Tuesday Poster Session
Category: Liver
P6024 - A Rare Complication of Hepatic Cysts in Advanced Autosomal Dominant Polycystic Kidney and Liver Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Sneh Sonaiya, MD, MPH, MBA, Jiayi Ge, MD, Jonathan hansen, DO, Pei Xue, MD, Vignan Manne, MD
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Autosomal dominant polycystic kidney disease (ADPKD) is among the most common hereditary kidney disorders, with an estimated prevalence of 1 in 400 to 1,000 individuals. Autosomal dominant polycystic liver disease (ADPLD), frequently associated with ADPKD, is considerably rarer, affecting fewer than 1 in 10,000 people [1]. While most hepatic cysts are asymptomatic, infected liver cysts represent an uncommon but potentially serious complication of ADPKD/PLD.
Case Description/
Methods: A 55-year-old female with known ADPKD/PLD presented with generalized abdominal pain, distension, and non-bloody diarrhea. She was septic on arrival, with labs notable for AKI on CKD (BUN 67, Cr 5.69, GFR 8), lactate 2.3, Na 125, and CRP >200. CT imaging showed extensive polycystic changes in both kidneys and liver, consistent with Gigot type III PLD [Figure 1]. Blood cultures grew Klebsiella spp. and Pantoea spp. Patient was empirically started on intravenous meropenem and later de-escalated to ampicillin-sulbactam. IR-guided percutaneous drainage of the infected liver cyst was performed with 1000 mL serous fluid output; fluid culture grew Klebsiella spp., confirming cyst infection as the likely source of sepsis. Given the AKI on CKD, she required hemodialysis during the hospitalization. The patient improved clinically and was discharged on oral amoxicillin-clavulanate, with plans for outpatient dialysis, and outpatient kidney and liver transplant evaluation.
Discussion: This case highlights a rare, but serious complication of ADPKD/PLD: hepatic cyst infection leading to sepsis and AKI on CKD. Infected liver cysts occur in fewer than 10% of patients with PLD and are notably less common than superinfected renal cysts [2]. CT imaging, especially without contrast due to AKI, can be of limited utility in localization of infection, whereas 18F-FDG PET can help localize metabolically active cysts. Management of hepatic cyst infection involves broad-spectrum antibiotics tailored to cultures; however, up to 64% of cases may require additional interventions such as percutaneous drainage or surgical management [3]. Treatment options for PLD include aspiration sclerotherapy, surgical fenestration of cysts, partial hepatic resection, or, in severe cases, orthotopic liver transplantation [4]. However, in patients with advanced ADPKD/PLD, including Gigot type III PLD and progressive renal failure, curative options become limited, and combined liver and kidney transplantation is the only definitive therapeutic option.
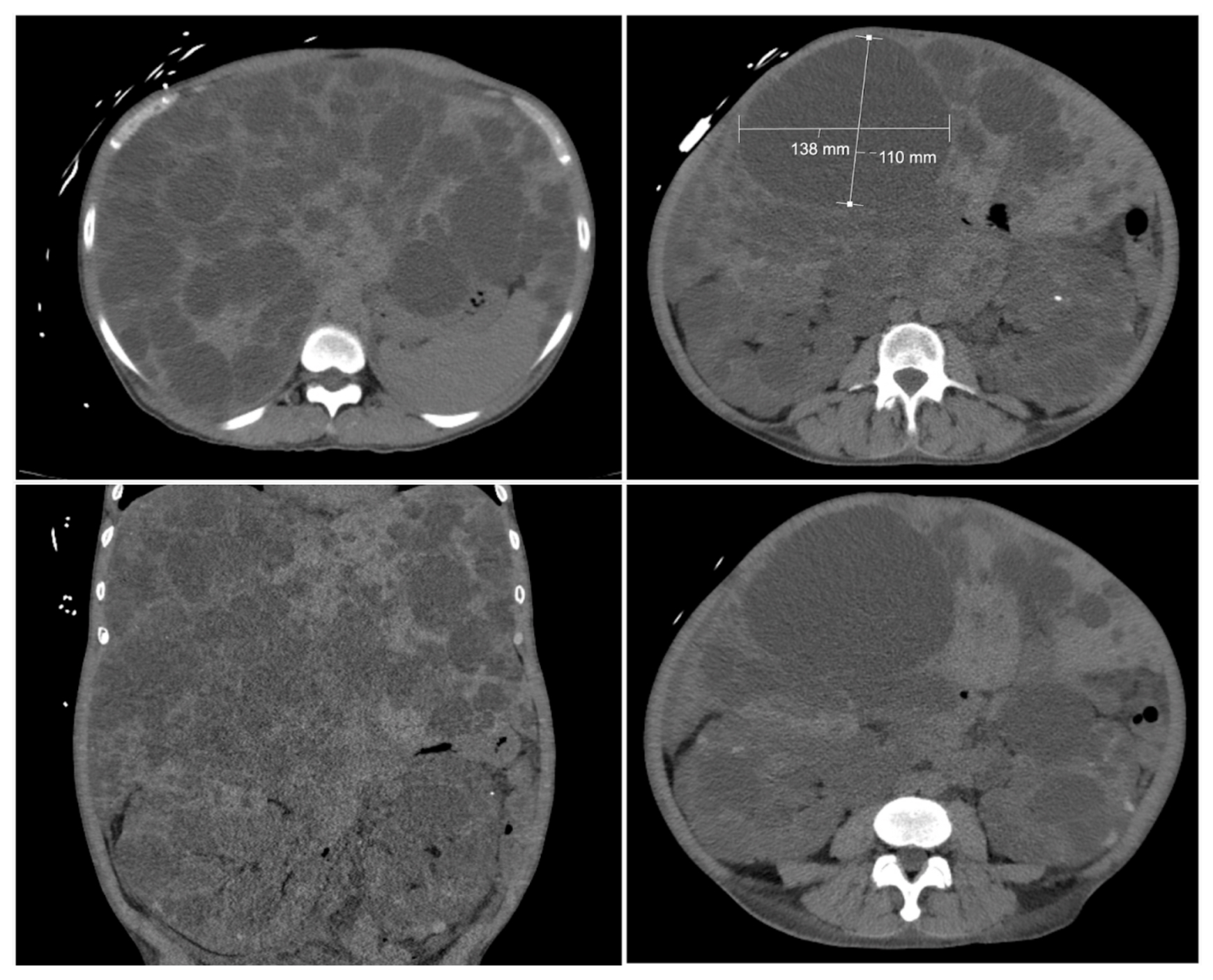
