Monday Poster Session
Category: Liver
P3692 - GLP-1 Analogs in Cirrhosis: Reduced Mortality and Fewer Complications in a National Cohort
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chidera Onwuzo, MBBS (he/him/his)
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Antoine Boustany, MD4, Sahith Kaki, BS5, Rashid Abdel-Razeq, MD6, Vishal Busa, MD1, Tavankit Singh, MD3
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4University of Florida College of Medicine, Jacksonville, FL; 5Lake Erie College of Osteopathic Medicine - Erie, Erie, PA; 6Cleveland Clinic Foundation, Cleveland, OH
Introduction: Cirrhosis is a chronic liver disease marked by progressive dysfunction and complications such as hepatic encephalopathy (HE), hepatorenal syndrome (HRS), and variceal bleeding. Glucagon-like peptide-1 (GLP-1) analogs, originally developed for type 2 diabetes, have shown promise in improving metabolic function and reducing hepatic inflammation. This study evaluates the impact of GLP-1 therapy on mortality and key clinical outcomes in patients with cirrhosis.
Methods: We conducted a retrospective analysis using deidentified data from the TriNetX research network, comprising over 130 million patients across 70+ U.S. healthcare systems. Adults (≥18 years) with cirrhosis were identified, and those prescribed GLP-1 analogs post-diagnosis were selected. Primary outcomes included all-cause mortality, HE, HRS, and portal hypertensive bleeding. Propensity score matching (1:1) accounted for confounders such as age, sex, race, diabetes, obesity, hypertension, CKD, tobacco use, and alcohol dependence. Matched cohorts were analyzed using Cox proportional hazards regression to generate hazard ratios (HR) with 95% confidence intervals (CI).
Results: GLP-1 analog use was associated with reduced risk of several cirrhosis complications. Users had significantly lower all-cause mortality (HR 0.374; 95% CI 0.359–0.392), HE (HR 0.900; 95% CI 0.843–0.959), HRS (HR 0.554; 95% CI 0.496–0.619), and portal hypertensive bleeding (HR 0.487; 95% CI 0.444–0.533). These findings indicate that GLP-1 therapy may mitigate both mortality and critical cirrhosis-related complications.
