Tuesday Poster Session
Category: Liver
P6075 - Multisystem Amyloidosis Mimicking Cirrhosis and Hepatorenal Syndrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NK
Nadia Kohler
Creighton University School of Medicine
Phoenix, Arizona
Presenting Author(s)
Nadia Kohler, Vishnu Yanamaladoddi, MD, Alonso C. Gonzalez, MD, Brianna A. Werner, , Vikash Kumar, MD, Justin Reynolds, MD
Creighton University School of Medicine, Phoenix, AZ
Introduction: Hepatic involvement in systemic amyloidosis is rare but can closely resemble advanced liver disease. Nonspecific presentations often lead to diagnostic delays, particularly in patients with coexisting plasma cell dyscrasias. We present a case of hepatic amyloidosis initially misdiagnosed as cirrhosis with hepatorenal syndrome (HRS).
Case Description/
Methods: A 78-year-old female with atrial fibrillation and smoldering IgG lambda myeloma (diagnosed 3 months prior - 13% plasma cells, negative bone marrow Congo red) presented with progressive abdominal distention, 40-lb unintentional weight loss, jaundice, dyspnea, and edema. Exam revealed icterus, digital clubbing, anasarca and hepatosplenomegaly. Labs showed hyponatremia, metabolic acidosis, renal dysfunction, cholestatic liver injury (total bilirubin 9.9 mg/dL, ALP 1311 U/L), and elevated BNP (3774 pg/mL).
RUQ Doppler showed cirrhotic morphology without portal vein thrombosis. CT abdomen showed hepatomegaly, ascites, gallbladder wall and mesenteric edema, and volume overload. HIDA scan was negative. MRCP showed no obstruction but revealed diffuse hepatic parenchymal signal loss, suggesting infiltrative disease as cause of liver injury. Echocardiography revealed LVEF 45–50% with grade III diastolic dysfunction; cardiac MRI showed late gadolinium enhancement consistent with infiltrative cardiomyopathy.
Given her myeloma and multiorgan involvement, systemic amyloidosis was suspected. Despite initial negative bone marrow Congo red staining, fat pad biopsy confirmed AL amyloidosis. Her condition deteriorated with refractory hypotension and multiorgan failure. Patient transitioned to comfort care.
Discussion: This case highlights the diagnostic challenge of hepatic amyloidosis, which can mimic cirrhosis and HRS. Initial tests, including bone marrow biopsy, may be falsely negative due to the sequential pattern of amyloid deposition, often beginning in soft tissues like fat pad before involving deeper organs. Multi-organ dysfunction, particularly with restrictive cardiomyopathy and cholestatic liver injury in the absence of classic cirrhosis risk factors, should prompt consideration of infiltrative diseases. MRCP and cardiac MRI can provide valuable diagnostic clues, while fat pad biopsy remains a minimally invasive and highly specific tool for diagnosis. Early recognition is crucial, as systemic amyloidosis can progress rapidly, limiting treatment options and worsening prognosis.

Figure: CT abdomen showing hepatomegaly with mild ascites
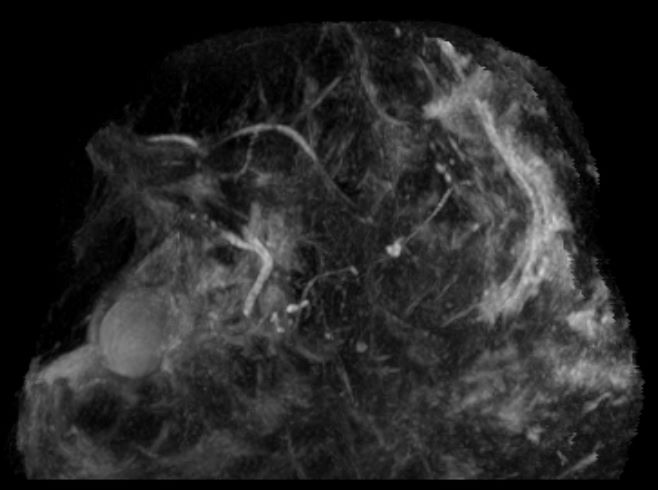
Figure: MRCP showing no gallbladder wall edema and pericholecystic fluid, no intra or extra hepatic biliary duct dilatation and no filling defects
Disclosures:
Nadia Kohler indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Alonso Gonzalez indicated no relevant financial relationships.
