Tuesday Poster Session
Category: Practice Management
P6172 - Rising Pulmonary Embolism-Related Mortality and Healthcare Disparities Among Patients With Digestive Neoplasms in the United States (1999-2020): A Population-Based Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Muhammad Ahmed, MD
Henry Ford Health
Clinton Township, MI
Presenting Author(s)
Muhammad Ahmed, MD1, Muhammad Umer, MBBS2, Sarah Zaka, 3, Ahmed Faizan, MBBS3, Amir Hamza Khan, MBBS4, Faraz Iqbal. Khaskheli, 5, Bismah Azam Ali, MBBS6, Misbah Bibi, MBBS7
1Henry Ford Health, Clinton Township, MI; 2King Edward Medical University, Bellmawr, NJ; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 5Liaquat University of Medical and Health Science, Karachi, Sindh, Pakistan; 6Dow University of Health Sciences, Karachi, Sindh, Pakistan; 7Bahria University Health Sciences Campus, Karachi, Sindh, Pakistan
Introduction: Gastrointestinal (GI) malignancies are a significant cause of cancer-related mortality in the United States and are frequently associated with thromboembolic events. Pulmonary embolism (PE), in particular, remains an under-recognized contributor to the overall mortality. We aimed to investigate the long-term mortality patterns stratified by sex, race/ethnicity, urbanization, and U.S. census region
Methods: We performed a retrospective analysis of mortality data for adults with PE and GI malignancies using the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database from 1999 to 2020. ICD-10 codes [PE: I26; GI malignancies: C15–C26] were used to obtain deidentified patient data. Age-adjusted mortality rates (AAMR), annual percentage change (APC), and average annual percentage change (AAPC) were calculated using the Joinpoint regression program. Trends were analyzed for disparities among age, gender, race, U.S. census region, and level of urbanization.
Results: From 1999 to 2020, a total of 53,331 deaths were attributed to pulmonary embolism among patients with digestive neoplasms in the United States. The overall age-adjusted mortality rate (AAMR) was stable from 1999 to 2014 (APC: 0.43%), but increased sharply from 2014 to 2020 (APC: 5.17%).
The steepest rises were observed in females, with AAMR increasing from 2015 to 2020 (APC: 6.65%), and in African American individuals, from 2015 to 2020 (APC: 5.50%). Among Hispanic individuals, AAMR increased steadily from 1999 to 2020 (APC: 2.42%).
Geographically, large central metropolitan areas showed the fastest increase from 2017 to 2020 (APC: 8.85%), while noncore rural areas also experienced a significant rise from 2013 to 2020 (APC: 5.95%).
Tests for parallelism revealed significant differences in trends across sex (p=0.03), race (p=0.02), and level of urbanization (p=0.01).
Discussion: Our study demonstrates a significant rise in pulmonary embolism-related mortality among patients with digestive neoplasms in the United States in recent years, particularly after 2014. The increasing trends observed across sex, race, and geographic subgroups highlight widening disparities and the need for targeted prevention strategies. Ongoing efforts to improve risk assessment, early diagnosis, and thromboprophylaxis in this population are critical to reversing this concerning trend.
