Tuesday Poster Session
Category: Liver
P6130 - A Rare Case of Budd-Chiari Syndrome Secondary to Portal Vein Thrombosis Requiring Direct Intrahepatic Portosystemic Shunt (DIPS) for Refractory Ascites
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Luis A. Morales, MD, MS
Tulane University
New Orleans, LA
Presenting Author(s)
Luis A.. Morales, MD, MS, Matthew B.. Alias, MD, MS, Abhijith Atkuru, MD, Giuseppe Morelli, MD
Tulane University, New Orleans, LA
Introduction: Budd-Chiari syndrome (BCS) is defined as hepatic venous outflow obstruction, regardless of the underlying mechanism. It is commonly caused by hepatic vein thrombosis and associated to prothrombotic conditions. It has an incidence of 0.5–2 cases per million in Western countries. BCS in the setting of extensive portal vein thrombosis is exceedingly rare. Management consists of a step-up approach starting with anticoagulation, and may escalate to transjugular intrahepatic portosystemic shunt (TIPS) in severe cases.
Case Description/
Methods: A 47-year-old female with hypertension, decompensated cirrhosis, and uncontrolled polycythemia vera presented with abdominal pain, nausea, and shortness of breath. Physical exam remarkable for somnolence, crackles, abdominal distension with fluid wave, and bilateral lower extremity edema. Labs showed leukocytosis (WBC 32), thrombocytosis (PLT 838), hyponatremia (Na 131), elevated BUN (29), Cr (1.13) and hyperammonemia (120). Liver enzymes were near normal (AST 27, ALT 14) with elevated ALP (185) and hyperbilirubinemia (3.5). PT (20) INR(1.7). Large-volume paracentesis showed SAAG >1.1. Abdominal CT scan revealed ascites, hepatomegaly with mottled appearance, caudate lobe enlargement, and diminutive inferior vena cava (IVC), suggesting BCS. Also noted were splenomegaly, collateral formations, and a 9mm non-occlusive portal vein thrombus. The patient was treated initially with diuretics and anticoagulation without clinical improvement. Interventional radiology was consulted for TIPS, however the extensive portal vein thrombosis made it complicated. The patient underwent direct intrahepatic portosystemic shunt (DIPS) with a pre-procedure hepatic venous pressure gradient of 38 mmHg and 8 mmHg post-procedure.
Discussion: This case highlights poorly controlled polycythemia vera as a major risk factor for extensive splanchnic venous thrombosis leading to BCS. In this patient, financial barriers to accessing appropriate anticoagulation contributed significantly to disease progression and decompensation. When medical therapy fails, a multidisciplinary approach is warranted, often involving TIPS. This procedure creates a bypass between the portal and hepatic veins via the transjugular route. However, when hepatic vein access is not feasible, DIPS offers an alternative by connecting the portal vein directly to the inferior vena cava through the liver parenchyma. DIPS is a viable option for portal decompression and symptom relief in select patients with advanced disease.
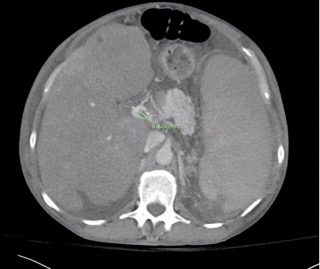
Figure: Notable non-occlusive 9mm portal vein thrombus. Enlarged and mottled appearance of liver, diminutive IVC, and splenomegaly. Findings suggestive of Budd-Chiari syndrome.
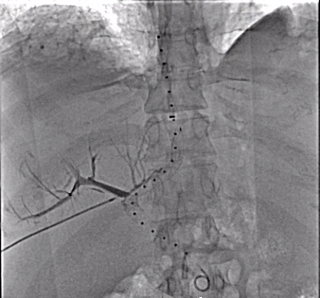
Figure: Fluoroscopic image post-DIPS placement demonstrating successful creation of a direct intrahepatic shunt between the portal vein and IVC.
Disclosures:
Luis Morales indicated no relevant financial relationships.
Matthew Alias indicated no relevant financial relationships.
Abhijith Atkuru indicated no relevant financial relationships.
Giuseppe Morelli indicated no relevant financial relationships.