Brianna Werner indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Nadia Kohler, Vishnu Yanamaladoddi, MD, Alonso C. Gonzalez, MD, Brianna A. Werner, , Vikash Kumar, MD, Justin Reynolds, MD. P6075 - Multisystem Amyloidosis Mimicking Cirrhosis and Hepatorenal Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Creighton University School of Medicine, Phoenix, AZ
Introduction: Hepatic involvement in systemic amyloidosis is rare but can closely resemble advanced liver disease. Nonspecific presentations often lead to diagnostic delays, particularly in patients with coexisting plasma cell dyscrasias. We present a case of hepatic amyloidosis initially misdiagnosed as cirrhosis with hepatorenal syndrome (HRS).
Case Description/
Methods: A 78-year-old female with atrial fibrillation and smoldering IgG lambda myeloma (diagnosed 3 months prior - 13% plasma cells, negative bone marrow Congo red) presented with progressive abdominal distention, 40-lb unintentional weight loss, jaundice, dyspnea, and edema. Exam revealed icterus, digital clubbing, anasarca and hepatosplenomegaly. Labs showed hyponatremia, metabolic acidosis, renal dysfunction, cholestatic liver injury (total bilirubin 9.9 mg/dL, ALP 1311 U/L), and elevated BNP (3774 pg/mL).
RUQ Doppler showed cirrhotic morphology without portal vein thrombosis. CT abdomen showed hepatomegaly, ascites, gallbladder wall and mesenteric edema, and volume overload. HIDA scan was negative. MRCP showed no obstruction but revealed diffuse hepatic parenchymal signal loss, suggesting infiltrative disease as cause of liver injury. Echocardiography revealed LVEF 45–50% with grade III diastolic dysfunction; cardiac MRI showed late gadolinium enhancement consistent with infiltrative cardiomyopathy.
Given her myeloma and multiorgan involvement, systemic amyloidosis was suspected. Despite initial negative bone marrow Congo red staining, fat pad biopsy confirmed AL amyloidosis. Her condition deteriorated with refractory hypotension and multiorgan failure. Patient transitioned to comfort care.
Discussion: This case highlights the diagnostic challenge of hepatic amyloidosis, which can mimic cirrhosis and HRS. Initial tests, including bone marrow biopsy, may be falsely negative due to the sequential pattern of amyloid deposition, often beginning in soft tissues like fat pad before involving deeper organs. Multi-organ dysfunction, particularly with restrictive cardiomyopathy and cholestatic liver injury in the absence of classic cirrhosis risk factors, should prompt consideration of infiltrative diseases. MRCP and cardiac MRI can provide valuable diagnostic clues, while fat pad biopsy remains a minimally invasive and highly specific tool for diagnosis. Early recognition is crucial, as systemic amyloidosis can progress rapidly, limiting treatment options and worsening prognosis.

Figure: CT abdomen showing hepatomegaly with mild ascites
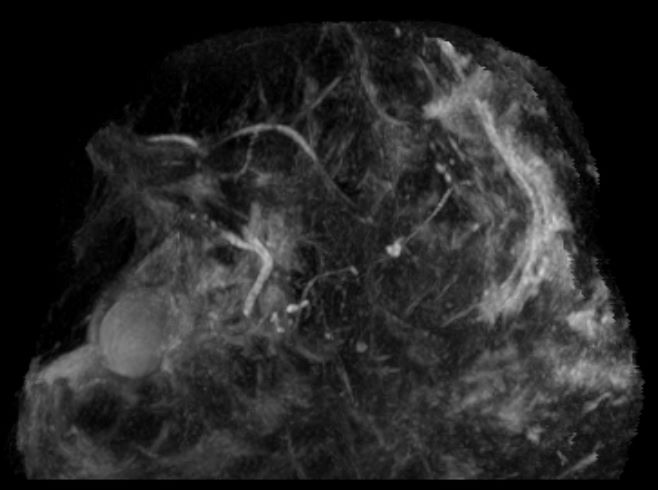
Figure: MRCP showing no gallbladder wall edema and pericholecystic fluid, no intra or extra hepatic biliary duct dilatation and no filling defects
Disclosures:
Nadia Kohler indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Alonso Gonzalez indicated no relevant financial relationships.
Brianna Werner indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Nadia Kohler, Vishnu Yanamaladoddi, MD, Alonso C. Gonzalez, MD, Brianna A. Werner, , Vikash Kumar, MD, Justin Reynolds, MD. P6075 - Multisystem Amyloidosis Mimicking Cirrhosis and Hepatorenal Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
