Monday Poster Session
Category: Liver
P3704 - Real World Impact of Guideline-Adherent Nutritional Support on Outcomes in Hospitalized Patients With Alcohol Associated Hepatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lauren Shaffer, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Lauren Shaffer, MD1, Conrad Fernandes, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Malnutrition is a significant contributor to poor outcomes in alcohol-associated hepatitis (AH). Despite guidelines recommending aggressive nutritional support, the real-world implementation and impact of these recommendations remain poorly understood.
Methods: We conducted a retrospective study of adult patients diagnosed with AH who were admitted to an academic tertiary care center between 1/1/2023 and 12/31/2023. We included patients with probable or definite AH per the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Alcoholic Hepatitis Consortia criteria. Nutritional interventions were categorized as guideline-adherent (≥35 kcal/kg/day with thiamine and folic acid supplementation) or non-adherent. The primary outcome was 90-day mortality. Multivariable Cox-regression models were used to assess the independent association between nutritional guideline adherence and 90-day mortality.
Results: A total of 101 patients with AH were included for analysis. The cohort had a median age of 47 years, with 42% being female, and a median body mass index (BMI) of 28 kg/m2. The median phosphatidylethanol level at admission was 212 ng/dL, and the median Model for End-Stage Liver Disease (MELD) score was 25. Only 20% of patients received guideline-adherent nutritional support. Guideline-adherent nutrition was associated with lower 90-day mortality (5% vs. 25%, p=0.05), but no differences were found in median hospital length of stay (6 vs. 7 days, p</em>=0.31) or need for intensive care unit admission (45% vs. 43%, p=0.89). After adjusting for age, sex, MELD score, and BMI, guideline-adherent nutrition was independently associated with reduced hazards of 90-day mortality (HR 0.11, 95% CI 0.14-0.85, p=0.04) (Figure 1). Subgroup analysis of patients with severe AH, defined as MELD >20 (76% of cohort), showed consistent results, where guideline-adherence was associated with reduced 90-day mortality (HR 0.10, 95% CI 0.10-0.81, p</em>=0.03).
Discussion: In this real-world cohort, only 20% of AH patients received guideline-recommended nutritional support, which was independently associated with an 89% reduction in 90-day mortality risk. These findings underscore the critical need for targeted interventions to improve nutritional support implementation in AH, potentially offering a cost-effective strategy to significantly improve outcomes in this high-risk population.
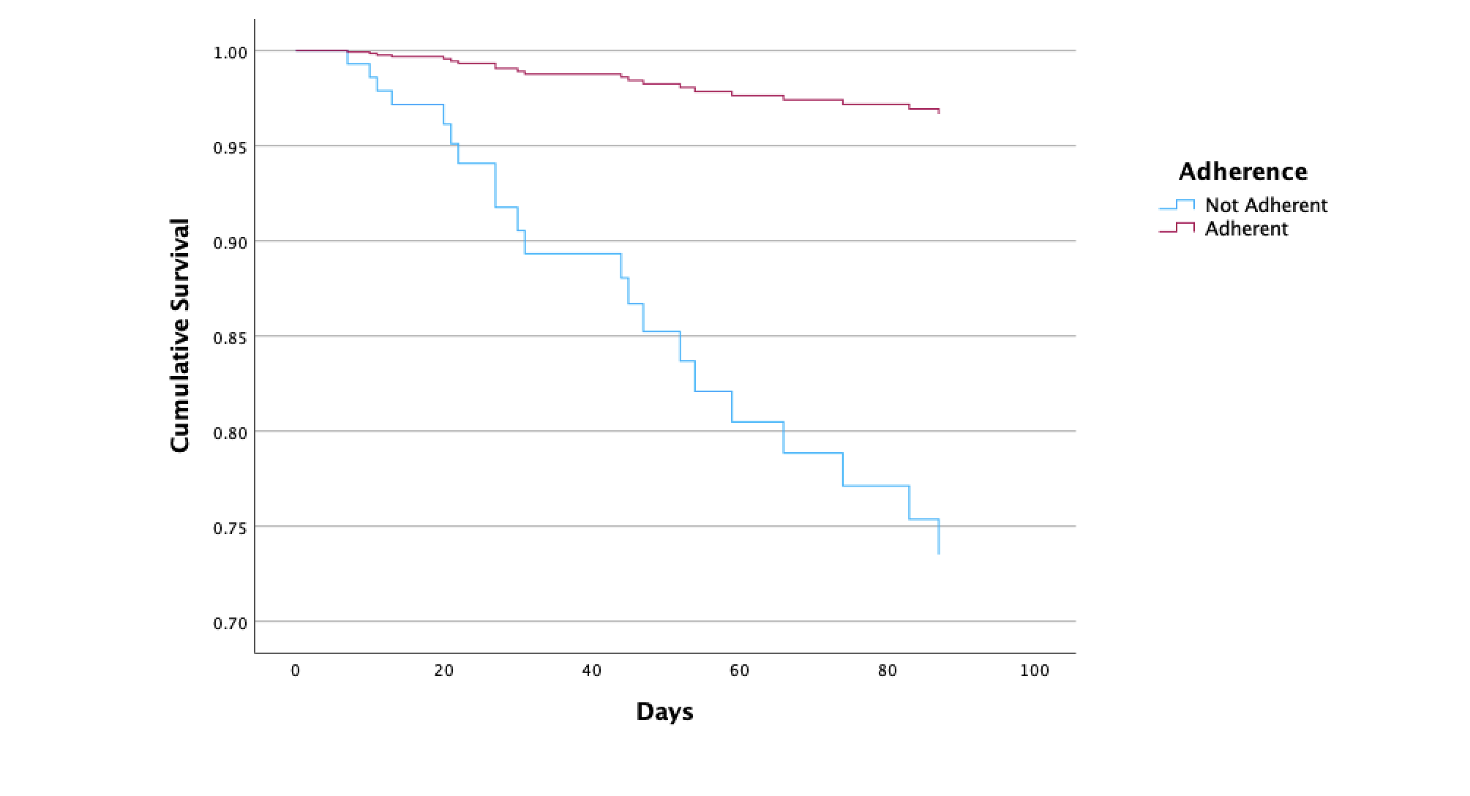
Figure: Figure 1: Comparison of Survival Between Guideline Recommended Nutritional Adherence and Non-Adherence
Disclosures:
Lauren Shaffer indicated no relevant financial relationships.
