Tuesday Poster Session
Category: Liver
P6133 - Streptococcus constellatus Pyogenic Liver Abscess Resembling a Neoplastic Lesion: A Case Review
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KA
Kamal Akbar, MD
Larkin Community Hospital
South Miami, FL
Presenting Author(s)
Martha Arevalo-Mora, MD1, Kamal Akbar, MD1, Airton Pinheiro-Meneses, MD1, Aaron Perez-Castaneda, DO1, Natalia Martin, DO1, Karthik Mohan, DO2
1Larkin Community Hospital, South Miami, FL; 2Larkin Community Hospital, Hialeah, FL
Introduction: Pyogenic liver abscesses (PLAs) are a common cause of visceral abscesses, typically arising from biliary disease and represent an annual incidence of 2.3 cases per 100,000, being more prevalent in men than women (3.3 vs 1.3). Major risk factors include diabetes mellitus, hepatobiliopancreatic disease, liver transplantation, and chronic PPI use. Most PLAs are polymicrobial, having among the most common pathogens the Streptococcus milleri group species (S. anginosus, S. constellatus, S. intermedius). We report a case of a large liver abscess caused by Streptococcus constellatus, initially mistaken for a neoplastic lesion.
Case Description/
Methods: A 68-year-old homeless male with a 10-year history of heavy alcohol use disorder who presented with RUQ abdominal pain, unintentional weight loss, and fatigue. Initial labs revealed Hb 8.6, INR 1.7, Na 128, Crea 1.2, AST 72, ALP 193, and TBIL 5.9. CT scan showed a multiseptated 12.0 x 9.9 x 14.4 cm liver lesion; MRCP revealed a well-defined, T2 hyperintense 14.4 x 9.8 x 15.9 cm hepatic lesion with restricted diffusion concerning for neoplasia. US-guided liver biopsy histopathology showed inflammatory and necrotic tissue consistent with abscess.
CT-guided percutaneous liver abscess drainage with a 14F pigtail catheter yielded copious blood-tinged pus. Cultures grew Streptococcus constellatus. Antibiotic therapy was narrowed to Rocephin and Flagyl. Despite these interventions, the patient passed after a second cardiac arrest.
Discussion: Complex cystic lesions, including PLAs, can sometimes mimic malignancy, specially when exhibiting solid components with cystic areas. PLAs pathogenesis often involve portal vein pyemia, arising from bowel leakage, peritonitis, or biliary tract infections and monomicrobial infections with streptococcal or staphylococcal species which should prompt evaluation for other sources, such as infectious endocarditis. S. anginosus group is frequently associated with liver abscesses alongside Enterobacteriaceae or gut anaerobes. The presence of S. constellatus in the liver without abdominal pathology, may suggest an occult GI malignancy. This case poses the diagnostic challenge, particularly in the setting of inespecific symptoms. Despite imaging suggesting malignancy, the infectious nature of the lesion was only confirmed with biopsy. Timely antibiotic therapy is critical and this case highlighs the importance of including infectious causes in the differential of large hepatic lesions.
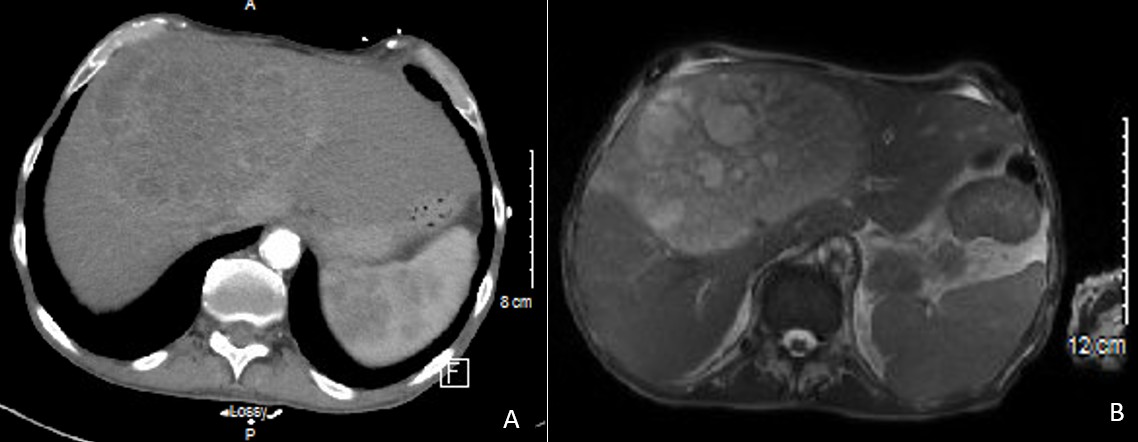
Figure: Figure 1: A. Axial CT scan showing a multiseptated 12.0 x 9.9 x 14.4 cm liver lesion. B. Axial MRCP portrayed a well-defined, segment 4, 14.4 x 9.8 x 15.9 cm T2 hyperintense liver lesion, with restricted diffusion, suggestive of malignancy.
Disclosures:
Martha Arevalo-Mora indicated no relevant financial relationships.
Kamal Akbar indicated no relevant financial relationships.
Airton Pinheiro-Meneses indicated no relevant financial relationships.