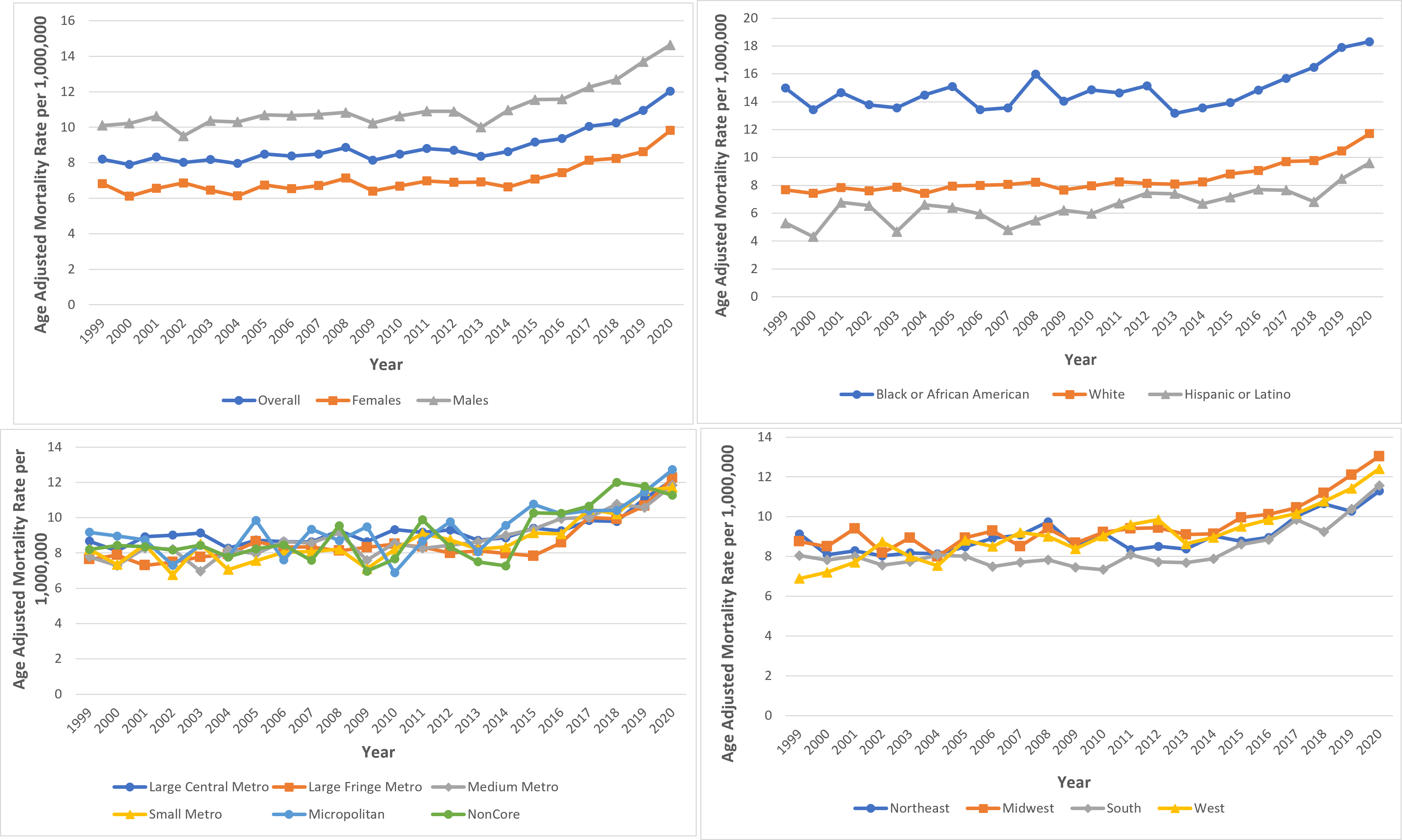
Figure: Trends in pulmonary embolism-related mortality among patients with digestive neoplasms in the United States, 1999–2020, stratified by (A) sex, (B) race/ethnicity, (C) urbanization level, and (D) U.S. census region. Rates are shown as age-adjusted mortality rates per 1,000,000 population.
