Tuesday Poster Session
Category: Liver
P6129 - Unclassified Hepatic Adenoma in the Setting of Hepatic Adenomatosis: A Case Report With Molecular Characterization
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Franklin Liu, MD
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Franklin Liu, MD1, Sabrina Ho, MD1, Samuel Cheong, DO1, Kai Tey, MBBS2
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona Tucson, Tucson, AZ
Introduction: Hepatic adenomatosis was first described by Flejou et al in 1985 as the presence of ten or more hepatocellular adenomas (HCAs) in otherwise normal liver parenchyma. HCAs are benign epithelial liver tumors that can be subclassified into four major subtypes: hepatocyte nuclear factor-1α (HNF-1α) inactivated, β-catenin activated, inflammatory, and unclassified. Although typically benign, HCAs carry a risk of hemorrhage and malignant transformation into hepatocellular carcinoma (HCC), particularly in certain subtypes or when lesions are large or multifocal.
Case Description/
Methods: A 24-year-old female with a history of class III obesity, Ehlers-Danlos syndrome, systemic lupus erythematosus, eosinophilic esophagitis, asthma, irritable bowel syndrome, on oral contraception presented with chronic abdominal pain, diarrhea, and episodes of jaundice. Laboratory evaluation was unremarkable. MRI of the abdomen revealed 13 bilobar hepatic lesions suggestive of HCAs - the largest was 4.2 x 3.7 cm in segment VI, which subsequently underwent biopsy and microwave ablation. Histopathologic analysis revealed a well-differentiated hepatocellular neoplasm with unpaired arterioles, mild cytologic atypia, patchy hepatocyte crowding, and focal sinusoidal dilatation. Immunohistochemistry demonstrated negative membranous β-catenin staining and pericentral glutamine synthetase staining, ruling out β-catenin–activated HCA and focal nodular hyperplasia. Serum amyloid A and C-reactive protein were negative, inconsistent with inflammatory HCA. Liver fatty acid-binding protein (LFABP) staining was retained, excluding HNF-1α-inactivated HCA and HCC. Although focal reticulin abnormalities were noted, the findings were most consistent with an unclassified HCA.
Following ablation, the patient’s symptoms improved. She has since repeated surveillance imaging every six months. Her most recent MRI showed stable adenomas without evidence of new lesions.
Discussion: This case is notable for a young female with class III obesity and overlapping autoimmune conditions. Although obesity is a known risk factor for inflammatory HCA, immunohistochemistry did not support this subtype nor HNF1A-inactivated or β-catenin–activated, instead favoring an unclassified phenotype. This case highlights the need for molecular subtyping and individualized care in hepatic adenomatosis, particularly in patients with atypical or overlapping risk factors.
Figure: Figure 1. Coronal delayed-phase (20-minute) contrast-enhanced MRI of the liver demonstrating multiple hypointense hepatic lesions consistent with hepatocellular adenomas.
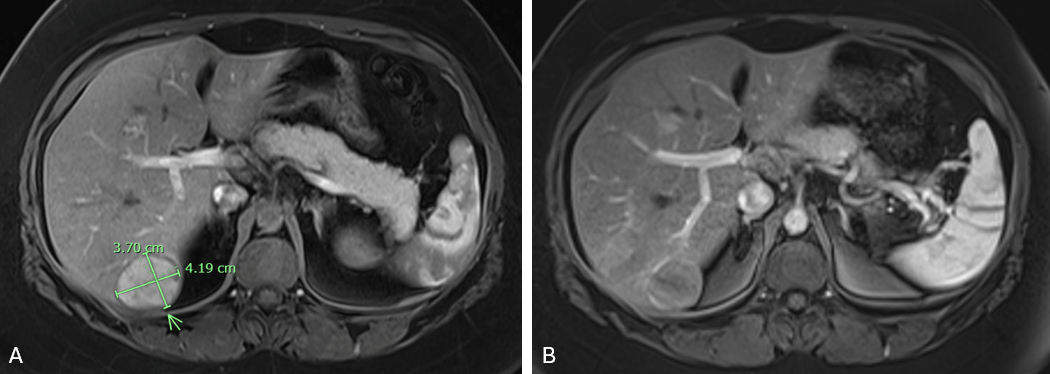
Figure: Figure 2. Axial arterial-phase contrast-enhanced MRI of the largest hepatic adenoma in segment VI, shown (A) prior to and (B) following microwave ablation.
Disclosures:
Franklin Liu indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Kai Tey indicated no relevant financial relationships.
