Tuesday Poster Session
Category: Stomach and Spleen
P6327 - Diabetes Mellitus Transforms Gastroparesis Outcomes: A National Analysis of Mortality, Healthcare Utilization, and Cost Burden
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Usama Sakhawat, MD
United Health Services, Wilson Medical Center
BINGHAMTON, NY
Presenting Author(s)
Usama Sakhawat, MD1, Najam Gohar, MBBS2, Muhammad Junaid Zahid, MBBS3, Taha Muhammad Hannan, MBBS3, Haziq Ahmad, MBBS4, Abdul Mateen, MBBS3, Muhammad Usman Azeem, MBBS3, Faizan A. Malik, MD5, Tehmasp Rehman Mirza, MBBS6, Rama Hassan, MBBS7, Abdul Subhan Talpur, MD1, Moheudin Khan, MD1, Ahmed Shehadah, MD8, Khandokar Talib, MD9, Toseef Javaid, MD1
1United Health Services, Wilson Medical Center, Johnson City, NY; 2Ameer Ud Din Medical College, Lahore, NY; 3Ameer Ud Din Medical College, Lahore, Punjab, Pakistan; 4Sheikh Khalifa Bin Zayed Al Nahyan Medical and Dental College, Lahore, Lahore, Punjab, Pakistan; 5Duke University, Durham, NC; 6MBBS, Lahore, Punjab, Pakistan; 7Akhtar Saeed Medical and Dental College, Lahore, Binghamton, NY; 8United Health Services, Wilson Medical Center, Binghamton, NY; 9United Health Services, Johnson City, NY
Introduction: Gastroparesis (GP), a chronic gastric motility disorder, is frequently linked with diabetes mellitus (DM), potentially altering both its etiology and hospitalization outcomes. Patients with a feeding tube associated GP represent a distinct high-risk subgroup. We aimed to assess associations between diabetes and in-hospital outcomes among patients hospitalized with GP, including those with feeding tubes.
Methods: We analyzed the National Inpatient Sample (2017 to 2022) for GP hospitalizations, stratified by diabetes status. Multivariable regression models were adjusted for demographic, socioeconomic, and clinical factors using STATA 17. Outcomes were reported as adjusted coefficients for continuous variables and adjusted odds ratios (aORs) for binary outcomes.
Results: Diabetic gastroparesis patients were predominantly male (78.97% vs 21.03%), older (77.86% ages 40-59), and non-White including Black (85.21%) and Hispanic (82.42%) patients (all p< 0.001). They were more frequently in the lowest income quartile (78.73%).
Comorbidity burden was substantially higher in diabetic patients: hypertension (73.69%), obesity (79.88%), chronic kidney disease (89.28%), congestive heart failure (85.26%), stroke (81.76%), and myocardial infarction (85.65%) (all p< 0.001). Despite this elevated burden, diabetic patients had superior outcomes.
Mortality was significantly reduced (aOR 0.45, 95% CI 0.42-0.49, p< 0.0001), hospital stay shortened by 2.48 days (95% CI -2.60 to -2.36, p< 0.0001), and charges decreased by $29,798 (95% CI -$31,426 to -$28,170, p< 0.0001). Among feeding tube patients with DM, mortality remained significantly lower as well (aOR 0.24, 95% CI 0.22-0.27, p< 0.0001).
Discussion: Gastroparesis with diabetes paradoxically demonstrates superior survival outcomes despite increased comorbidity burden. Diabetic patients experience shorter hospitalizations and reduced healthcare costs. These findings suggest diabetes may confer protective mechanisms or reflect improved disease management strategies. Healthcare resource allocation should consider these differential outcomes. Further research should investigate underlying biological and care delivery factors driving these counterintuitive results.
