Tuesday Poster Session
Category: Liver
P6073 - A Portal Closed, a Window Opened: Salvage DIPS in Budd-Chiari From Ulcerative Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Yanamaladoddi, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Award: ACG Presidential Poster Award
Edy Hatem, MD1, Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Amla Patel, MBBS2, Justin Reynolds, MD1, Nilofar Najafian, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University, Phoenix, Phoenix, AZ
Introduction: Portal vein thrombosis (PVT) is a rare complication of inflammatory bowel disease (IBD), often associated with active inflammation, corticosteroid use, and hypercoagulability. While transjugular intrahepatic portosystemic shunt (TIPS) is standard for portal hypertension, extensive thrombosis or cavernous transformation may render the procedure technically challenging. In such scenarios, direct intrahepatic portosystemic shunt (DIPS) offers a complex but viable alternative. We present a rare case of a young woman with ulcerative colitis (UC) and extensive splanchnic thrombosis successfully treated with DIPS.
Case Description/
Methods: A 36-year-old female with a 4-year history of poorly controlled UC and prior PVT presented with one week of bloody diarrhea, fatigue, and lethargy. She had failed multiple therapies due to intolerance and developed anti-infliximab antibodies, requiring chronic corticosteroids. Labs revealed ALT 320 U/L, AST 138 U/L, ALP 243 U/L, bilirubin 1.9 mg/dL, INR 2.6. She developed progressive encephalopathy from acute liver failure. Imaging revealed extensive thrombosis involving superior mesenteric, splenic, portal vein with cavernous transformation, and hepatic veins consistent with Budd-Chiari syndrome. Additional findings included splenomegaly with infarcts, and peripancreatic edema. EGD showed small esophageal and extensive gastric varices with portal hypertensive gastropathy. Liver biopsy demonstrated sinusoidal congestion, central and portal vein dilation, nodular regenerative hyperplasia, and macrovesicular steatosis without fibrosis. She was started on IV steroids and anticoagulation. The extent of thrombosis precluded TIPS and liver transplant due to anatomical inaccessibility. As a last resort, DIPS was successfully performed using a visualized target. At 6-week follow-up, she demonstrated marked clinical and biochemical improvement, including complete resolution of encephalopathy.
Discussion: This case illustrates extensive splanchnic and IVC thrombosis as a rare but serious complication of UC, leading to portal hypertension and encephalopathy. TIPS was unfeasible due to cavernous transformation, and liver transplant was not possible due to the thrombotic burden. DIPS was successfully performed with marked clinical improvement. This highlights DIPS as a vital alternative in complex thrombotic IBD cases and the need for early, multidisciplinary management.
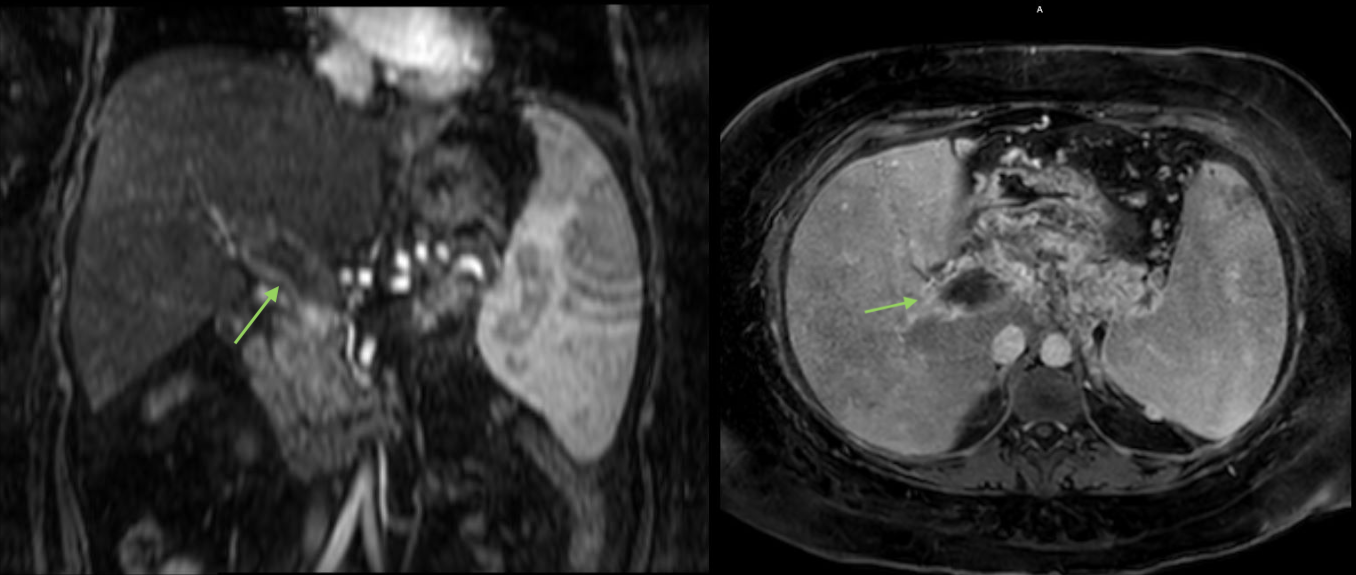
Figure: Coronal and axial CT showing portal vein thrombosis
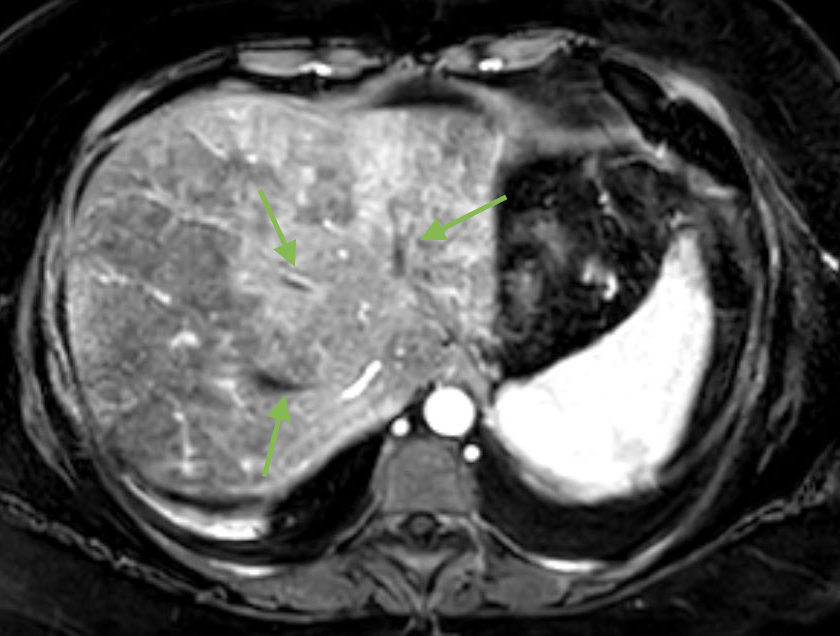