Figure: Figure 1: Non-contrast CT Imaging of the Abdomen Showing Extensive Polycystic Changes in Both Kidneys and Liver, Consistent with Advanced Autosomal Dominant Polycystic Kidney and Liver Disease. Liver cyst with measurement (13.8 cm x 11 cm) indicates the hepatic cyst that was drained percutaneously, with 1000 mL serous drainage output.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Jiayi Ge indicated no relevant financial relationships.
Jonathan hansen indicated no relevant financial relationships.
Pei Xue indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA, Jiayi Ge, MD, Jonathan hansen, DO, Pei Xue, MD, Vignan Manne, MD. P6024 - A Rare Complication of Hepatic Cysts in Advanced Autosomal Dominant Polycystic Kidney and Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Autosomal dominant polycystic kidney disease (ADPKD) is among the most common hereditary kidney disorders, with an estimated prevalence of 1 in 400 to 1,000 individuals. Autosomal dominant polycystic liver disease (ADPLD), frequently associated with ADPKD, is considerably rarer, affecting fewer than 1 in 10,000 people [1]. While most hepatic cysts are asymptomatic, infected liver cysts represent an uncommon but potentially serious complication of ADPKD/PLD.
Case Description/
Methods: A 55-year-old female with known ADPKD/PLD presented with generalized abdominal pain, distension, and non-bloody diarrhea. She was septic on arrival, with labs notable for AKI on CKD (BUN 67, Cr 5.69, GFR 8), lactate 2.3, Na 125, and CRP >200. CT imaging showed extensive polycystic changes in both kidneys and liver, consistent with Gigot type III PLD [Figure 1]. Blood cultures grew Klebsiella spp. and Pantoea spp. Patient was empirically started on intravenous meropenem and later de-escalated to ampicillin-sulbactam. IR-guided percutaneous drainage of the infected liver cyst was performed with 1000 mL serous fluid output; fluid culture grew Klebsiella spp., confirming cyst infection as the likely source of sepsis. Given the AKI on CKD, she required hemodialysis during the hospitalization. The patient improved clinically and was discharged on oral amoxicillin-clavulanate, with plans for outpatient dialysis, and outpatient kidney and liver transplant evaluation.
Discussion: This case highlights a rare, but serious complication of ADPKD/PLD: hepatic cyst infection leading to sepsis and AKI on CKD. Infected liver cysts occur in fewer than 10% of patients with PLD and are notably less common than superinfected renal cysts [2]. CT imaging, especially without contrast due to AKI, can be of limited utility in localization of infection, whereas 18F-FDG PET can help localize metabolically active cysts. Management of hepatic cyst infection involves broad-spectrum antibiotics tailored to cultures; however, up to 64% of cases may require additional interventions such as percutaneous drainage or surgical management [3]. Treatment options for PLD include aspiration sclerotherapy, surgical fenestration of cysts, partial hepatic resection, or, in severe cases, orthotopic liver transplantation [4]. However, in patients with advanced ADPKD/PLD, including Gigot type III PLD and progressive renal failure, curative options become limited, and combined liver and kidney transplantation is the only definitive therapeutic option.
