Tuesday Poster Session
Category: Liver
P6005 - Painless Obstructive Jaundice Suspected of Malignancy: A Case of IgG4-Related Hepatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abraham Nakshabendi, BS
St. James School of Medicine
Tampa, FL
Presenting Author(s)
Abraham Nakshabendi, BS1, Jennie An, BS2, Ramy R. Mitwalli, MD, MBA, MSc3, Rahman Nakshabendi, MD3
1St. James School of Medicine, Tampa, FL; 2St. James School of Medicine, Chicago, IL; 3Florida Advanced Gastroenterology Center, Tampa, FL
Introduction: IgG4-related disease is a systemic inflammatory condition characterized by infiltration of various organs, including the liver, by IgG4-positive plasma cells. IgG4-related hepatitis is rare and often mimics primary sclerosing cholangitis and autoimmune hepatitis, complicating diagnosis. It is more common in males than females (2.2:1). Early recognition is essential to prevent liver damage, as the disease typically responds well to corticosteroids. A full diagnostic workup is important to rule out malignancy.
Case Description/
Methods: A 70-year-old female with a family history of pancreatic cancer presented with fatigue, weight loss, jaundice, elevated liver enzymes (AST 97 U/L, ALT 62 U/L, ALP 954 U/L), and total bilirubin of 10 mg/dl. Viral and autoimmune markers, including ANA and SMA, were unremarkable. CT scan and MRI demonstrated a 6 cm hepatic mass with lymphadenopathy prompting further evaluation with EUS and ERCP
EUS revealed normal hepatic parenchyma with dilated intrahepatic duct. FNB EUS obtained at the transition site from biliary stenosis to intrahepatic biliary dilation.
ERCP with cholangioscopy revealed biliary stenosis at the common hepatic duct, two intrahepatic biliary stents placed for decompression.
Liver biopsy demonstrated portal and periportal lymphoplasmacytic infiltrates with fibrosis and more than 50 IgG4-positive plasma cells per high-power field, confirming IgG4-related hepatitis. She was started on 40 mg prednisone with plans for repeat Imaging within 3 months time with follow up ERCP stent removal.
Discussion: We present a case of IgG4-related disease mimicking malignant obstructive jaundice. The diagnostic approach and follow-up are essential to confirm the diagnosis. Liver biopsy typically reveals a dense lymphoplasmacytic infiltrate with numerous IgG4-positive plasma cells, storiform fibrosis, and obliterative phlebitis. It is important to distinguish this from autoimmune hepatitis, as treatments differ. Corticosteroids remain the mainstay of therapy and generally yield good clinical response, though relapses may occur. Early diagnosis and treatment are critical to avoid cirrhosis or liver failure. In biliary involvement, ERCP may be necessary for decompression. Ongoing research is needed to refine diagnostic criteria and optimize long-term care. Follow-up imaging after treatment helps confirm lesion resolution and rule out neoplasia.