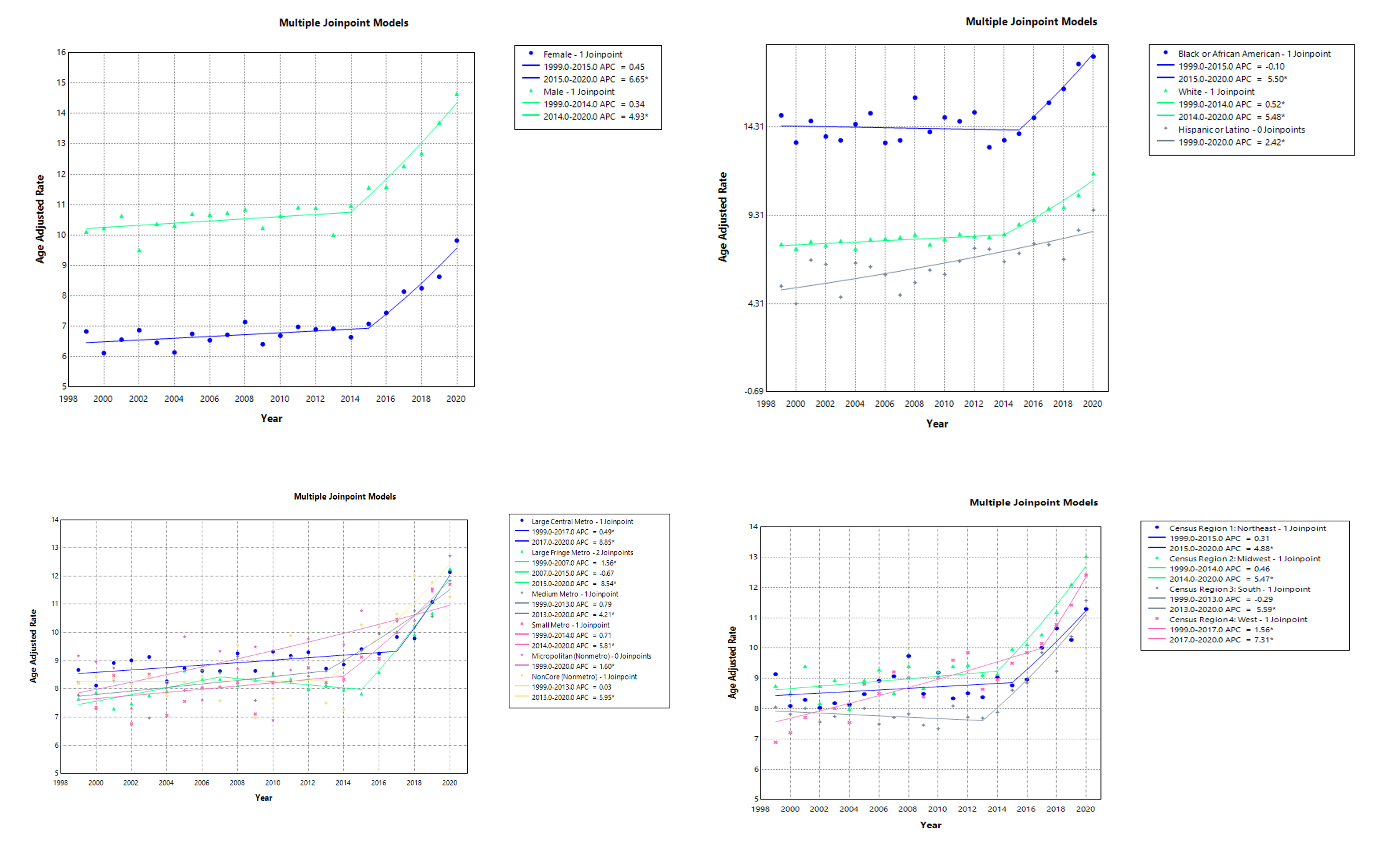
Figure: Join point regression analysis of pulmonary embolism-related mortality among patients with digestive neoplasms in the U.S. (1999–2020), stratified by sex, race/ethnicity, urbanization level, and census region.
Disclosures:
Muhammad Ahmed indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Sarah Zaka indicated no relevant financial relationships.
Ahmed Faizan indicated no relevant financial relationships.
Amir Hamza Khan indicated no relevant financial relationships.
Faraz Khaskheli indicated no relevant financial relationships.
Bismah Azam Ali indicated no relevant financial relationships.
Misbah Bibi indicated no relevant financial relationships.
