Tuesday Poster Session
Category: Practice Management
P6175 - Transforming the Gastroenterology Morbidity and Mortality Conference: A Multicenter, Fellow-Led Approach to Systems Thinking, Equity, and Safety Culture
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samantha Magier, MD, MEng
Brigham and Women's Hospital, Harvard Medical School
Dedham, MA
Presenting Author(s)
Award: ACG Outstanding Research Award in the Practice Management Category (Trainee)
Award: ACG Presidential Poster Award
Samantha Magier, MD, MEng1, Daniel Stein, MD, MPH2, Ryan Flanagan, MD, MPH2, Kunal Jajoo, MD2, Michelle L. Hughes, MD3
1Brigham and Women's Hospital, Harvard Medical School, Dedham, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Yale School of Medicine, Orange, CT
Introduction: Modern patient safety (PS) culture emphasizes shared accountability and constructive assessment of adverse outcomes to improve care. Morbidity and Mortality (M&M) reviews are a major process to support this, but limited data exists on implementation in gastroenterology (GI). This gap highlights the need for resources to train gastroenterologists to recognize and address key PS drivers. Tools like the SBAR and Ottawa M&M Model (OM3) can be adopted to guide communication and productive error analysis to advance this aim.
Methods: A structured, trainee-led M&M conference was implemented at two GI training programs: Institution 1 (I1) in 9/2021 and Institution 2 (I2) in 10/2024, with data collected through 5/2025. I1 captured complete case data through 6/2023 before transitioning to a maintenance phase focused on scale-up at I2. Pre-intervention M&Ms at both sites were unstructured and limited to procedural complications. Post-intervention, trainees met with QI-proficient mentors prior to presenting cases using standardized SBAR- and OM3-based models. Each case included an apparent cause analysis addressing systems factors, cognitive bias (CB), and social determinants of health (SDOH). Action items, division feedback, and outcomes were tracked. ACGME fellow surveys were reviewed for trends in PS culture.