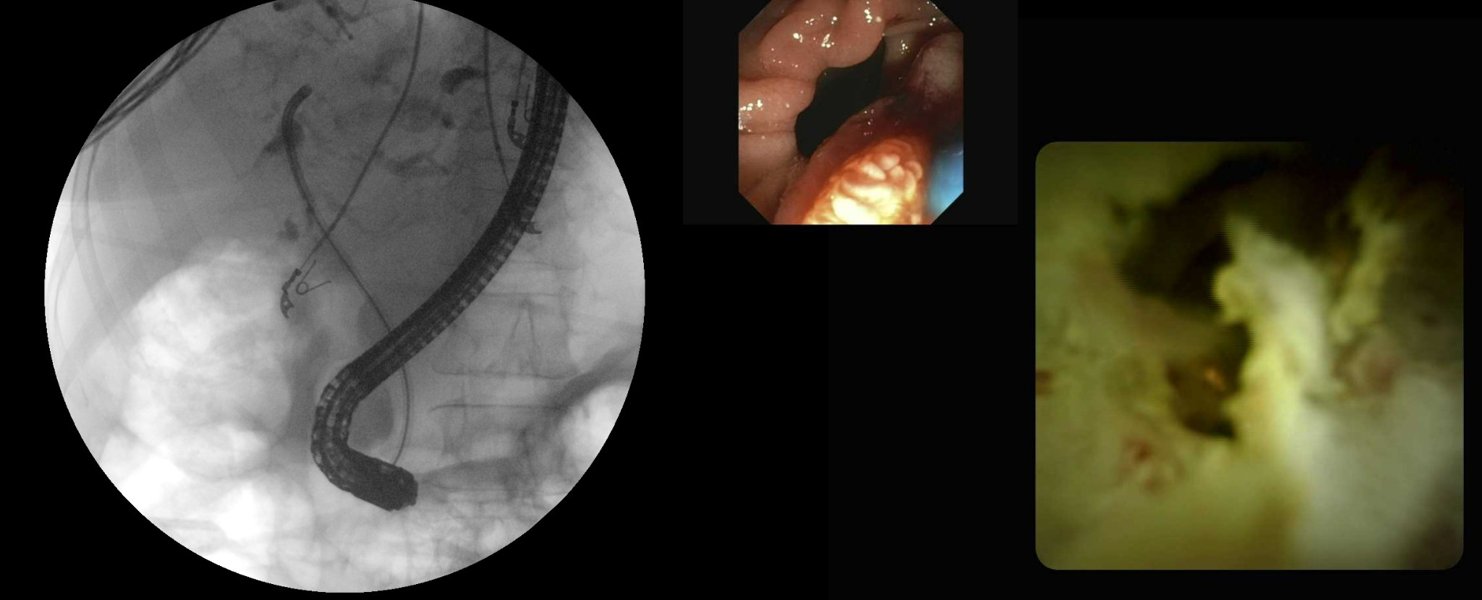
Figure: Left: Coronal CT of the chest and upper abdomen demonstrating a 6 cm left hepatic mass.
Top Right: Dilated intrahepatic ducts on EUS
Bottom Right: Lymph node biopsy on EUS
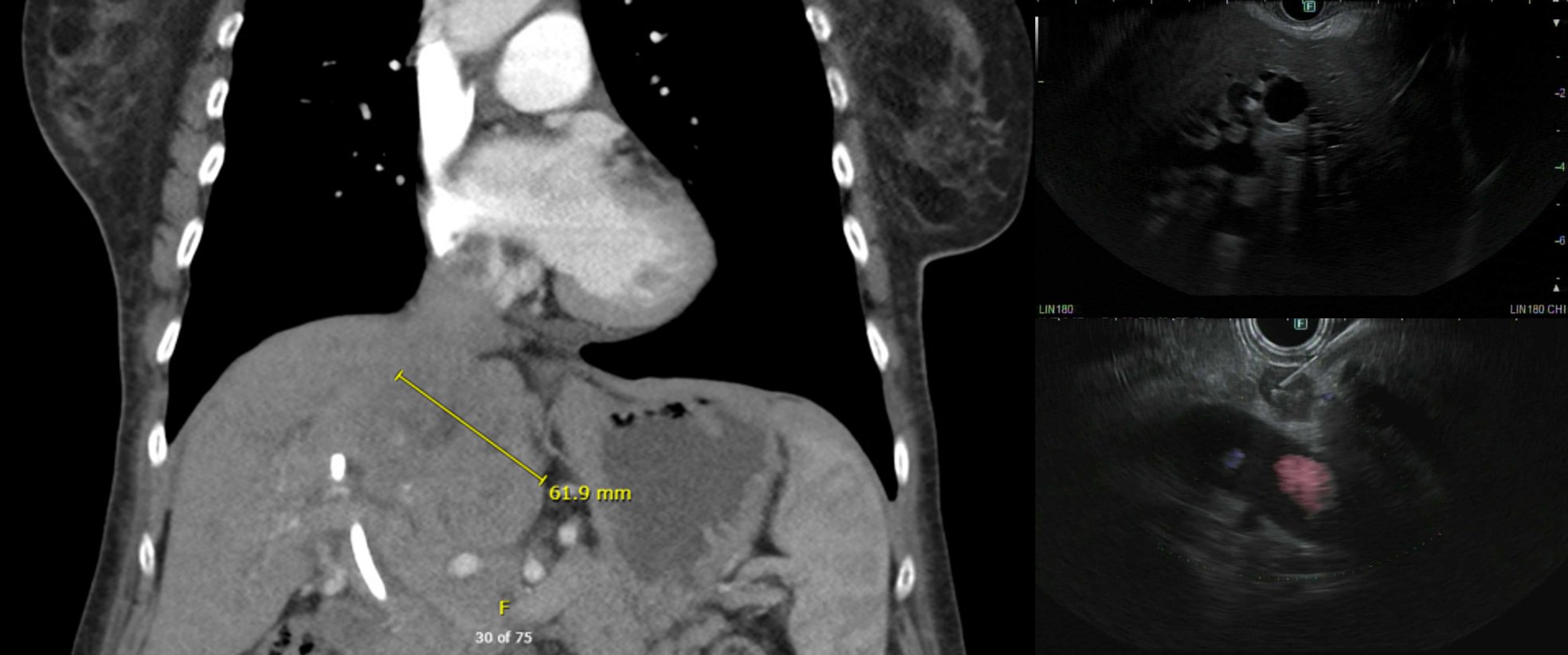
Figure: Left: Fluoroscopy demonstrating cholangioscope in the left common hepatic duct.
Middle and right: ERCP Cholangioscopy
Disclosures:
Abraham Nakshabendi indicated no relevant financial relationships.
Jennie An indicated no relevant financial relationships.
Ramy Mitwalli indicated no relevant financial relationships.
Rahman Nakshabendi indicated no relevant financial relationships.
Abraham Nakshabendi, BS1, Jennie An, BS2, Ramy R. Mitwalli, MD, MBA, MSc3, Rahman Nakshabendi, MD3. P6005 - Painless Obstructive Jaundice Suspected of Malignancy: A Case of IgG4-Related Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. James School of Medicine, Tampa, FL; 2St. James School of Medicine, Chicago, IL; 3Florida Advanced Gastroenterology Center, Tampa, FL
Introduction: IgG4-related disease is a systemic inflammatory condition characterized by infiltration of various organs, including the liver, by IgG4-positive plasma cells. IgG4-related hepatitis is rare and often mimics primary sclerosing cholangitis and autoimmune hepatitis, complicating diagnosis. It is more common in males than females (2.2:1). Early recognition is essential to prevent liver damage, as the disease typically responds well to corticosteroids. A full diagnostic workup is important to rule out malignancy.
Case Description/
Methods: A 70-year-old female with a family history of pancreatic cancer presented with fatigue, weight loss, jaundice, elevated liver enzymes (AST 97 U/L, ALT 62 U/L, ALP 954 U/L), and total bilirubin of 10 mg/dl. Viral and autoimmune markers, including ANA and SMA, were unremarkable. CT scan and MRI demonstrated a 6 cm hepatic mass with lymphadenopathy prompting further evaluation with EUS and ERCP
EUS revealed normal hepatic parenchyma with dilated intrahepatic duct. FNB EUS obtained at the transition site from biliary stenosis to intrahepatic biliary dilation.
ERCP with cholangioscopy revealed biliary stenosis at the common hepatic duct, two intrahepatic biliary stents placed for decompression.
Liver biopsy demonstrated portal and periportal lymphoplasmacytic infiltrates with fibrosis and more than 50 IgG4-positive plasma cells per high-power field, confirming IgG4-related hepatitis. She was started on 40 mg prednisone with plans for repeat Imaging within 3 months time with follow up ERCP stent removal.