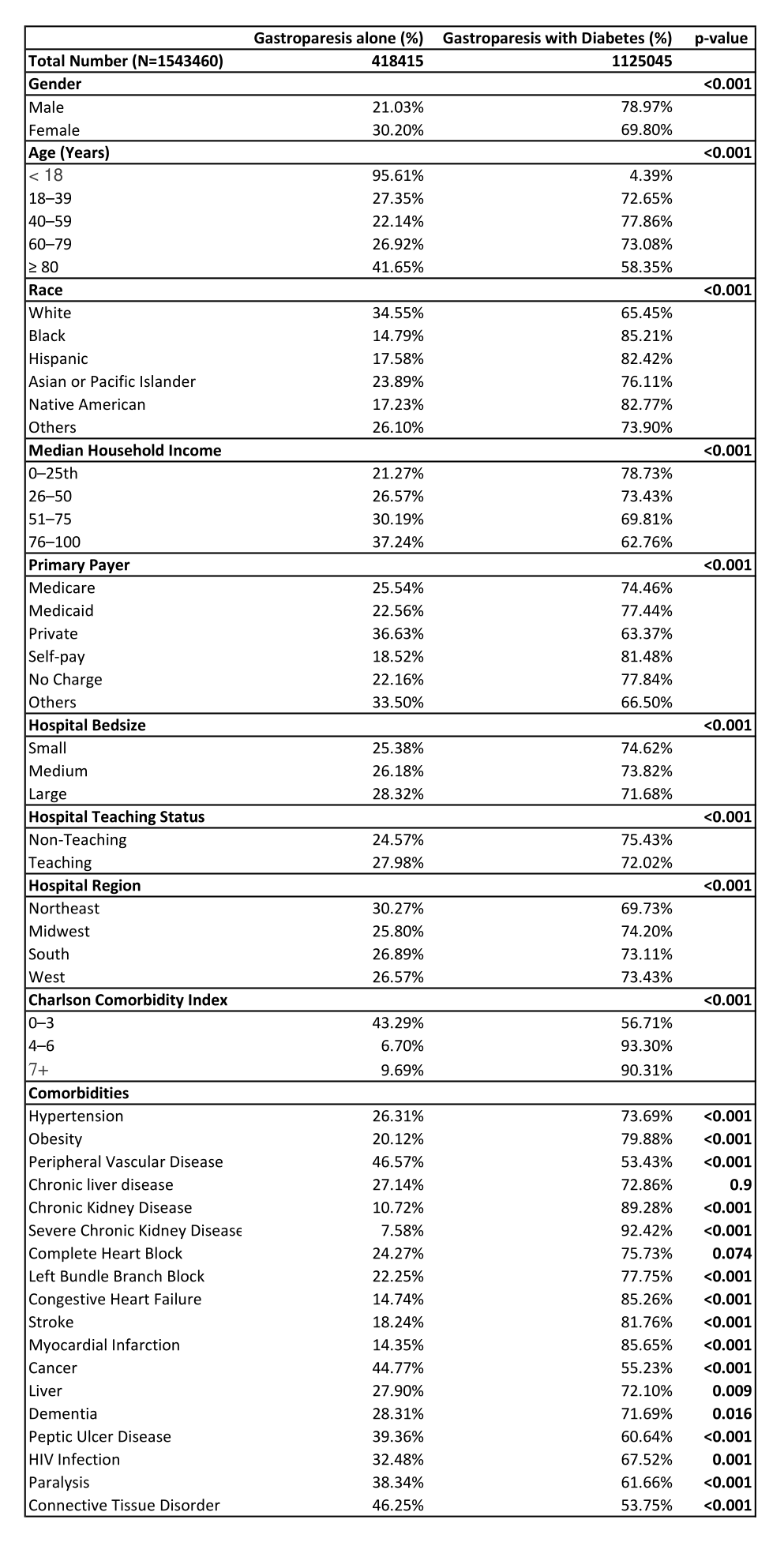
Figure: Baseline Characteristics
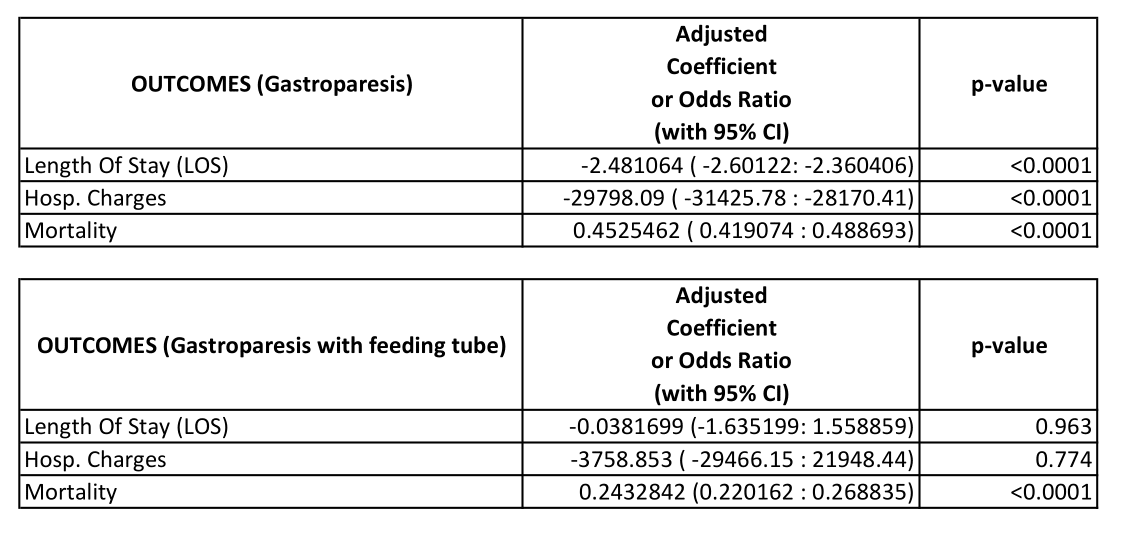
Figure: Adjusted Outcomes
Disclosures:
Usama Sakhawat indicated no relevant financial relationships.
Najam Gohar indicated no relevant financial relationships.
Muhammad Junaid Zahid indicated no relevant financial relationships.
Taha Muhammad Hannan indicated no relevant financial relationships.
Haziq Ahmad indicated no relevant financial relationships.
Abdul Mateen indicated no relevant financial relationships.
Muhammad Usman Azeem indicated no relevant financial relationships.
Faizan A. Malik indicated no relevant financial relationships.
Tehmasp Rehman Mirza indicated no relevant financial relationships.
Rama Hassan indicated no relevant financial relationships.
Abdul Subhan Talpur indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Usama Sakhawat, MD1, Najam Gohar, MBBS2, Muhammad Junaid Zahid, MBBS3, Taha Muhammad Hannan, MBBS3, Haziq Ahmad, MBBS4, Abdul Mateen, MBBS3, Muhammad Usman Azeem, MBBS3, Faizan A. Malik, MD5, Tehmasp Rehman Mirza, MBBS6, Rama Hassan, MBBS7, Abdul Subhan Talpur, MD1, Moheudin Khan, MD1, Ahmed Shehadah, MD8, Khandokar Talib, MD9, Toseef Javaid, MD1. P6327 - Diabetes Mellitus Transforms Gastroparesis Outcomes: A National Analysis of Mortality, Healthcare Utilization, and Cost Burden, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Johnson City, NY; 2Ameer Ud Din Medical