Aaron Perez-Castaneda indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Martha Arevalo-Mora, MD1, Kamal Akbar, MD1, Airton Pinheiro-Meneses, MD1, Aaron Perez-Castaneda, DO1, Natalia Martin, DO1, Karthik Mohan, DO2. P6133 - <i>Streptococcus constellatus</i> Pyogenic Liver Abscess Resembling a Neoplastic Lesion: A Case Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Larkin Community Hospital, South Miami, FL; 2Larkin Community Hospital, Hialeah, FL
Introduction: Pyogenic liver abscesses (PLAs) are a common cause of visceral abscesses, typically arising from biliary disease and represent an annual incidence of 2.3 cases per 100,000, being more prevalent in men than women (3.3 vs 1.3). Major risk factors include diabetes mellitus, hepatobiliopancreatic disease, liver transplantation, and chronic PPI use. Most PLAs are polymicrobial, having among the most common pathogens the Streptococcus milleri group species (S. anginosus, S. constellatus, S. intermedius). We report a case of a large liver abscess caused by Streptococcus constellatus, initially mistaken for a neoplastic lesion.
Case Description/
Methods: A 68-year-old homeless male with a 10-year history of heavy alcohol use disorder who presented with RUQ abdominal pain, unintentional weight loss, and fatigue. Initial labs revealed Hb 8.6, INR 1.7, Na 128, Crea 1.2, AST 72, ALP 193, and TBIL 5.9. CT scan showed a multiseptated 12.0 x 9.9 x 14.4 cm liver lesion; MRCP revealed a well-defined, T2 hyperintense 14.4 x 9.8 x 15.9 cm hepatic lesion with restricted diffusion concerning for neoplasia. US-guided liver biopsy histopathology showed inflammatory and necrotic tissue consistent with abscess.
CT-guided percutaneous liver abscess drainage with a 14F pigtail catheter yielded copious blood-tinged pus. Cultures grew Streptococcus constellatus. Antibiotic therapy was narrowed to Rocephin and Flagyl. Despite these interventions, the patient passed after a second cardiac arrest.
Discussion: Complex cystic lesions, including PLAs, can sometimes mimic malignancy, specially when exhibiting solid components with cystic areas. PLAs pathogenesis often involve portal vein pyemia, arising from bowel leakage, peritonitis, or biliary tract infections and monomicrobial infections with streptococcal or staphylococcal species which should prompt evaluation for other sources, such as infectious endocarditis. S. anginosus group is frequently associated with liver abscesses alongside Enterobacteriaceae or gut anaerobes. The presence of S. constellatus in the liver without abdominal pathology, may suggest an occult GI malignancy. This case poses the diagnostic challenge, particularly in the setting of inespecific symptoms. Despite imaging suggesting malignancy, the infectious nature of the lesion was only confirmed with biopsy. Timely antibiotic therapy is critical and this case highlighs the importance of including infectious causes in the differential of large hepatic lesions.
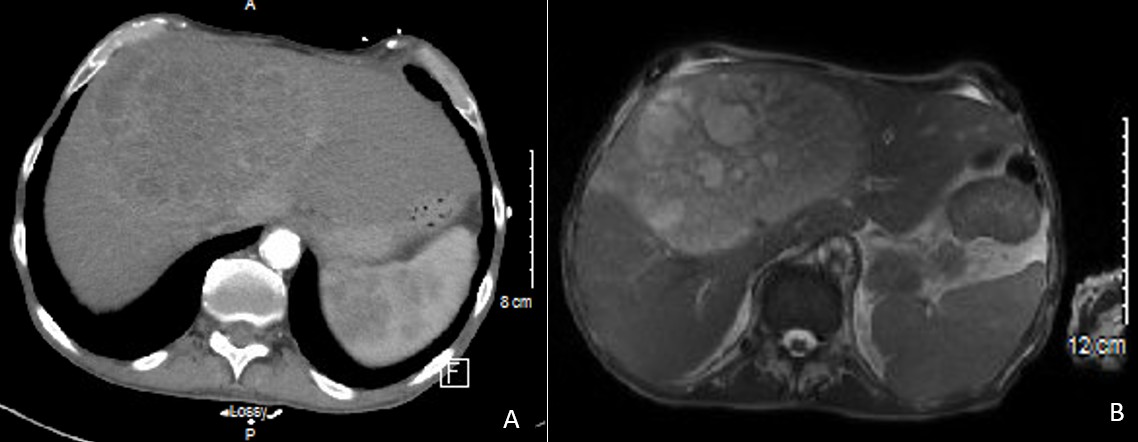
Figure: Figure 1: A. Axial CT scan showing a multiseptated 12.0 x 9.9 x 14.4 cm liver lesion. B. Axial MRCP portrayed a well-defined, segment 4, 14.4 x 9.8 x 15.9 cm T2 hyperintense liver lesion, with restricted diffusion, suggestive of malignancy.
Disclosures:
Martha Arevalo-Mora indicated no relevant financial relationships.
Kamal Akbar indicated no relevant financial relationships.
Airton Pinheiro-Meneses indicated no relevant financial relationships.
Aaron Perez-Castaneda indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Martha Arevalo-Mora, MD1, Kamal Akbar, MD1, Airton Pinheiro-Meneses, MD1, Aaron Perez-Castaneda, DO1, Natalia Martin, DO1, Karthik Mohan, DO2. P6133 - <i>Streptococcus constellatus</i> Pyogenic Liver Abscess Resembling a Neoplastic Lesion: A Case Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