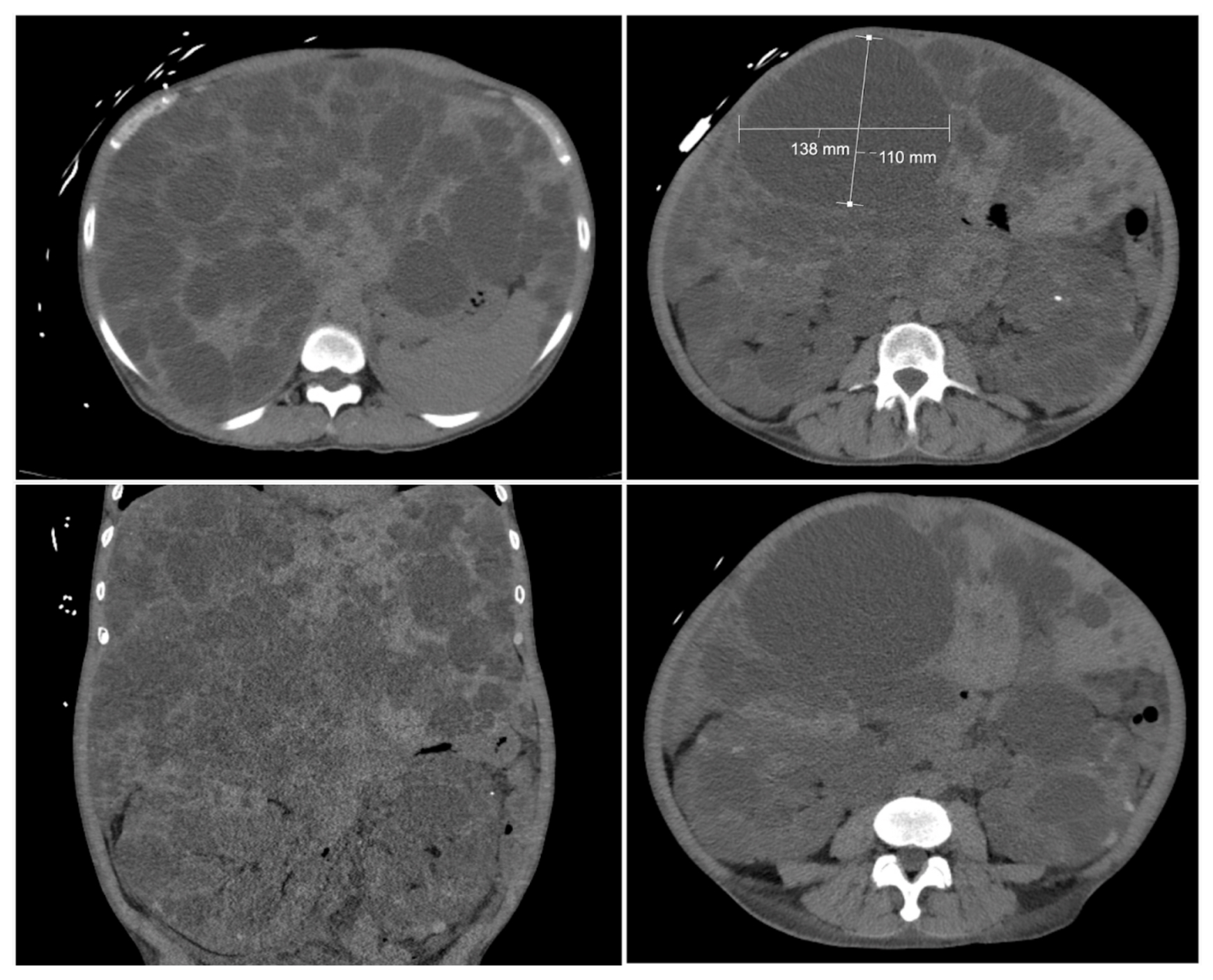
Figure: Figure 1: Non-contrast CT Imaging of the Abdomen Showing Extensive Polycystic Changes in Both Kidneys and Liver, Consistent with Advanced Autosomal Dominant Polycystic Kidney and Liver Disease. Liver cyst with measurement (13.8 cm x 11 cm) indicates the hepatic cyst that was drained percutaneously, with 1000 mL serous drainage output.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Jiayi Ge indicated no relevant financial relationships.
Jonathan hansen indicated no relevant financial relationships.
Pei Xue indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA, Jiayi Ge, MD, Jonathan hansen, DO, Pei Xue, MD, Vignan Manne, MD. P6024 - A Rare Complication of Hepatic Cysts in Advanced Autosomal Dominant Polycystic Kidney and Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

