Tuesday Poster Session
Category: Practice Management
P6177 - Pulmonary Embolism-Related Mortality Patterns Among Gastrointestinal Cancer Patients in the United States: Analysis of a Nationwide Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Niloy Ghosh, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Abdul Awan, MBBS1, Muhammad A. Nadeem, MD2, Niloy Ghosh, MD3, Abdullah Ahmad, MD4, Ahsan Raja, MD5, Jibran Ikram, MD2, Abhishek Patel, MD3, Amir Sohail, MD, MSc6, Abu Baker Sheikh, MD3
1Nishtar Medical University, Multan, Punjab, Pakistan; 2Cleveland Clinic, Cleveland, OH; 3University of New Mexico Health Sciences Center, Albuquerque, NM; 4CMH Lahore Medical College, Lahore, Punjab, Pakistan; 5Aga Khan University Medical Center, Karachi, Sindh, Pakistan; 6University of New Mexico, Albuquerque, NM
Introduction: Malignancy-associated hypercoagulability predisposes patients to thromboembolic complications such as pulmonary embolism (PE). However, there is limited data addressing demographic disparities in PE-related mortality among patients with gastrointestinal (GI) malignancies. To better understand and address potential systemic inequities in intervention and healthcare access, this study analyzes temporal trends and demographic patterns in PE-related mortality among GI cancer patients using data from the CDC WONDER database.
Methods: We conducted a retrospective analysis using data from the CDC WONDER database covering the years 1999–2020. Patients with a documented history of GI malignancy (ICD-10 codes C15–C26) and PE-related mortality (ICD-10 code I26) were identified. Individuals under the age of 15 were excluded. Age-adjusted mortality rates (AAMR) were calculated and stratified by demographic variables. Monotonic trends were assessed using the Mann-Kendall test, and group comparisons for continuous variables were performed using the t-test.
Results: From 1999 to 2020, the overall AAMR for PE-related deaths in patients with GI malignancies was 0.724 per 100,000 (95% CI: 0.731–0.718). Both men (τ = 0.685, p < 0.001) and women (τ = 0.550, p < 0.001) exhibited significant upward trends. Across all racial and age groups, males consistently had higher AAMRs than females. The Black population demonstrated significantly higher mortality compared to White individuals (p < 0.001 for both Black vs. White males and females). While most groups showed a significant rise in mortality over time, the trend was not significant among Black males (p = 0.535). Older adults had significantly higher AAMRs compared to younger counterparts (p < 0.001 across all subgroups). Regionally, males in the Midwest had the highest observed AAMR (Table 1).
Discussion: This study identifies significant disparities in PE-related mortality among patients with GI malignancies. Men, Black individuals, and older adults are at higher risk of mortality, underscoring the urgent need for targeted, equity-focused strategies in prevention, early detection, and intervention. These findings highlight key areas for public health action to reduce demographic disparities in cancer-associated thromboembolic outcomes.