Results: Detailed review of 21 cases (I1:12 ; I2:9) confirmed 100% adherence to new format (Table 1). I1 completed 16 additional cases after 6/2023 excluded from analysis. Both sites identified CB in ≥89% of cases and addressed all CB categories. SDOH were discussed in ≥83% of cases. All cases identified change opportunities and proposed interventions, with an implementation rate up to 48%. Post-intervention, fellows at both programs reported an absolute increase in PS event investigation participation, strengthened perceptions of personal responsibility for PS, and universal knowledge of how to report PS events by 2025 (Table 2).
Discussion: This multicenter implementation of a structured, trainee-led GI M&M conference shifted focus from procedural and individual errors to systems-based learning by addressing cognitive reasoning pitfalls, SDOH, and healthcare delivery flaws. The process was scalable and reproducible across two academic centers, led to measurable interventions to improve care quality and safety, and enhanced fellow engagement in safety culture. A structured M&M framework should be broadly implemented to promote patient safety and accountability in GI training programs.
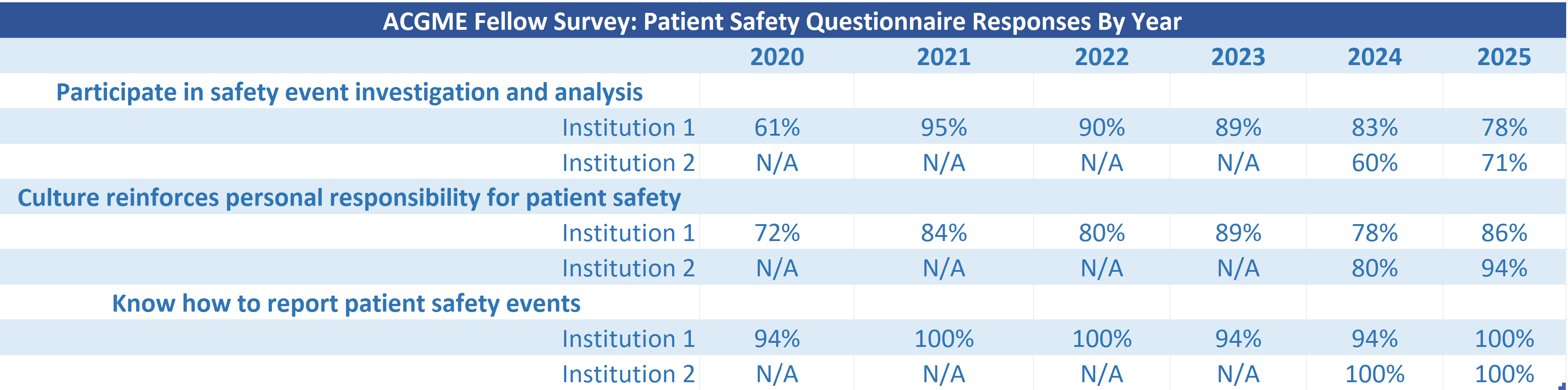
Figure: Table 1. Summary of Case Metrics and Interventions by Institution
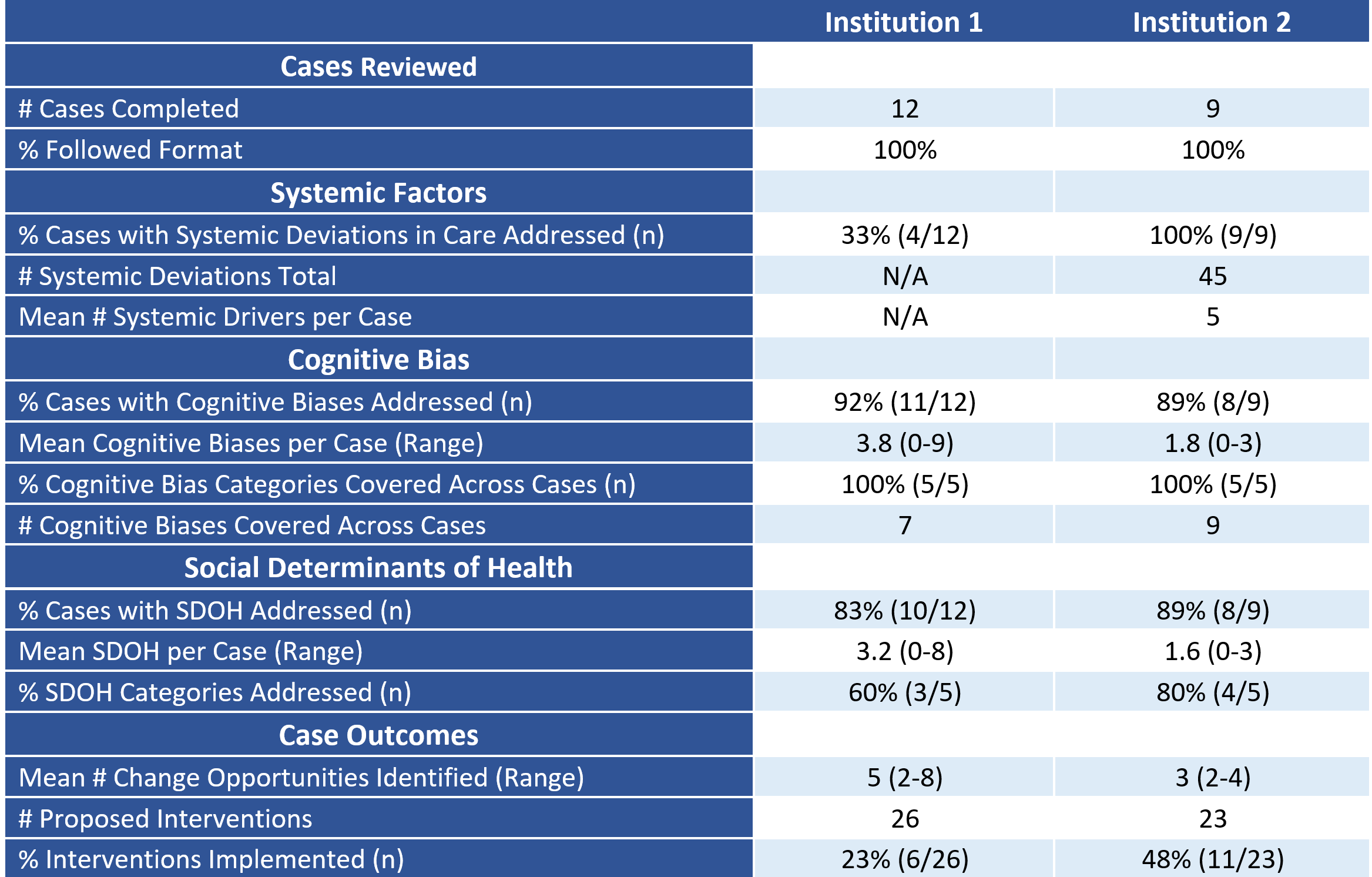
Figure: Table 2. ACGME Fellow Survey: Patient Safety Questionnaire Responses By Year
Disclosures:
Samantha Magier indicated no relevant financial relationships.
Daniel Stein: Fujifilm endoscopy – Consultant. Ovesco endoscopy – Grant/Research Support.
Ryan Flanagan indicated no relevant financial relationships.
Kunal Jajoo indicated no relevant financial relationships.
Michelle Hughes: Iterative Health – Consultant.