Muhammad Ahmed, MD1, Muhammad Umer, MBBS2, Sarah Zaka, 3, Ahmed Faizan, MBBS3, Amir Hamza Khan, MBBS4, Faraz Iqbal. Khaskheli, 5, Bismah Azam Ali, MBBS6, Misbah Bibi, MBBS7. P6172 - Rising Pulmonary Embolism-Related Mortality and Healthcare Disparities Among Patients With Digestive Neoplasms in the United States (1999-2020): A Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Clinton Township, MI; 2King Edward Medical University, Bellmawr, NJ; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 5Liaquat University of Medical and Health Science, Karachi, Sindh, Pakistan; 6Dow University of Health Sciences, Karachi, Sindh, Pakistan; 7Bahria University Health Sciences Campus, Karachi, Sindh, Pakistan
Introduction: Gastrointestinal (GI) malignancies are a significant cause of cancer-related mortality in the United States and are frequently associated with thromboembolic events. Pulmonary embolism (PE), in particular, remains an under-recognized contributor to the overall mortality. We aimed to investigate the long-term mortality patterns stratified by sex, race/ethnicity, urbanization, and U.S. census region
Methods: We performed a retrospective analysis of mortality data for adults with PE and GI malignancies using the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database from 1999 to 2020. ICD-10 codes [PE: I26; GI malignancies: C15–C26] were used to obtain deidentified patient data. Age-adjusted mortality rates (AAMR), annual percentage change (APC), and average annual percentage change (AAPC) were calculated using the Joinpoint regression program. Trends were analyzed for disparities among age, gender, race, U.S. census region, and level of urbanization.
Results: From 1999 to 2020, a total of 53,331 deaths were attributed to pulmonary embolism among patients with digestive neoplasms in the United States. The overall age-adjusted mortality rate (AAMR) was stable from 1999 to 2014 (APC: 0.43%), but increased sharply from 2014 to 2020 (APC: 5.17%).
The steepest rises were observed in females, with AAMR increasing from 2015 to 2020 (APC: 6.65%), and in African American individuals, from 2015 to 2020 (APC: 5.50%). Among Hispanic individuals, AAMR increased steadily from 1999 to 2020 (APC: 2.42%).
Geographically, large central metropolitan areas showed the fastest increase from 2017 to 2020 (APC: 8.85%), while noncore rural areas also experienced a significant rise from 2013 to 2020 (APC: 5.95%).
Tests for parallelism revealed significant differences in trends across sex (p=0.03), race (p=0.02), and level of urbanization (p=0.01).
Discussion: Our study demonstrates a significant rise in pulmonary embolism-related mortality among patients with digestive neoplasms in the United States in recent years, particularly after 2014. The increasing trends observed across sex, race, and geographic subgroups highlight widening disparities and the need for targeted prevention strategies. Ongoing efforts to improve risk assessment, early diagnosis, and thromboprophylaxis in this population are critical to reversing this concerning trend.