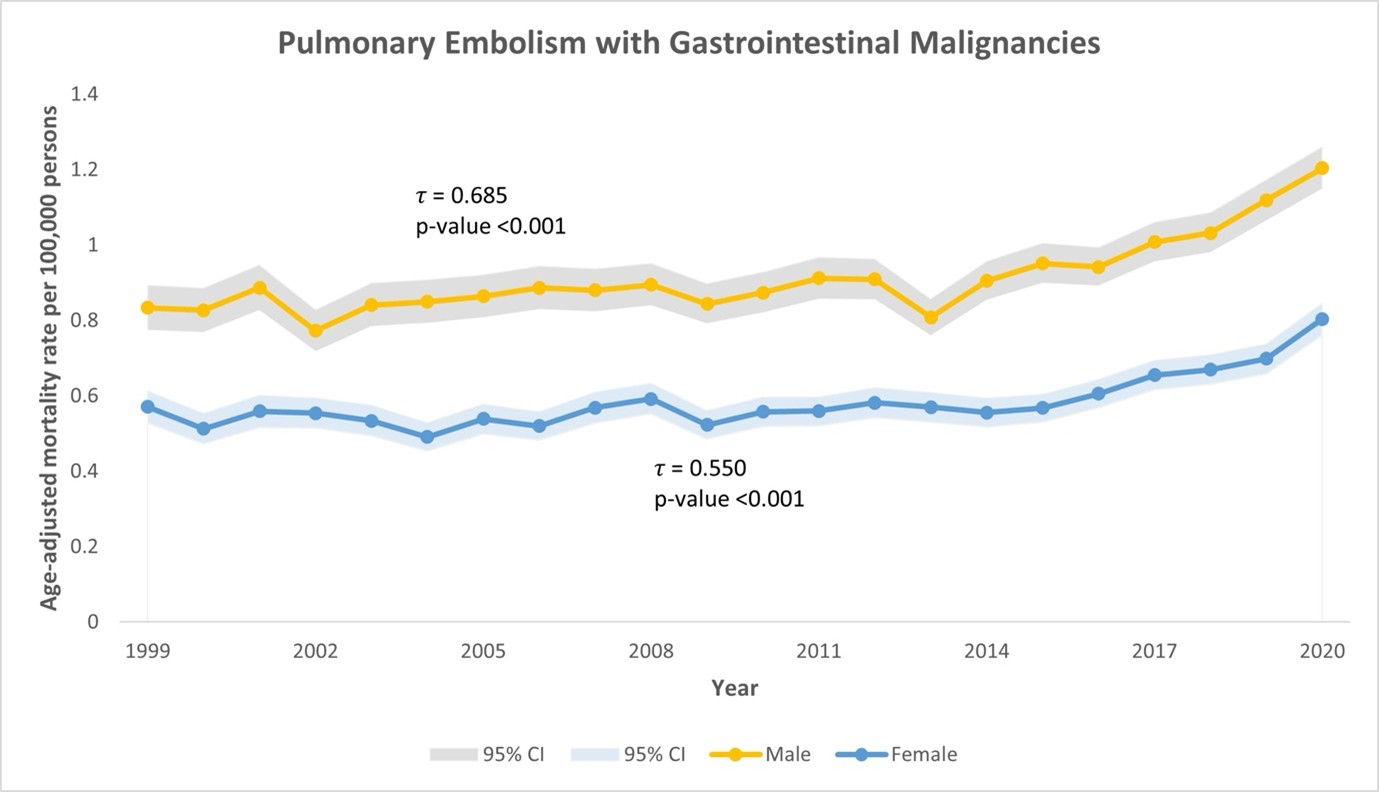
Figure: Table 1: AAMR for PE-related deaths in patients with GI malignancies
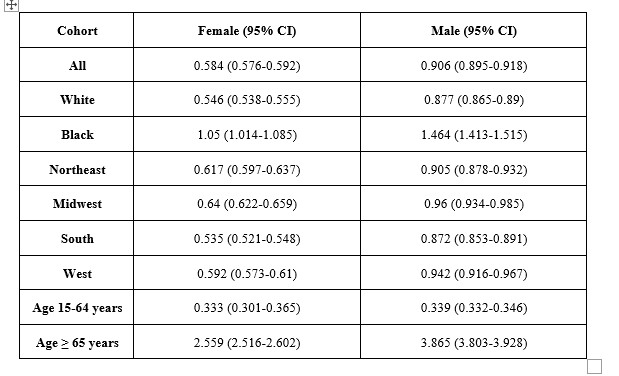
Figure: Figure 1: Trends in Age-Adjusted Mortality Rate in Patients with PE in setting of GI Malignancies
Disclosures:
Abdul Awan indicated no relevant financial relationships.
Muhammad Nadeem indicated no relevant financial relationships.
Niloy Ghosh indicated no relevant financial relationships.
Abdullah Ahmad indicated no relevant financial relationships.
Ahsan Raja indicated no relevant financial relationships.