Conrad Fernandes indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
George Cholankeril indicated no relevant financial relationships.
Ruben Hernaez indicated no relevant financial relationships.
Kavish Patidar: Madrigal Pharmaceuticals – Advisor or Review Panel Member. Mallinckrodt Pharmaceuticals – Consultant.
Lauren Shaffer, MD1, Conrad Fernandes, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2. P3704 - Real World Impact of Guideline-Adherent Nutritional Support on Outcomes in Hospitalized Patients With Alcohol Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Malnutrition is a significant contributor to poor outcomes in alcohol-associated hepatitis (AH). Despite guidelines recommending aggressive nutritional support, the real-world implementation and impact of these recommendations remain poorly understood.
Methods: We conducted a retrospective study of adult patients diagnosed with AH who were admitted to an academic tertiary care center between 1/1/2023 and 12/31/2023. We included patients with probable or definite AH per the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Alcoholic Hepatitis Consortia criteria. Nutritional interventions were categorized as guideline-adherent (≥35 kcal/kg/day with thiamine and folic acid supplementation) or non-adherent. The primary outcome was 90-day mortality. Multivariable Cox-regression models were used to assess the independent association between nutritional guideline adherence and 90-day mortality.
Results: A total of 101 patients with AH were included for analysis. The cohort had a median age of 47 years, with 42% being female, and a median body mass index (BMI) of 28 kg/m2. The median phosphatidylethanol level at admission was 212 ng/dL, and the median Model for End-Stage Liver Disease (MELD) score was 25. Only 20% of patients received guideline-adherent nutritional support. Guideline-adherent nutrition was associated with lower 90-day mortality (5% vs. 25%, p=0.05), but no differences were found in median hospital length of stay (6 vs. 7 days, p</em>=0.31) or need for intensive care unit admission (45% vs. 43%, p=0.89). After adjusting for age, sex, MELD score, and BMI, guideline-adherent nutrition was independently associated with reduced hazards of 90-day mortality (HR 0.11, 95% CI 0.14-0.85, p=0.04) (Figure 1). Subgroup analysis of patients with severe AH, defined as MELD >20 (76% of cohort), showed consistent results, where guideline-adherence was associated with reduced 90-day mortality (HR 0.10, 95% CI 0.10-0.81, p</em>=0.03).
Discussion: In this real-world cohort, only 20% of AH patients received guideline-recommended nutritional support, which was independently associated with an 89% reduction in 90-day mortality risk. These findings underscore the critical need for targeted interventions to improve nutritional support implementation in AH, potentially offering a cost-effective strategy to significantly improve outcomes in this high-risk population.