College, Lahore, NY; 3Ameer Ud Din Medical College, Lahore, Punjab, Pakistan; 4Sheikh Khalifa Bin Zayed Al Nahyan Medical and Dental College, Lahore, Lahore, Punjab, Pakistan; 5Duke University, Durham, NC; 6MBBS, Lahore, Punjab, Pakistan; 7Akhtar Saeed Medical and Dental College, Lahore, Binghamton, NY; 8United Health Services, Wilson Medical Center, Binghamton, NY; 9United Health Services, Johnson City, NY
Introduction: Gastroparesis (GP), a chronic gastric motility disorder, is frequently linked with diabetes mellitus (DM), potentially altering both its etiology and hospitalization outcomes. Patients with a feeding tube associated GP represent a distinct high-risk subgroup. We aimed to assess associations between diabetes and in-hospital outcomes among patients hospitalized with GP, including those with feeding tubes.
Methods: We analyzed the National Inpatient Sample (2017 to 2022) for GP hospitalizations, stratified by diabetes status. Multivariable regression models were adjusted for demographic, socioeconomic, and clinical factors using STATA 17. Outcomes were reported as adjusted coefficients for continuous variables and adjusted odds ratios (aORs) for binary outcomes.
Results: Diabetic gastroparesis patients were predominantly male (78.97% vs 21.03%), older (77.86% ages 40-59), and non-White including Black (85.21%) and Hispanic (82.42%) patients (all p< 0.001). They were more frequently in the lowest income quartile (78.73%).