Jibran Ikram indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Abdul Awan, MBBS1, Muhammad A. Nadeem, MD2, Niloy Ghosh, MD3, Abdullah Ahmad, MD4, Ahsan Raja, MD5, Jibran Ikram, MD2, Abhishek Patel, MD3, Amir Sohail, MD, MSc6, Abu Baker Sheikh, MD3. P6177 - Pulmonary Embolism-Related Mortality Patterns Among Gastrointestinal Cancer Patients in the United States: Analysis of a Nationwide Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nishtar Medical University, Multan, Punjab, Pakistan; 2Cleveland Clinic, Cleveland, OH; 3University of New Mexico Health Sciences Center, Albuquerque, NM; 4CMH Lahore Medical College, Lahore, Punjab, Pakistan; 5Aga Khan University Medical Center, Karachi, Sindh, Pakistan; 6University of New Mexico, Albuquerque, NM
Introduction: Malignancy-associated hypercoagulability predisposes patients to thromboembolic complications such as pulmonary embolism (PE). However, there is limited data addressing demographic disparities in PE-related mortality among patients with gastrointestinal (GI) malignancies. To better understand and address potential systemic inequities in intervention and healthcare access, this study analyzes temporal trends and demographic patterns in PE-related mortality among GI cancer patients using data from the CDC WONDER database.
Methods: We conducted a retrospective analysis using data from the CDC WONDER database covering the years 1999–2020. Patients with a documented history of GI malignancy (ICD-10 codes C15–C26) and PE-related mortality (ICD-10 code I26) were identified. Individuals under the age of 15 were excluded. Age-adjusted mortality rates (AAMR) were calculated and stratified by demographic variables. Monotonic trends were assessed using the Mann-Kendall test, and group comparisons for continuous variables were performed using the t-test.
