwent laparoscopic SB resection, which confirmed large SB diverticulosis [Figure 2] and an impacted bezoar at the ileum. Post-operatively, symptoms improved, and he was later discharged.
Discussion: Bezoars are conglomerates of substances (hair, plant fibers, medications, milk) that can lodge in the stomach, and less commonly cause SBO. Formation is linked to GI motility disorders, inflammatory strictures, blind loops, and SB diverticula. They can cause ischemia and obstruction.
SB bezoars pose a diagnostic challenge due to variable presentation with nonspecific symptoms and difficult endoscopic visualization, making imaging crucial. Most cases require surgery, especially if the bezoar cannot be reached by endoscopy.
This case highlights how the diagnosis of a bezoar-induced SBO can be delayed or missed without high clinical suspicion. It emphasizes the value of repeated imaging and collaborative decision-making among surgery, gastroenterology, and radiology.
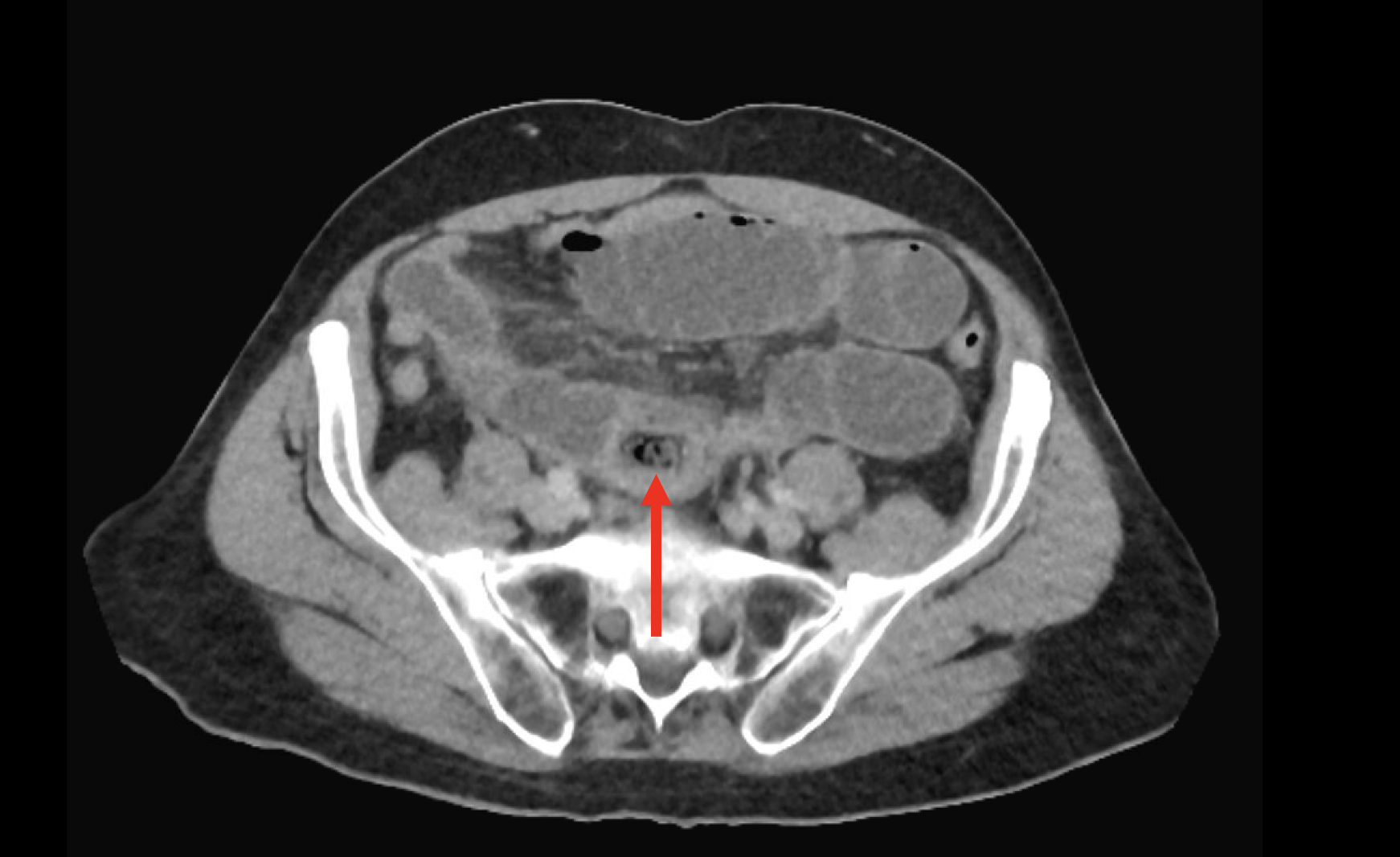
Figure: Encapsulated, heterogeneous, air-containing structure in the proximal to mid ileum consistent with a bezoar, confirmed post-SB resection. Transition point also visualized.