Franklin Liu, MD1, Sabrina Ho, MD1, Samuel Cheong, DO1, Kai Tey, MBBS2. P6129 - Unclassified Hepatic Adenoma in the Setting of Hepatic Adenomatosis: A Case Report With Molecular Characterization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona Tucson, Tucson, AZ
Introduction: Hepatic adenomatosis was first described by Flejou et al in 1985 as the presence of ten or more hepatocellular adenomas (HCAs) in otherwise normal liver parenchyma. HCAs are benign epithelial liver tumors that can be subclassified into four major subtypes: hepatocyte nuclear factor-1α (HNF-1α) inactivated, β-catenin activated, inflammatory, and unclassified. Although typically benign, HCAs carry a risk of hemorrhage and malignant transformation into hepatocellular carcinoma (HCC), particularly in certain subtypes or when lesions are large or multifocal.
Case Description/
Methods: A 24-year-old female with a history of class III obesity, Ehlers-Danlos syndrome, systemic lupus erythematosus, eosinophilic esophagitis, asthma, irritable bowel syndrome, on oral contraception presented with chronic abdominal pain, diarrhea, and episodes of jaundice. Laboratory evaluation was unremarkable. MRI of the abdomen revealed 13 bilobar hepatic lesions suggestive of HCAs - the largest was 4.2 x 3.7 cm in segment VI, which subsequently underwent biopsy and microwave ablation. Histopathologic analysis revealed a well-differentiated hepatocellular neoplasm with unpaired arterioles, mild cytologic atypia, patchy hepatocyte crowding, and focal sinusoidal dilatation. Immunohistochemistry demonstrated negative membranous β-catenin staining and pericentral glutamine synthetase staining, ruling out β-catenin–activated HCA and focal nodular hyperplasia. Serum amyloid A and C-reactive protein were negative, inconsistent with inflammatory HCA. Liver fatty acid-binding protein (LFABP) staining was retained, excluding HNF-1α-inactivated HCA and HCC. Although focal reticulin abnormalities were noted, the findings were most consistent with an unclassified HCA.
Following ablation, the patient’s symptoms improved. She has since repeated surveillance imaging every six months. Her most recent MRI showed stable adenomas without evidence of new lesions.
Discussion: This case is notable for a young female with class III obesity and overlapping autoimmune conditions. Although obesity is a known risk factor for inflammatory HCA, immunohistochemistry did not support this subtype nor HNF1A-inactivated or β-catenin–activated, instead favoring an unclassified phenotype. This case highlights the need for molecular subtyping and individualized care in hepatic adenomatosis, particularly in patients with atypical or overlapping risk factors.
Figure: Figure 1. Coronal delayed-phase (20-minute) contrast-enhanced MRI of the liver demonstrating multiple hypointense hepatic lesions consistent with hepatocellular adenomas.
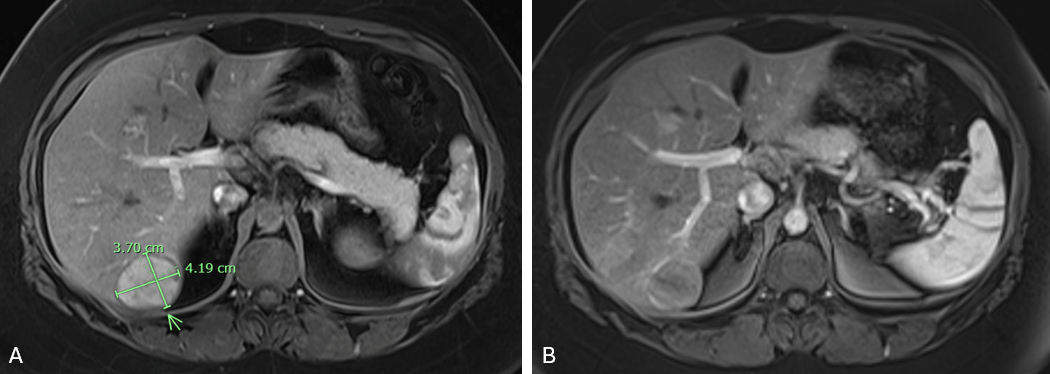
Figure: Figure 2. Axial arterial-phase contrast-enhanced MRI of the largest hepatic adenoma in segment VI, shown (A) prior to and (B) following microwave ablation.
Disclosures:
Franklin Liu indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Kai Tey indicated no relevant financial relationships.
Franklin Liu, MD1, Sabrina Ho, MD1, Samuel Cheong, DO1, Kai Tey, MBBS2. P6129 - Unclassified Hepatic Adenoma in the Setting of Hepatic Adenomatosis: A Case Report With Molecular Characterization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