Discussion: GLP-1 analog use in cirrhotic patients is linked to lower mortality and reduced risk of HE, HRS, and variceal bleeding. The potential for fewer bleeding events may translate into decreased hospitalizations and improved quality of life. These findings support the consideration of GLP-1 therapy as a complementary strategy in cirrhosis management to enhance patient outcomes and reduce acute care burden.
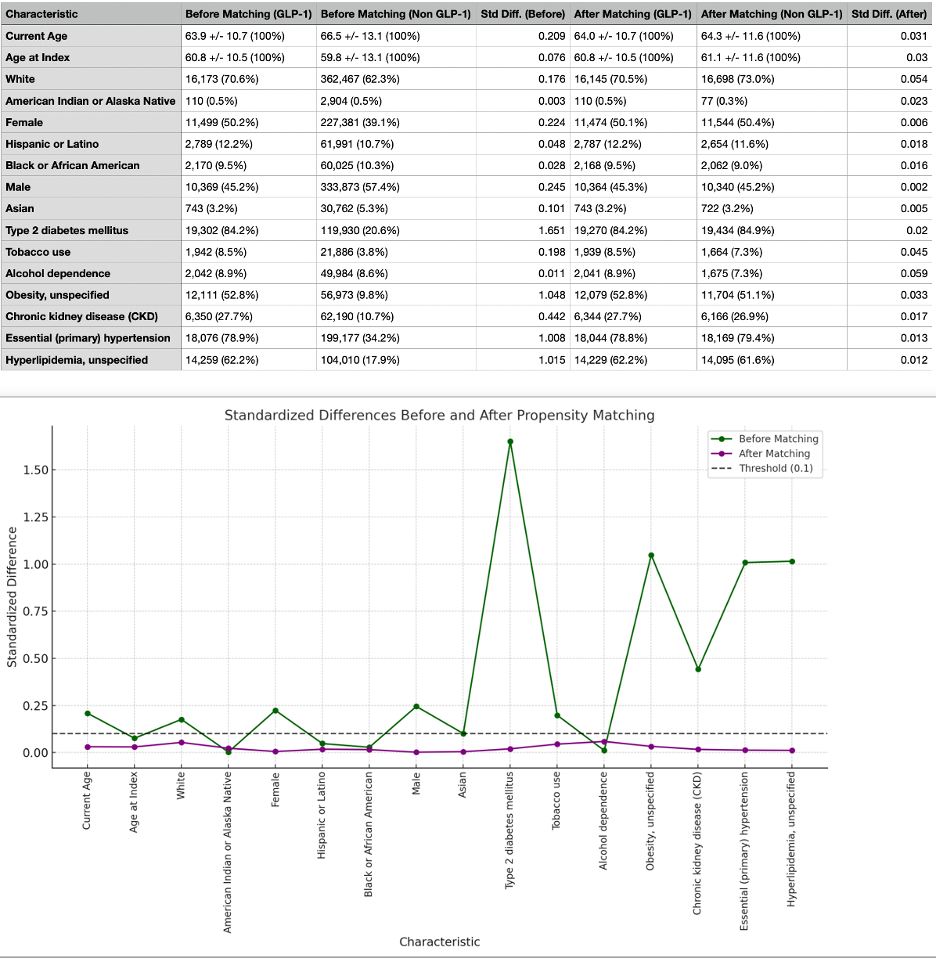
Figure: Figure 1: Comparison of Demographics and Comorbidities of GLP-1 Analog Users and Non-GLP-1 Analog Users Before and After Propensity Score Matching
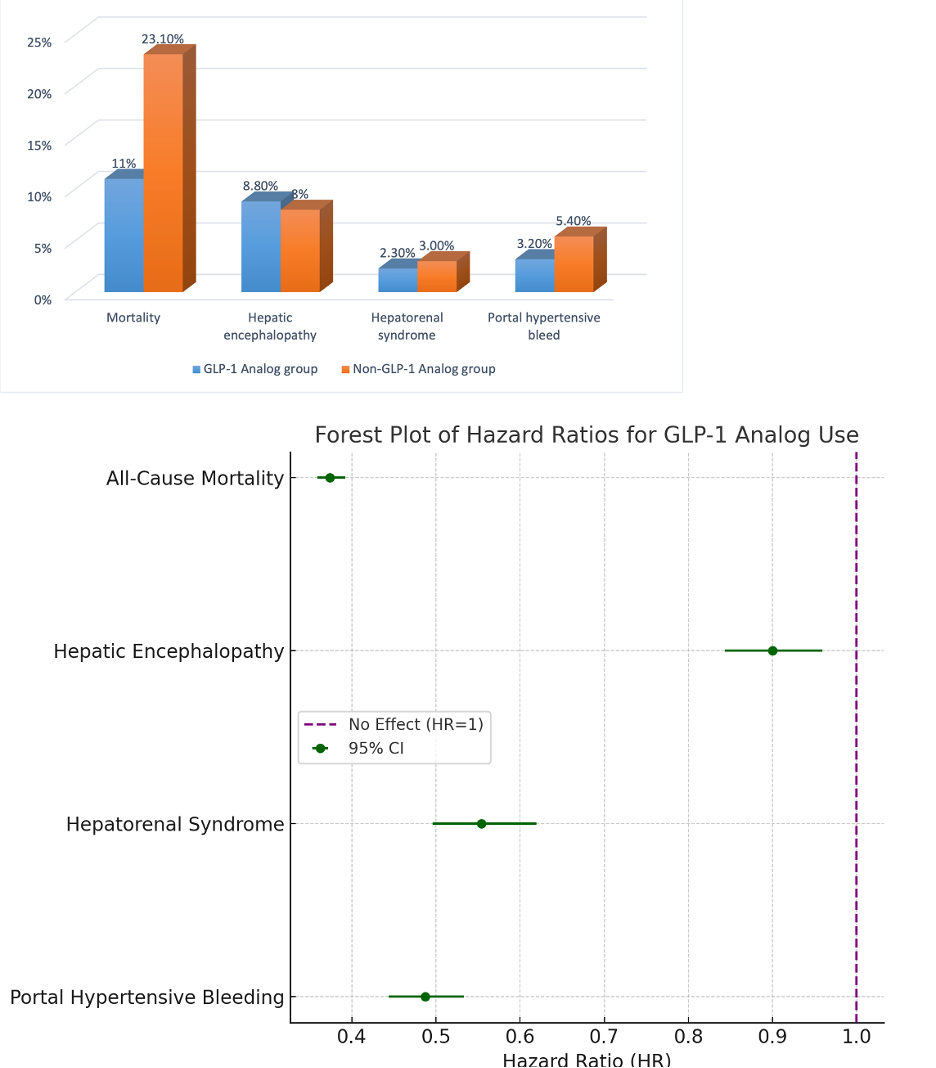
Figure: Figure 2: Bar chart showing complication rates & Forest plot comparing hazard ratios for events in GLP analog group vs non-GLP analog group.
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Sahith Kaki indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Vishal Busa indicated no relevant financial relationships.
Tavankit Singh indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Antoine Boustany, MD4, Sahith Kaki, BS5, Rashid Abdel-Razeq, MD6, Vishal Busa, MD1, Tavankit Singh, MD3. P3692 - GLP-1 Analogs in Cirrhosis: Reduced Mortality and Fewer Complications in a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4University of Florida College of Medicine, Jacksonville, FL; 5Lake Erie College of Osteopathic Medicine - Erie, Erie, PA; 6Cleveland Clinic Foundation, Cleveland, OH
Introduction: Cirrhosis is a chronic liver disease marked by progressive dysfunction and complications such as hepatic encephalopathy (HE), hepatorenal syndrome (HRS), and variceal bleeding. Glucagon-like peptide-1 (GLP-1) analogs, originally developed for type 2 diabetes, have shown promise in improving metabolic function and reducing hepatic inflammation. This study evaluates the impact of GLP-1 therapy on mortality and key clinical outcomes in patients with cirrhosis.