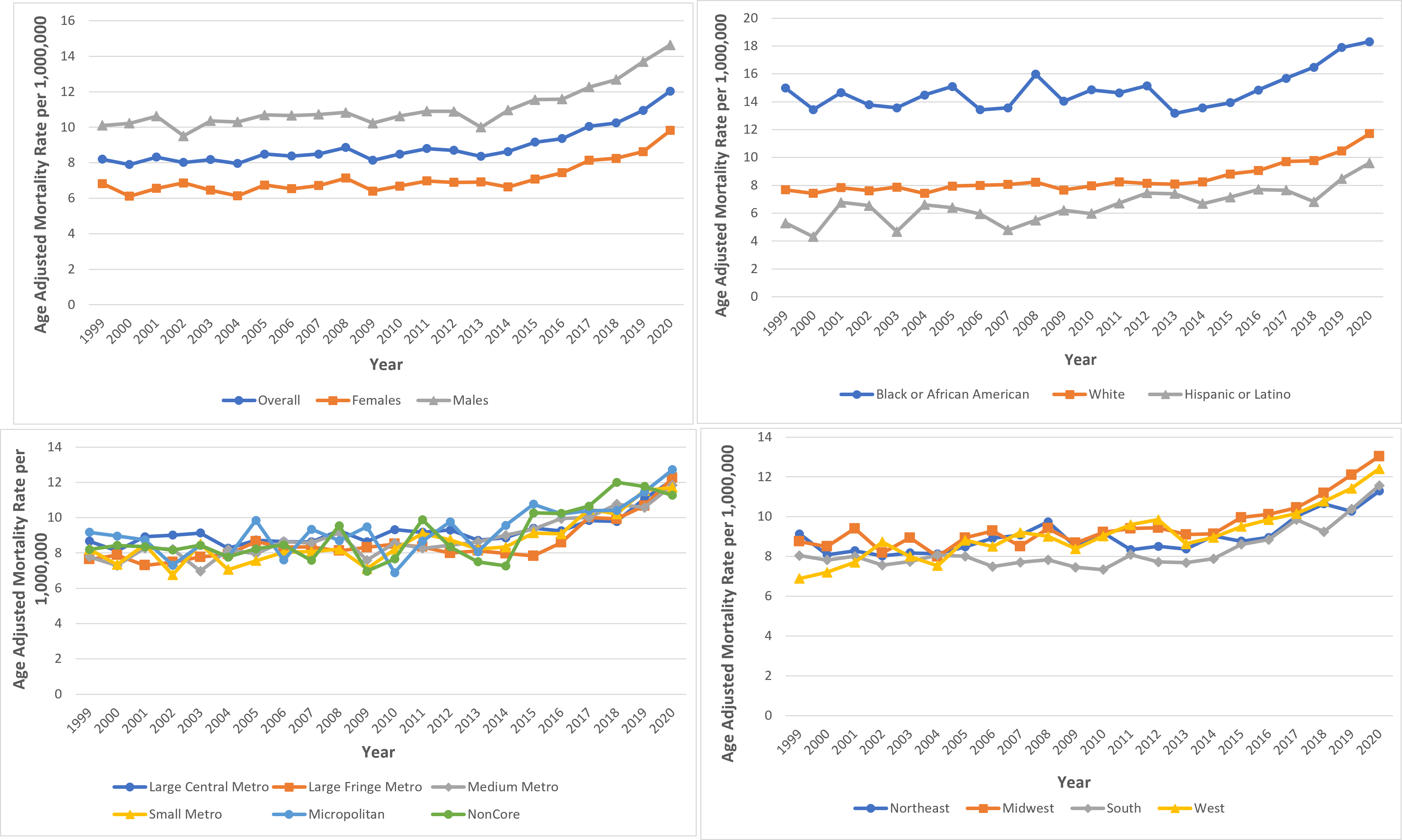
Figure: Trends in pulmonary embolism-related mortality among patients with digestive neoplasms in the United States, 1999–2020, stratified by (A) sex, (B) race/ethnicity, (C) urbanization level, and (D) U.S. census region. Rates are shown as age-adjusted mortality rates per 1,000,000 population.