Luis A.. Morales, MD, MS, Matthew B.. Alias, MD, MS, Abhijith Atkuru, MD, Giuseppe Morelli, MD. P6130 - A Rare Case of Budd-Chiari Syndrome Secondary to Portal Vein Thrombosis Requiring Direct Intrahepatic Portosystemic Shunt (DIPS) for Refractory Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Tulane University, New Orleans, LA
Introduction: Budd-Chiari syndrome (BCS) is defined as hepatic venous outflow obstruction, regardless of the underlying mechanism. It is commonly caused by hepatic vein thrombosis and associated to prothrombotic conditions. It has an incidence of 0.5–2 cases per million in Western countries. BCS in the setting of extensive portal vein thrombosis is exceedingly rare. Management consists of a step-up approach starting with anticoagulation, and may escalate to transjugular intrahepatic portosystemic shunt (TIPS) in severe cases.
Case Description/
Methods: A 47-year-old female with hypertension, decompensated cirrhosis, and uncontrolled polycythemia vera presented with abdominal pain, nausea, and shortness of breath. Physical exam remarkable for somnolence, crackles, abdominal distension with fluid wave, and bilateral lower extremity edema. Labs showed leukocytosis (WBC 32), thrombocytosis (PLT 838), hyponatremia (Na 131), elevated BUN (29), Cr (1.13) and hyperammonemia (120). Liver enzymes were near normal (AST 27, ALT 14) with elevated ALP (185) and hyperbilirubinemia (3.5). PT (20) INR(1.7). Large-volume paracentesis showed SAAG >1.1. Abdominal CT scan revealed ascites, hepatomegaly with mottled appearance, caudate lobe enlargement, and diminutive inferior vena cava (IVC), suggesting BCS. Also noted were splenomegaly, collateral formations, and a 9mm non-occlusive portal vein thrombus. The patient was treated initially with diuretics and anticoagulation without clinical improvement. Interventional radiology was consulted for TIPS, however the extensive portal vein thrombosis made it complicated. The patient underwent direct intrahepatic portosystemic shunt (DIPS) with a pre-procedure hepatic venous pressure gradient of 38 mmHg and 8 mmHg post-procedure.
Discussion: This case highlights poorly controlled polycythemia vera as a major risk factor for extensive splanchnic venous thrombosis leading to BCS. In this patient, financial barriers to accessing appropriate anticoagulation contributed significantly to disease progression and decompensation. When medical therapy fails, a multidisciplinary approach is warranted, often involving TIPS. This procedure creates a bypass between the portal and hepatic veins via the transjugular route. However, when hepatic vein access is not feasible, DIPS offers an alternative by connecting the portal vein directly to the inferior vena cava through the liver parenchyma. DIPS is a viable option for portal decompression and symptom relief in select patients with advanced disease.
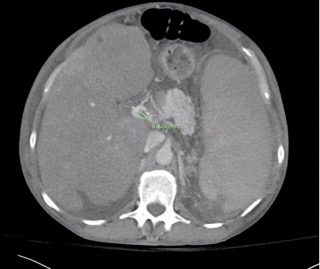
Figure: Notable non-occlusive 9mm portal vein thrombus. Enlarged and mottled appearance of liver, diminutive IVC, and splenomegaly. Findings suggestive of Budd-Chiari syndrome.
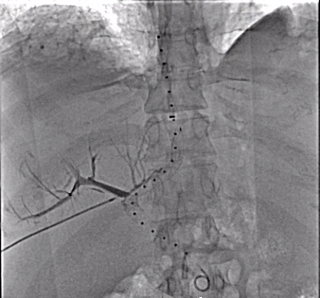
Figure: Fluoroscopic image post-DIPS placement demonstrating successful creation of a direct intrahepatic shunt between the portal vein and IVC.
Disclosures:
Luis Morales indicated no relevant financial relationships.
Matthew Alias indicated no relevant financial relationships.
Abhijith Atkuru indicated no relevant financial relationships.
Giuseppe Morelli indicated no relevant financial relationships.
Luis A.. Morales, MD, MS, Matthew B.. Alias, MD, MS, Abhijith Atkuru, MD, Giuseppe Morelli, MD. P6130 - A Rare Case of Budd-Chiari Syndrome Secondary to Portal Vein Thrombosis Requiring Direct Intrahepatic Portosystemic Shunt (DIPS) for Refractory Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