Results: From 1999 to 2020, the overall AAMR for PE-related deaths in patients with GI malignancies was 0.724 per 100,000 (95% CI: 0.731–0.718). Both men (τ = 0.685, p < 0.001) and women (τ = 0.550, p < 0.001) exhibited significant upward trends. Across all racial and age groups, males consistently had higher AAMRs than females. The Black population demonstrated significantly higher mortality compared to White individuals (p < 0.001 for both Black vs. White males and females). While most groups showed a significant rise in mortality over time, the trend was not significant among Black males (p = 0.535). Older adults had significantly higher AAMRs compared to younger counterparts (p < 0.001 across all subgroups). Regionally, males in the Midwest had the highest observed AAMR (Table 1).
Discussion: This study identifies significant disparities in PE-related mortality among patients with GI malignancies. Men, Black individuals, and older adults are at higher risk of mortality, underscoring the urgent need for targeted, equity-focused strategies in prevention, early detection, and intervention. These findings highlight key areas for public health action to reduce demographic disparities in cancer-associated thromboembolic outcomes.
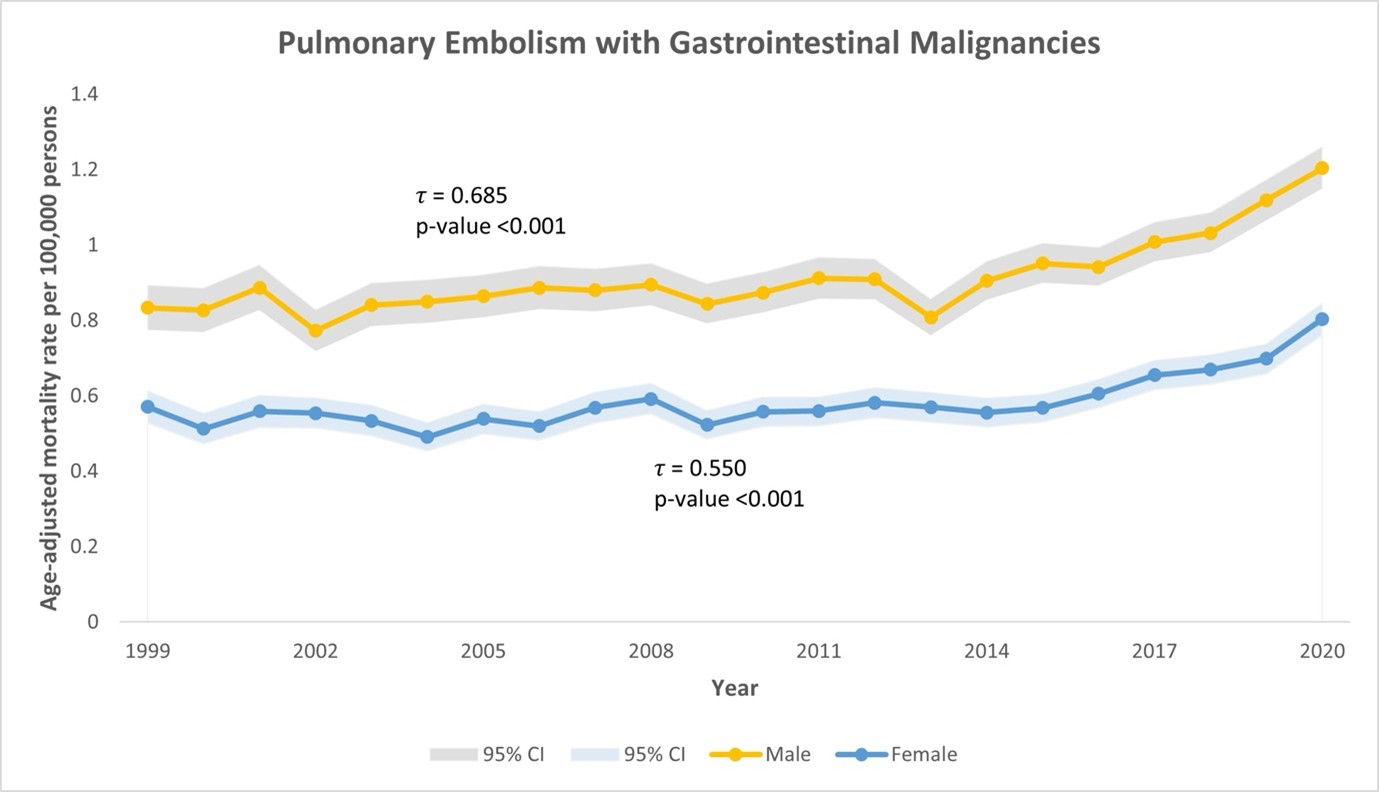
Figure: Table 1: AAMR for PE-related deaths in patients with GI malignancies
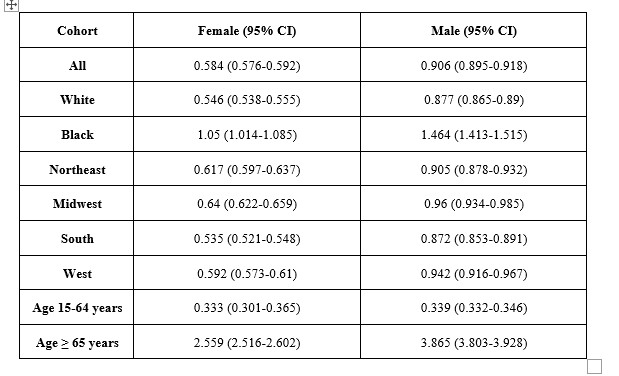
Figure: Figure 1: Trends in Age-Adjusted Mortality Rate in Patients with PE in setting of GI Malignancies
Disclosures:
Abdul Awan indicated no relevant financial relationships.
Muhammad Nadeem indicated no relevant financial relationships.
Niloy Ghosh indicated no relevant financial relationships.
Abdullah Ahmad indicated no relevant financial relationships.
Ahsan Raja indicated no relevant financial relationships.
Jibran Ikram indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Abdul Awan, MBBS1, Muhammad A. Nadeem, MD2, Niloy Ghosh, MD3, Abdullah Ahmad, MD4, Ahsan Raja, MD5, Jibran Ikram, MD2, Abhishek Patel, MD3, Amir Sohail, MD, MSc6, Abu Baker Sheikh, MD3. P6177 - Pulmonary Embolism-Related Mortality Patterns Among Gastrointestinal Cancer Patients in the United States: Analysis of a Nationwide Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