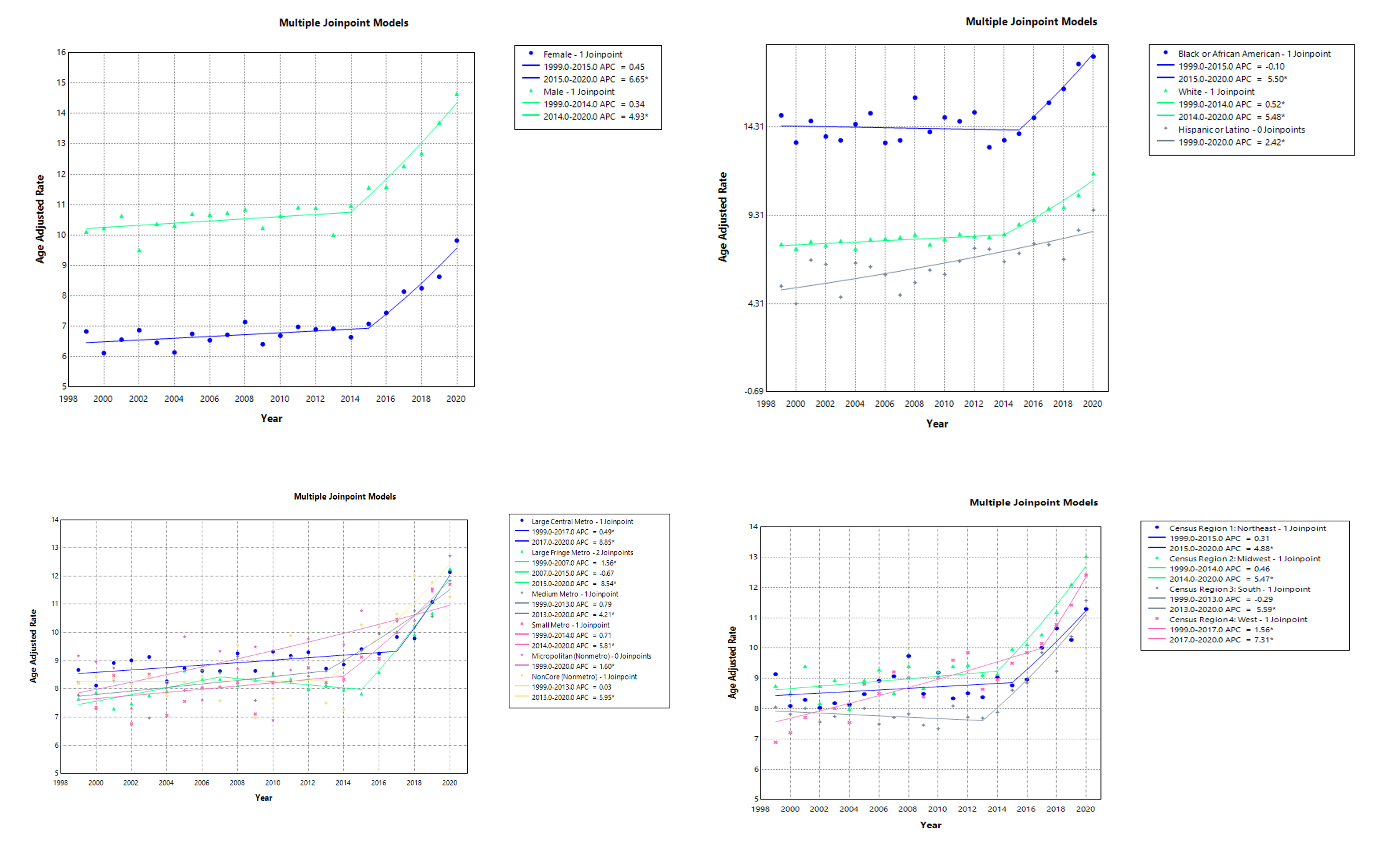
Figure: Join point regression analysis of pulmonary embolism-related mortality among patients with digestive neoplasms in the U.S. (1999–2020), stratified by sex, race/ethnicity, urbanization level, and census region.
Disclosures:
Muhammad Ahmed indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Sarah Zaka indicated no relevant financial relationships.
Ahmed Faizan indicated no relevant financial relationships.
Amir Hamza Khan indicated no relevant financial relationships.
Faraz Khaskheli indicated no relevant financial relationships.
Bismah Azam Ali indicated no relevant financial relationships.
Misbah Bibi indicated no relevant financial relationships.
Muhammad Ahmed, MD1, Muhammad Umer, MBBS2, Sarah Zaka, 3, Ahmed Faizan, MBBS3, Amir Hamza Khan, MBBS4, Faraz Iqbal. Khaskheli, 5, Bismah Azam Ali, MBBS6, Misbah Bibi, MBBS7. P6172 - Rising Pulmonary Embolism-Related Mortality and Healthcare Disparities Among Patients With Digestive Neoplasms in the United States (1999-2020): A Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