Discussion: We present a case of IgG4-related disease mimicking malignant obstructive jaundice. The diagnostic approach and follow-up are essential to confirm the diagnosis. Liver biopsy typically reveals a dense lymphoplasmacytic infiltrate with numerous IgG4-positive plasma cells, storiform fibrosis, and obliterative phlebitis. It is important to distinguish this from autoimmune hepatitis, as treatments differ. Corticosteroids remain the mainstay of therapy and generally yield good clinical response, though relapses may occur. Early diagnosis and treatment are critical to avoid cirrhosis or liver failure. In biliary involvement, ERCP may be necessary for decompression. Ongoing research is needed to refine diagnostic criteria and optimize long-term care. Follow-up imaging after treatment helps confirm lesion resolution and rule out neoplasia.
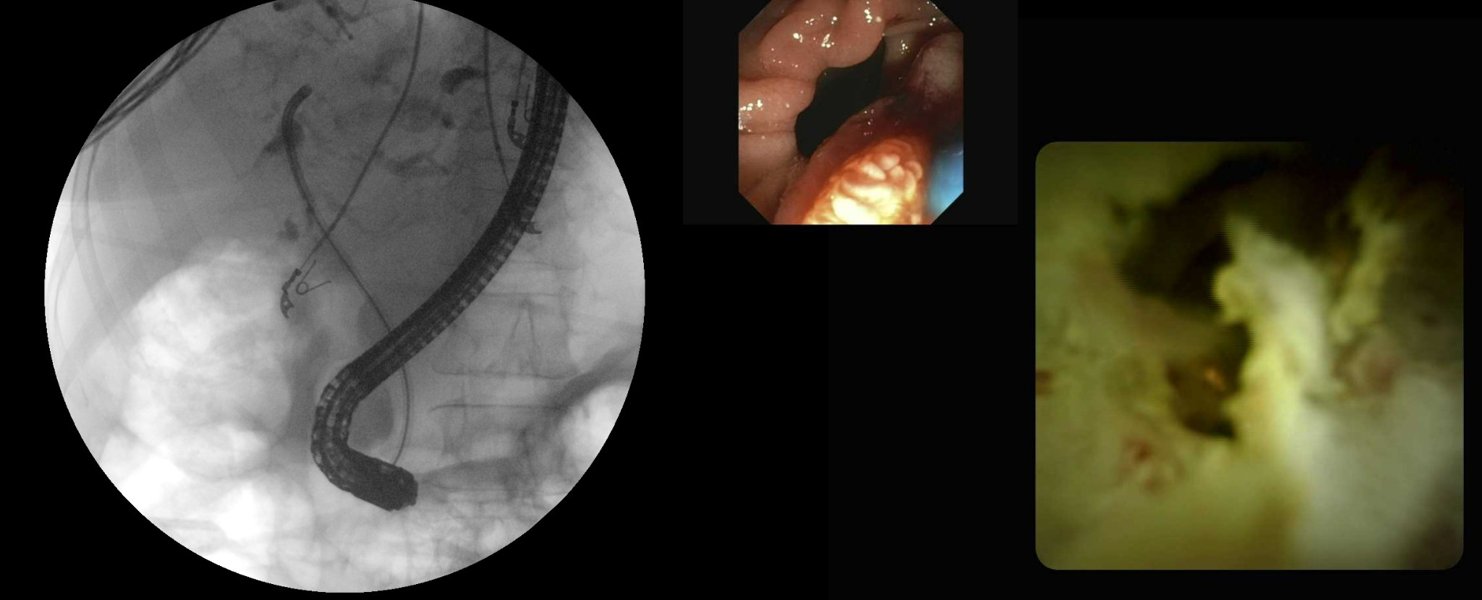
Figure: Left: Coronal CT of the chest and upper abdomen demonstrating a 6 cm left hepatic mass.