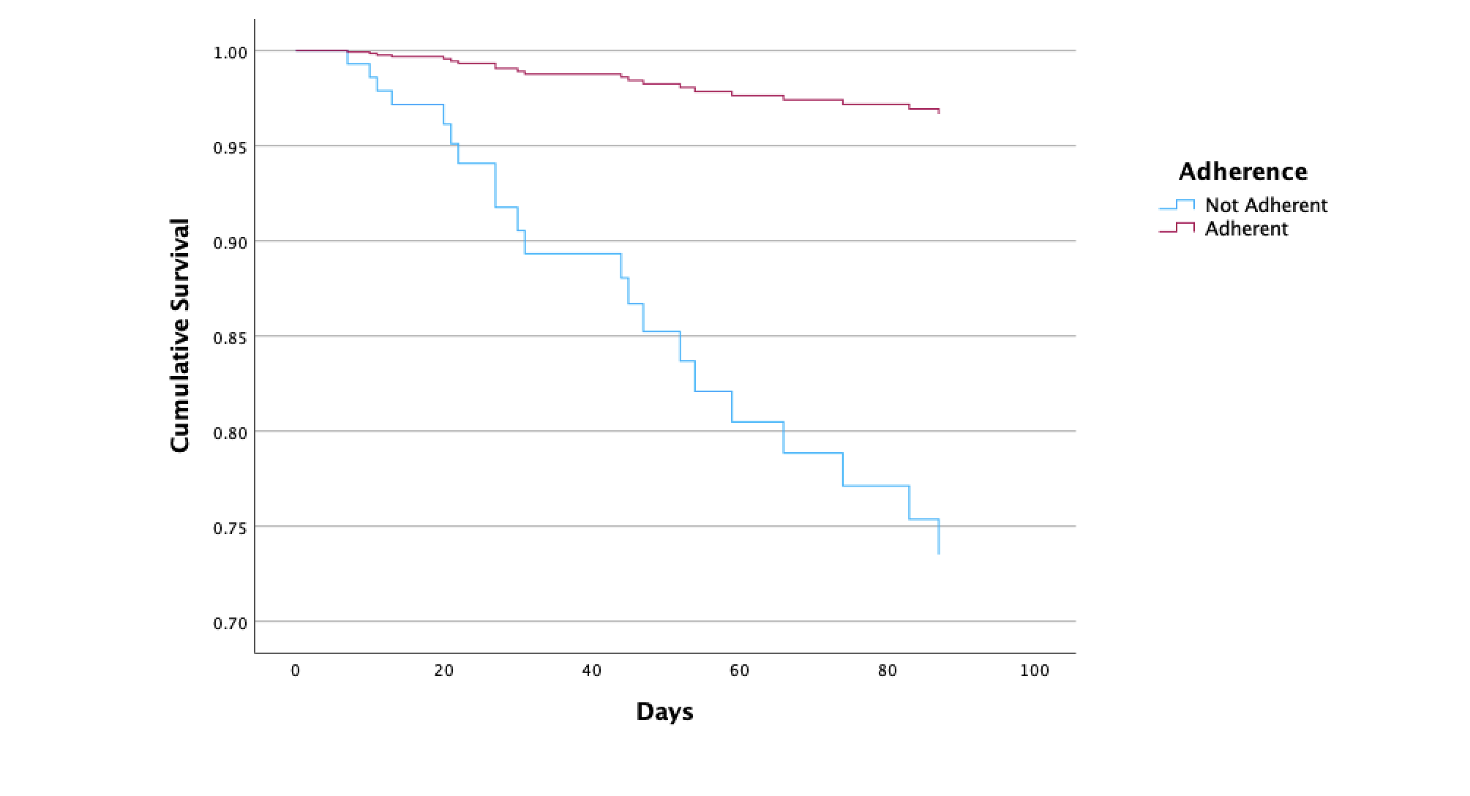
Figure: Figure 1: Comparison of Survival Between Guideline Recommended Nutritional Adherence and Non-Adherence
Disclosures:
Lauren Shaffer indicated no relevant financial relationships.
Conrad Fernandes indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
George Cholankeril indicated no relevant financial relationships.
Ruben Hernaez indicated no relevant financial relationships.
Kavish Patidar: Madrigal Pharmaceuticals – Advisor or Review Panel Member. Mallinckrodt Pharmaceuticals – Consultant.
Lauren Shaffer, MD1, Conrad Fernandes, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2. P3704 - Real World Impact of Guideline-Adherent Nutritional Support on Outcomes in Hospitalized Patients With Alcohol Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