Figure: Laparoscopic view of large jejunal diverticulosis in this patient.
Disclosures:
Julian Azar indicated no relevant financial relationships.
Louis Levine indicated no relevant financial relationships.
Ira Leeds: Intuitive Surgical – Consultant.
Jose Restrepo indicated no relevant financial relationships.
Petr Protiva indicated no relevant financial relationships.
Amy Ogurick indicated no relevant financial relationships.
Julian Azar, MD1, Louis J. Levine, MD, MEd2, Ira Leeds, MD3, Jose Restrepo, MD4, Petr Protiva, MD, MPH2, Amy Ogurick, MD2. P6239 - Bezoar-Induced Small Bowel Obstruction: A Case Highlighting the Role of Imaging and Multidisciplinary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Health, New Haven, CT; 2Yale Digestive Diseases, New Haven, CT; 3Department of Surgery's Division of Colon & Rectal Surgery, Yale School of Medicine, New Haven, CT; 4Veterans Affairs Connecticut Healthcare System, West Haven, CT
Introduction: Small bowel (SB) bezoars are rare, but can lead to serious complications, including ischemia and small bowel obstruction (SBO). This case highlights the importance of imaging and multidisciplinary discussion in recognizing bezoar-induced SBO.
Case Description/
Methods: A 68-year-old man with history of remote SBO due to jejunal diverticulitis status post SB resection presented with five days of generalized abdominal pain and poor oral intake. Abdominal CT showed dilated, edematous SB loops. Upon admission to the surgical team, emergent intervention was deferred given benign physical exam and labs (no leukocytosis, normal lactate). The patient initially improved with IV fluids, NPO, and nasogastric tube decompression. Upon diet resumption, abdominal pain recurred, along with nausea and vomiting. Repeat CT revealed chronically thickened SB loops, but no evidence of ongoing obstruction. Fecal calprotectin was checked due to thickened bowel loops and was elevated (2940 μg/g). However, without other signs of IBD, and concern for intermittent SBO, endoscopy was deferred. Total parenteral nutrition and IV antibiotics were initiated.
The patient later developed acute abdominal pain, distension, nausea, and obstipation. Repeat CT revealed SBO and a 3-cm bezoar in the ileum, at the transition point of the SBO. The bezoar, initially seen in the jejunum on re-review of prior imaging, had impacted the ileum, causing obstruction [Figure 1]. It was felt the bezoar was likely intermittently obstructing, causing SBO symptoms. He underwent laparoscopic SB resection, which confirmed large SB diverticulosis [Figure 2] and an impacted bezoar at the ileum. Post-operatively, symptoms improved, and he was later discharged.
Discussion: Bezoars are conglomerates of substances (hair, plant fibers, medications, milk) that can lodge in the stomach, and less commonly cause SBO. Formation is linked to GI motility disorders, inflammatory strictures, blind loops, and SB diverticula. They can cause ischemia and obstruction.
SB bezoars pose a diagnostic challenge due to variable presentation with nonspecific symptoms and difficult endoscopic visualization, making imaging crucial. Most cases require surgery, especially if the bezoar cannot be reached by endoscopy.
This case highlights how the diagnosis of a bezoar-induced SBO can be delayed or missed without high clinical suspicion. It emphasizes the value of repeated imaging and collaborative decision-making among surgery, gastroenterology, and radiology.