Samantha Magier, MD, MEng1, Daniel Stein, MD, MPH2, Ryan Flanagan, MD, MPH2, Kunal Jajoo, MD2, Michelle L. Hughes, MD3. P6175 - Transforming the Gastroenterology Morbidity and Mortality Conference: A Multicenter, Fellow-Led Approach to Systems Thinking, Equity, and Safety Culture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Award: ACG Presidential Poster Award
Samantha Magier, MD, MEng1, Daniel Stein, MD, MPH2, Ryan Flanagan, MD, MPH2, Kunal Jajoo, MD2, Michelle L. Hughes, MD3
1Brigham and Women's Hospital, Harvard Medical School, Dedham, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Yale School of Medicine, Orange, CT
Introduction: Modern patient safety (PS) culture emphasizes shared accountability and constructive assessment of adverse outcomes to improve care. Morbidity and Mortality (M&M) reviews are a major process to support this, but limited data exists on implementation in gastroenterology (GI). This gap highlights the need for resources to train gastroenterologists to recognize and address key PS drivers. Tools like the SBAR and Ottawa M&M Model (OM3) can be adopted to guide communication and productive error analysis to advance this aim.
Methods: A structured, trainee-led M&M conference was implemented at two GI training programs: Institution 1 (I1) in 9/2021 and Institution 2 (I2) in 10/2024, with data collected through 5/2025. I1 captured complete case data through 6/2023 before transitioning to a maintenance phase focused on scale-up at I2. Pre-intervention M&Ms at both sites were unstructured and limited to procedural complications. Post-intervention, trainees met with QI-proficient mentors prior to presenting cases using standardized SBAR- and OM3-based models. Each case included an apparent cause analysis addressing systems factors, cognitive bias (CB), and social determinants of health (SDOH). Action items, division feedback, and outcomes were tracked. ACGME fellow surveys were reviewed for trends in PS culture.