Figure: CT showing thrombosis of all three hepatic veins
Disclosures:
Edy Hatem indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Edy Hatem, MD1, Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Amla Patel, MBBS2, Justin Reynolds, MD1, Nilofar Najafian, MD1. P6073 - A Portal Closed, a Window Opened: Salvage DIPS in Budd-Chiari From Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Edy Hatem, MD1, Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Amla Patel, MBBS2, Justin Reynolds, MD1, Nilofar Najafian, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University, Phoenix, Phoenix, AZ
Introduction: Portal vein thrombosis (PVT) is a rare complication of inflammatory bowel disease (IBD), often associated with active inflammation, corticosteroid use, and hypercoagulability. While transjugular intrahepatic portosystemic shunt (TIPS) is standard for portal hypertension, extensive thrombosis or cavernous transformation may render the procedure technically challenging. In such scenarios, direct intrahepatic portosystemic shunt (DIPS) offers a complex but viable alternative. We present a rare case of a young woman with ulcerative colitis (UC) and extensive splanchnic thrombosis successfully treated with DIPS.
Case Description/
Methods: A 36-year-old female with a 4-year history of poorly controlled UC and prior PVT presented with one week of bloody diarrhea, fatigue, and lethargy. She had failed multiple therapies due to intolerance and developed anti-infliximab antibodies, requiring chronic corticosteroids. Labs revealed ALT 320 U/L, AST 138 U/L, ALP 243 U/L, bilirubin 1.9 mg/dL, INR 2.6. She developed progressive encephalopathy from acute liver failure. Imaging revealed extensive thrombosis involving superior mesenteric, splenic, portal vein with cavernous transformation, and hepatic veins consistent with Budd-Chiari syndrome. Additional findings included splenomegaly with infarcts, and peripancreatic edema. EGD showed small esophageal and extensive gastric varices with portal hypertensive gastropathy. Liver biopsy demonstrated sinusoidal congestion, central and portal vein dilation, nodular regenerative hyperplasia, and macrovesicular steatosis without fibrosis. She was started on IV steroids and anticoagulation. The extent of thrombosis precluded TIPS and liver transplant due to anatomical inaccessibility. As a last resort, DIPS was successfully performed using a visualized target. At 6-week follow-up, she demonstrated marked clinical and biochemical improvement, including complete resolution of encephalopathy.
Discussion: This case illustrates extensive splanchnic and IVC thrombosis as a rare but serious complication of UC, leading to portal hypertension and encephalopathy. TIPS was unfeasible due to cavernous transformation, and liver transplant was not possible due to the thrombotic burden. DIPS was successfully performed with marked clinical improvement. This highlights DIPS as a vital alternative in complex thrombotic IBD cases and the need for early, multidisciplinary management.