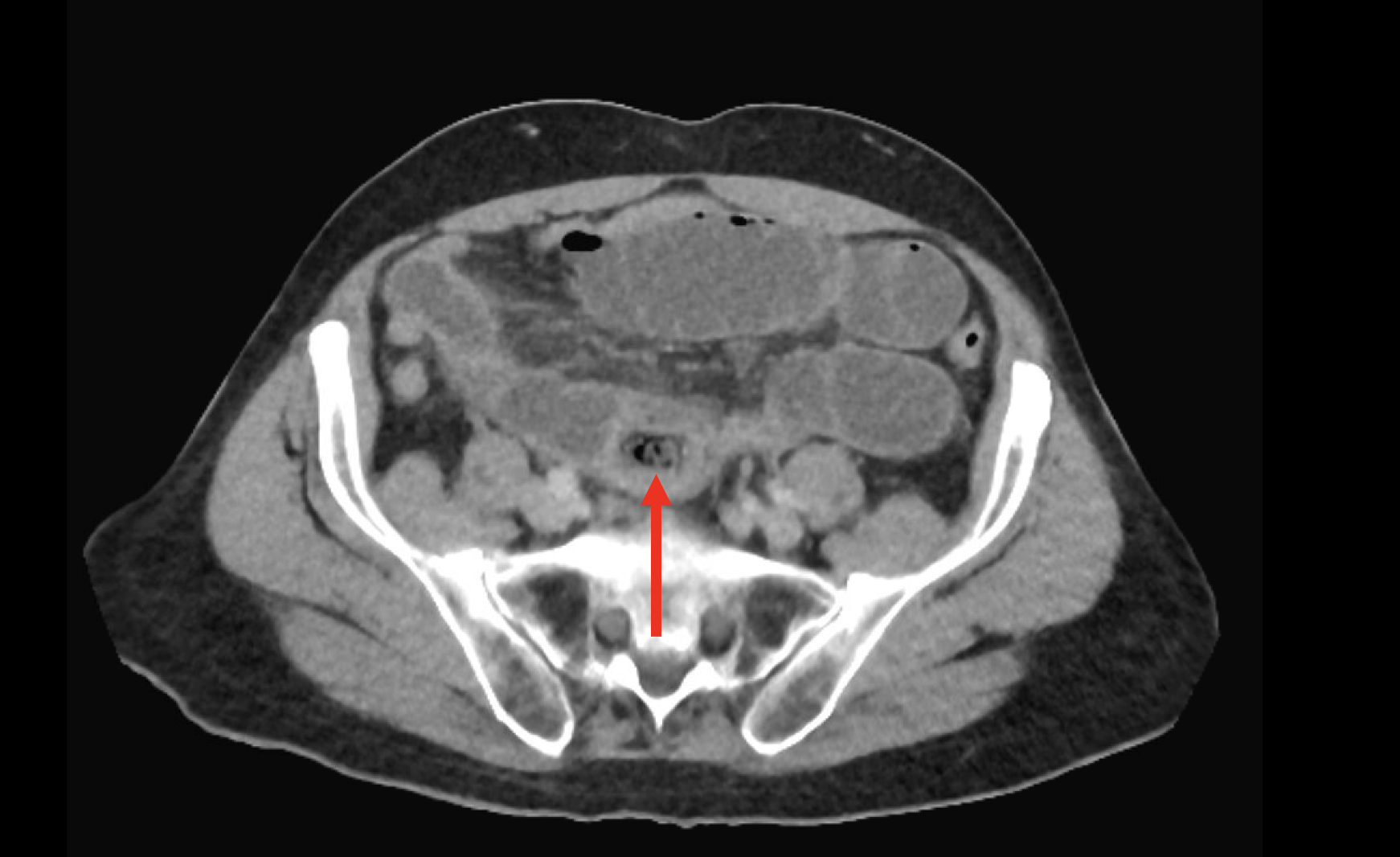
Figure: Encapsulated, heterogeneous, air-containing structure in the proximal to mid ileum consistent with a bezoar, confirmed post-SB resection. Transition point also visualized.

Figure: Laparoscopic view of large jejunal diverticulosis in this patient.
Disclosures:
Julian Azar indicated no relevant financial relationships.
Louis Levine indicated no relevant financial relationships.
Ira Leeds: Intuitive Surgical – Consultant.
Jose Restrepo indicated no relevant financial relationships.
Petr Protiva indicated no relevant financial relationships.
Amy Ogurick indicated no relevant financial relationships.
Julian Azar, MD1, Louis J. Levine, MD, MEd2, Ira Leeds, MD3, Jose Restrepo, MD4, Petr Protiva, MD, MPH2, Amy Ogurick, MD2. P6239 - Bezoar-Induced Small Bowel Obstruction: A Case Highlighting the Role of Imaging and Multidisciplinary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