Results: Detailed review of 21 cases (I1:12 ; I2:9) confirmed 100% adherence to new format (Table 1). I1 completed 16 additional cases after 6/2023 excluded from analysis. Both sites identified CB in ≥89% of cases and addressed all CB categories. SDOH were discussed in ≥83% of cases. All cases identified change opportunities and proposed interventions, with an implementation rate up to 48%. Post-intervention, fellows at both programs reported an absolute increase in PS event investigation participation, strengthened perceptions of personal responsibility for PS, and universal knowledge of how to report PS events by 2025 (Table 2).
Discussion: This multicenter implementation of a structured, trainee-led GI M&M conference shifted focus from procedural and individual errors to systems-based learning by addressing cognitive reasoning pitfalls, SDOH, and healthcare delivery flaws. The process was scalable and reproducible across two academic centers, led to measurable interventions to improve care quality and safety, and enhanced fellow engagement in safety culture. A structured M&M framework should be broadly implemented to promote patient safety and accountability in GI training programs.
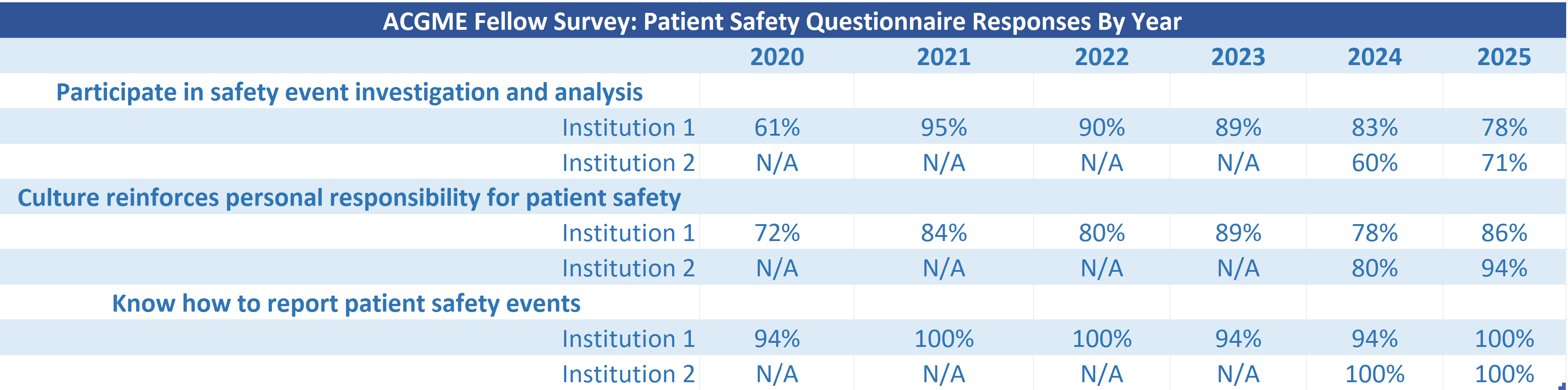
Figure: Table 1. Summary of Case Metrics and Interventions by Institution
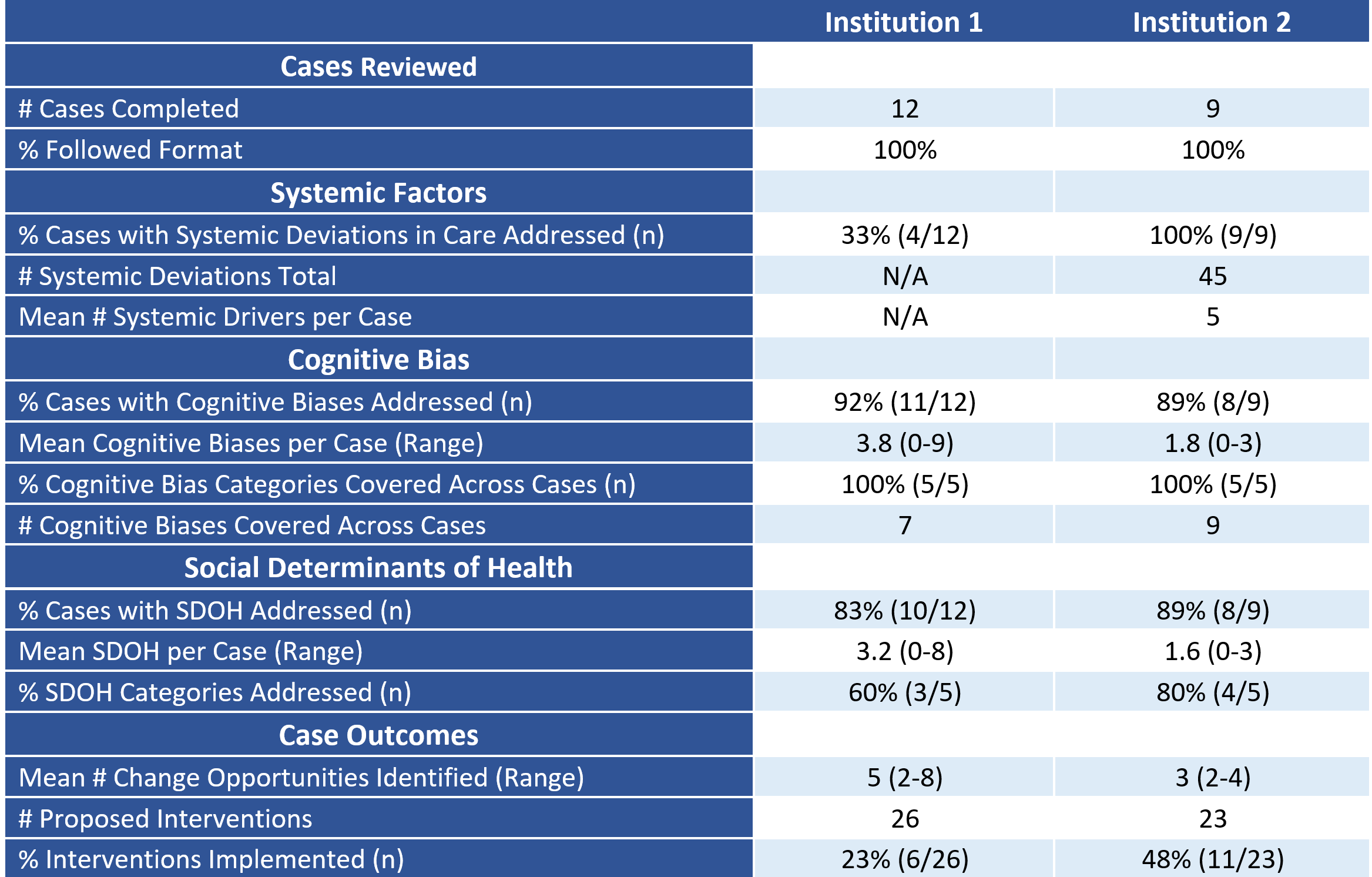
Figure: Table 2. ACGME Fellow Survey: Patient Safety Questionnaire Responses By Year
Disclosures:
Samantha Magier indicated no relevant financial relationships.
Daniel Stein: Fujifilm endoscopy – Consultant. Ovesco endoscopy – Grant/Research Support.
Ryan Flanagan indicated no relevant financial relationships.
Kunal Jajoo indicated no relevant financial relationships.
Michelle Hughes: Iterative Health – Consultant.
Samantha Magier, MD, MEng1, Daniel Stein, MD, MPH2, Ryan Flanagan, MD, MPH2, Kunal Jajoo, MD2, Michelle L. Hughes, MD3. P6175 - Transforming the Gastroenterology Morbidity and Mortality Conference: A Multicenter, Fellow-Led Approach to Systems Thinking, Equity, and Safety Culture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