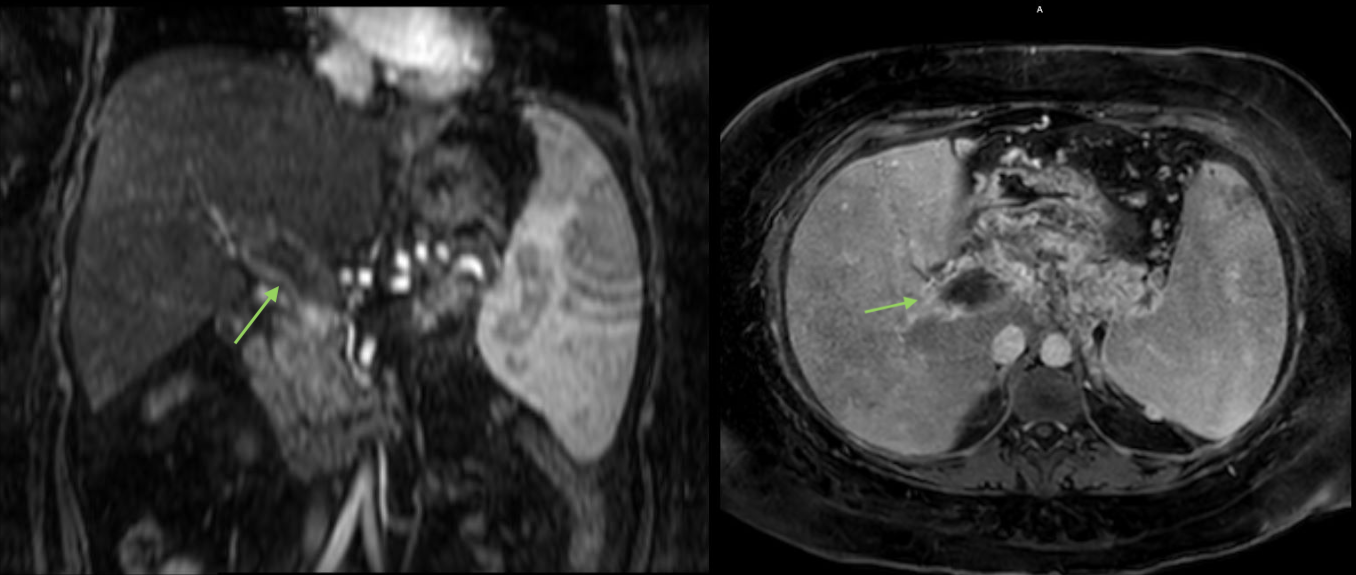
Figure: Coronal and axial CT showing portal vein thrombosis
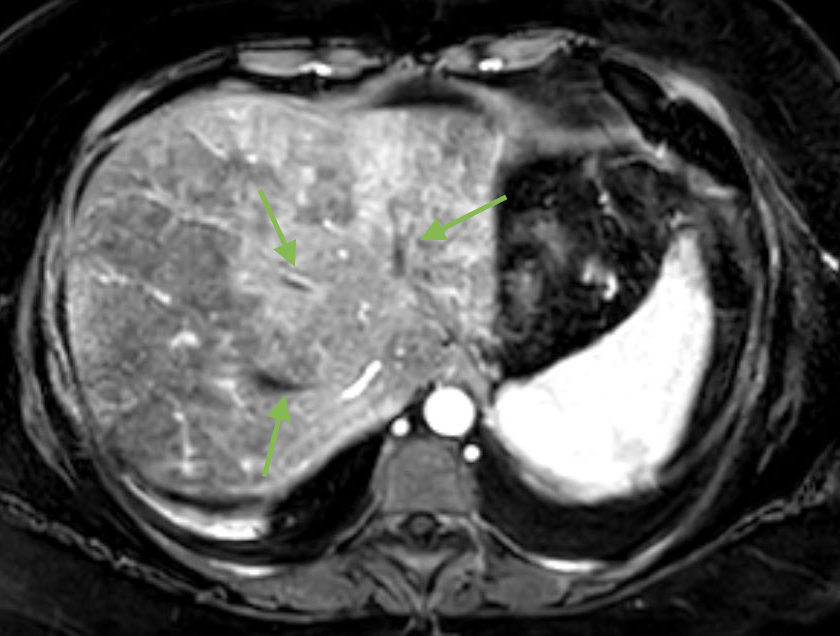
Figure: CT showing thrombosis of all three hepatic veins
Disclosures:
Edy Hatem indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Edy Hatem, MD1, Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Amla Patel, MBBS2, Justin Reynolds, MD1, Nilofar Najafian, MD1. P6073 - A Portal Closed, a Window Opened: Salvage DIPS in Budd-Chiari From Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