Comorbidity burden was substantially higher in diabetic patients: hypertension (73.69%), obesity (79.88%), chronic kidney disease (89.28%), congestive heart failure (85.26%), stroke (81.76%), and myocardial infarction (85.65%) (all p< 0.001). Despite this elevated burden, diabetic patients had superior outcomes.
Mortality was significantly reduced (aOR 0.45, 95% CI 0.42-0.49, p< 0.0001), hospital stay shortened by 2.48 days (95% CI -2.60 to -2.36, p< 0.0001), and charges decreased by $29,798 (95% CI -$31,426 to -$28,170, p< 0.0001). Among feeding tube patients with DM, mortality remained significantly lower as well (aOR 0.24, 95% CI 0.22-0.27, p< 0.0001).
Discussion: Gastroparesis with diabetes paradoxically demonstrates superior survival outcomes despite increased comorbidity burden. Diabetic patients experience shorter hospitalizations and reduced healthcare costs. These findings suggest diabetes may confer protective mechanisms or reflect improved disease management strategies. Healthcare resource allocation should consider these differential outcomes. Further research should investigate underlying biological and care delivery factors driving these counterintuitive results.
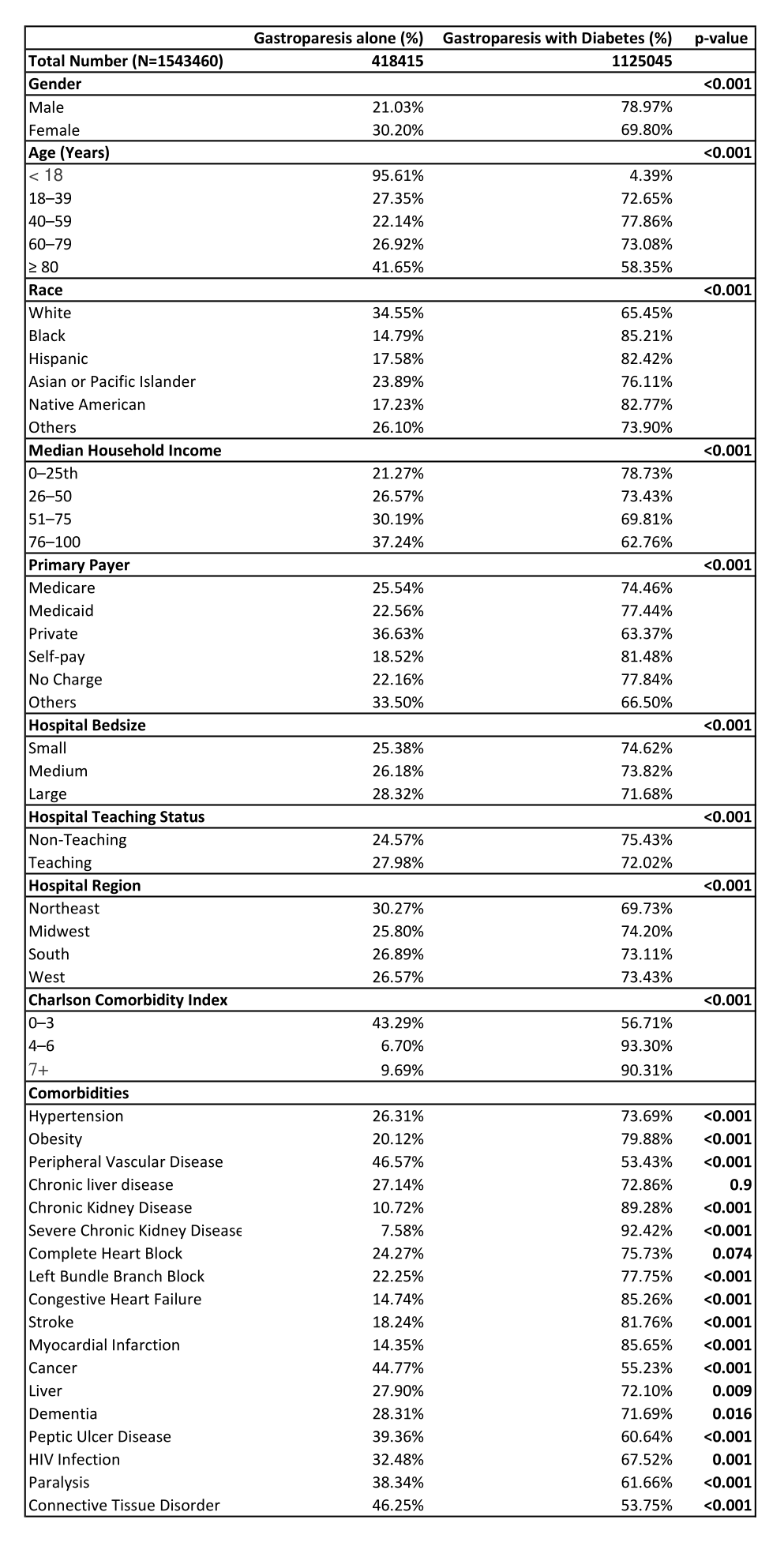
Figure: Baseline Characteristics
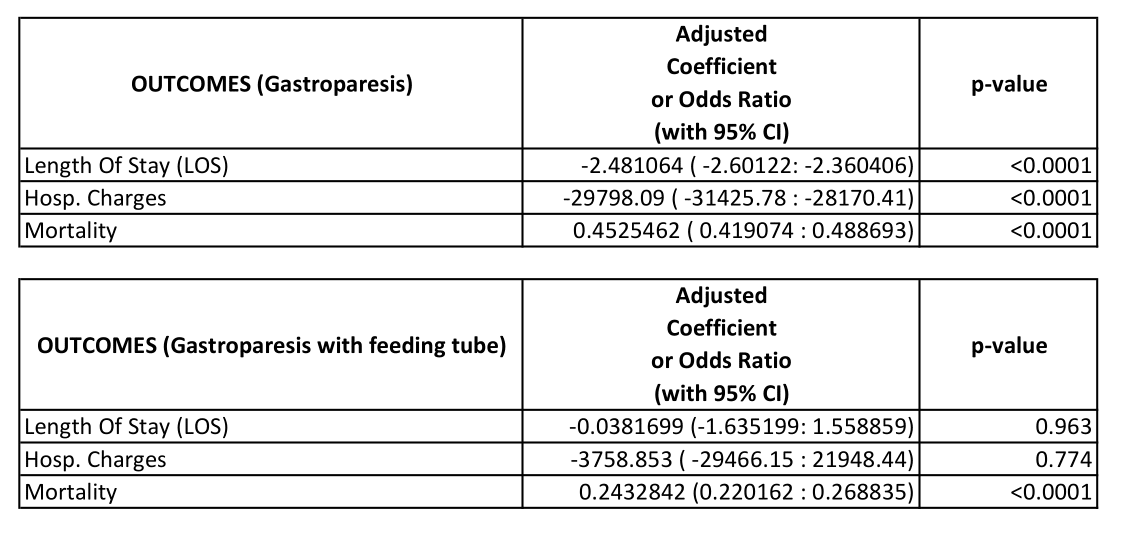