Top Right: Dilated intrahepatic ducts on EUS
Bottom Right: Lymph node biopsy on EUS
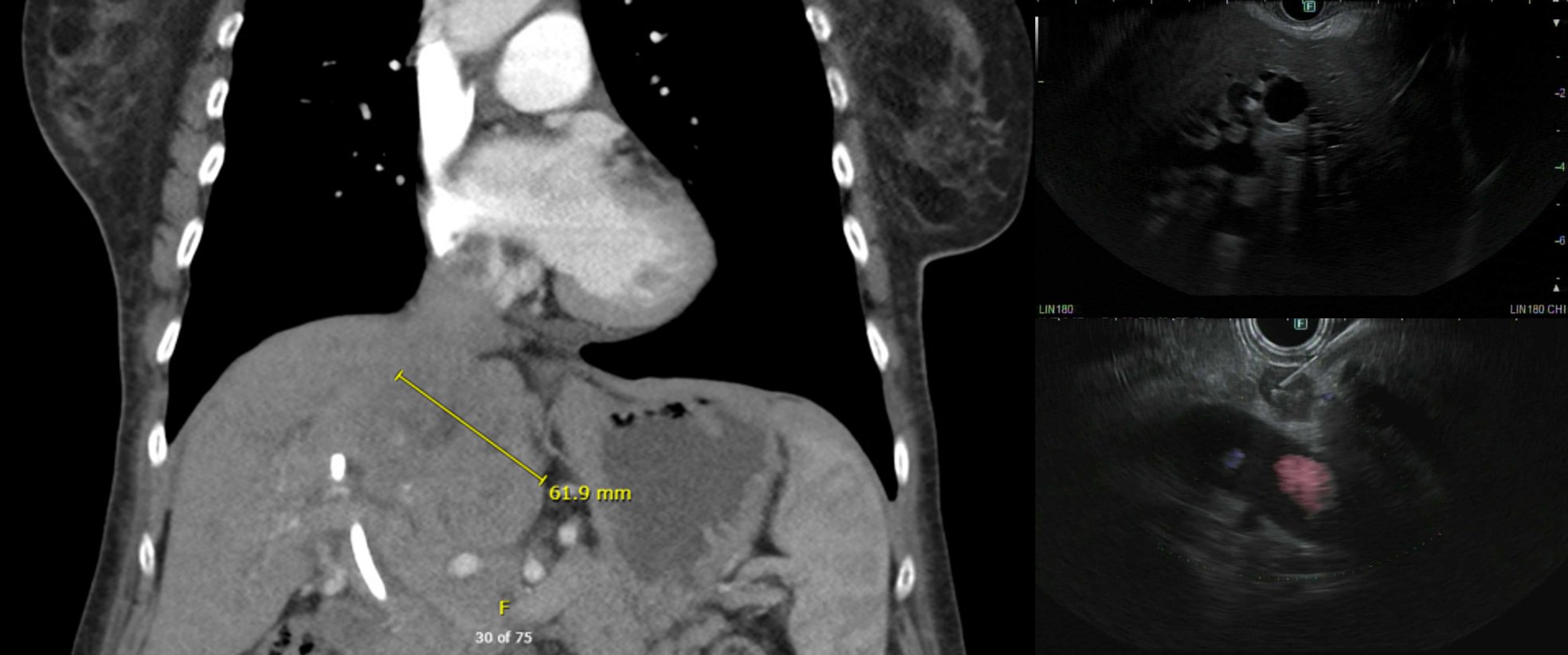
Figure: Left: Fluoroscopy demonstrating cholangioscope in the left common hepatic duct.
Middle and right: ERCP Cholangioscopy
Disclosures:
Abraham Nakshabendi indicated no relevant financial relationships.
Jennie An indicated no relevant financial relationships.
Ramy Mitwalli indicated no relevant financial relationships.
Rahman Nakshabendi indicated no relevant financial relationships.
Abraham Nakshabendi, BS1, Jennie An, BS2, Ramy R. Mitwalli, MD, MBA, MSc3, Rahman Nakshabendi, MD3. P6005 - Painless Obstructive Jaundice Suspected of Malignancy: A Case of IgG4-Related Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