Figure: Adjusted Outcomes
Disclosures:
Usama Sakhawat indicated no relevant financial relationships.
Najam Gohar indicated no relevant financial relationships.
Muhammad Junaid Zahid indicated no relevant financial relationships.
Taha Muhammad Hannan indicated no relevant financial relationships.
Haziq Ahmad indicated no relevant financial relationships.
Abdul Mateen indicated no relevant financial relationships.
Muhammad Usman Azeem indicated no relevant financial relationships.
Faizan A. Malik indicated no relevant financial relationships.
Tehmasp Rehman Mirza indicated no relevant financial relationships.
Rama Hassan indicated no relevant financial relationships.
Abdul Subhan Talpur indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Usama Sakhawat, MD1, Najam Gohar, MBBS2, Muhammad Junaid Zahid, MBBS3, Taha Muhammad Hannan, MBBS3, Haziq Ahmad, MBBS4, Abdul Mateen, MBBS3, Muhammad Usman Azeem, MBBS3, Faizan A. Malik, MD5, Tehmasp Rehman Mirza, MBBS6, Rama Hassan, MBBS7, Abdul Subhan Talpur, MD1, Moheudin Khan, MD1, Ahmed Shehadah, MD8, Khandokar Talib, MD9, Toseef Javaid, MD1. P6327 - Diabetes Mellitus Transforms Gastroparesis Outcomes: A National Analysis of Mortality, Healthcare Utilization, and Cost Burden, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