Methods: We conducted a retrospective analysis using deidentified data from the TriNetX research network, comprising over 130 million patients across 70+ U.S. healthcare systems. Adults (≥18 years) with cirrhosis were identified, and those prescribed GLP-1 analogs post-diagnosis were selected. Primary outcomes included all-cause mortality, HE, HRS, and portal hypertensive bleeding. Propensity score matching (1:1) accounted for confounders such as age, sex, race, diabetes, obesity, hypertension, CKD, tobacco use, and alcohol dependence. Matched cohorts were analyzed using Cox proportional hazards regression to generate hazard ratios (HR) with 95% confidence intervals (CI).
Results: GLP-1 analog use was associated with reduced risk of several cirrhosis complications. Users had significantly lower all-cause mortality (HR 0.374; 95% CI 0.359–0.392), HE (HR 0.900; 95% CI 0.843–0.959), HRS (HR 0.554; 95% CI 0.496–0.619), and portal hypertensive bleeding (HR 0.487; 95% CI 0.444–0.533). These findings indicate that GLP-1 therapy may mitigate both mortality and critical cirrhosis-related complications.
Discussion: GLP-1 analog use in cirrhotic patients is linked to lower mortality and reduced risk of HE, HRS, and variceal bleeding. The potential for fewer bleeding events may translate into decreased hospitalizations and improved quality of life. These findings support the consideration of GLP-1 therapy as a complementary strategy in cirrhosis management to enhance patient outcomes and reduce acute care burden.
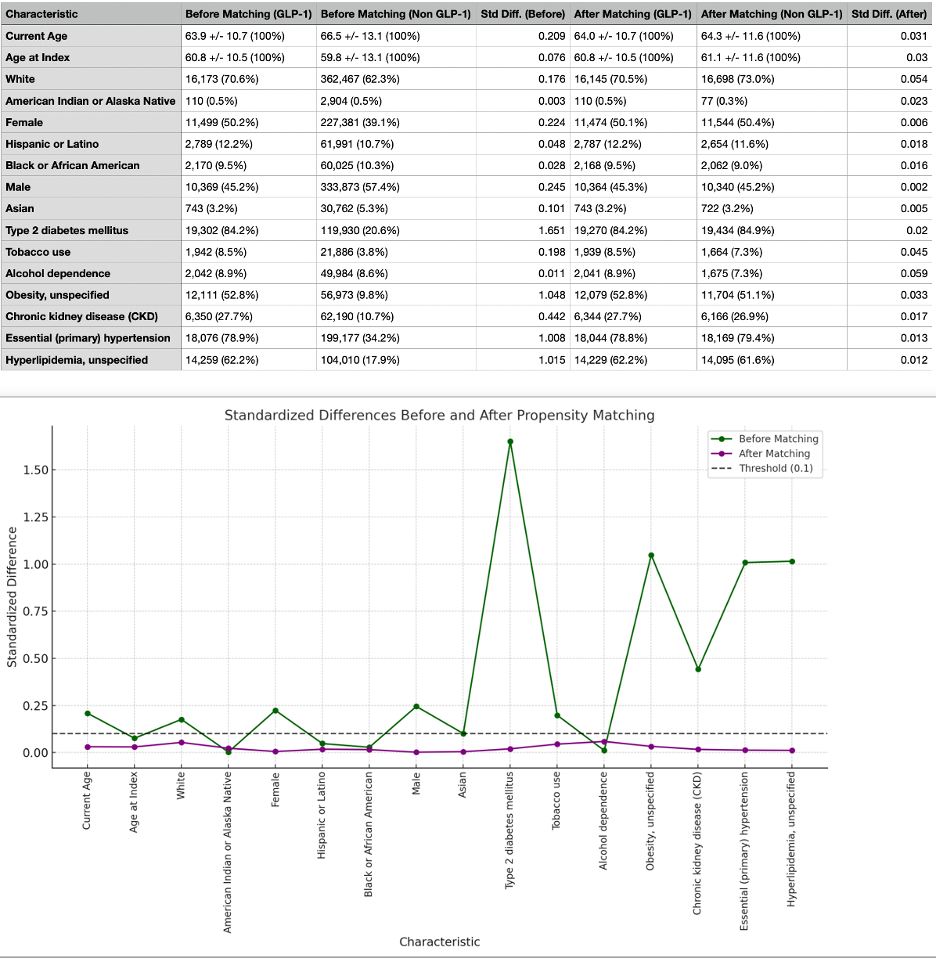
Figure: Figure 1: Comparison of Demographics and Comorbidities of GLP-1 Analog Users and Non-GLP-1 Analog Users Before and After Propensity Score Matching
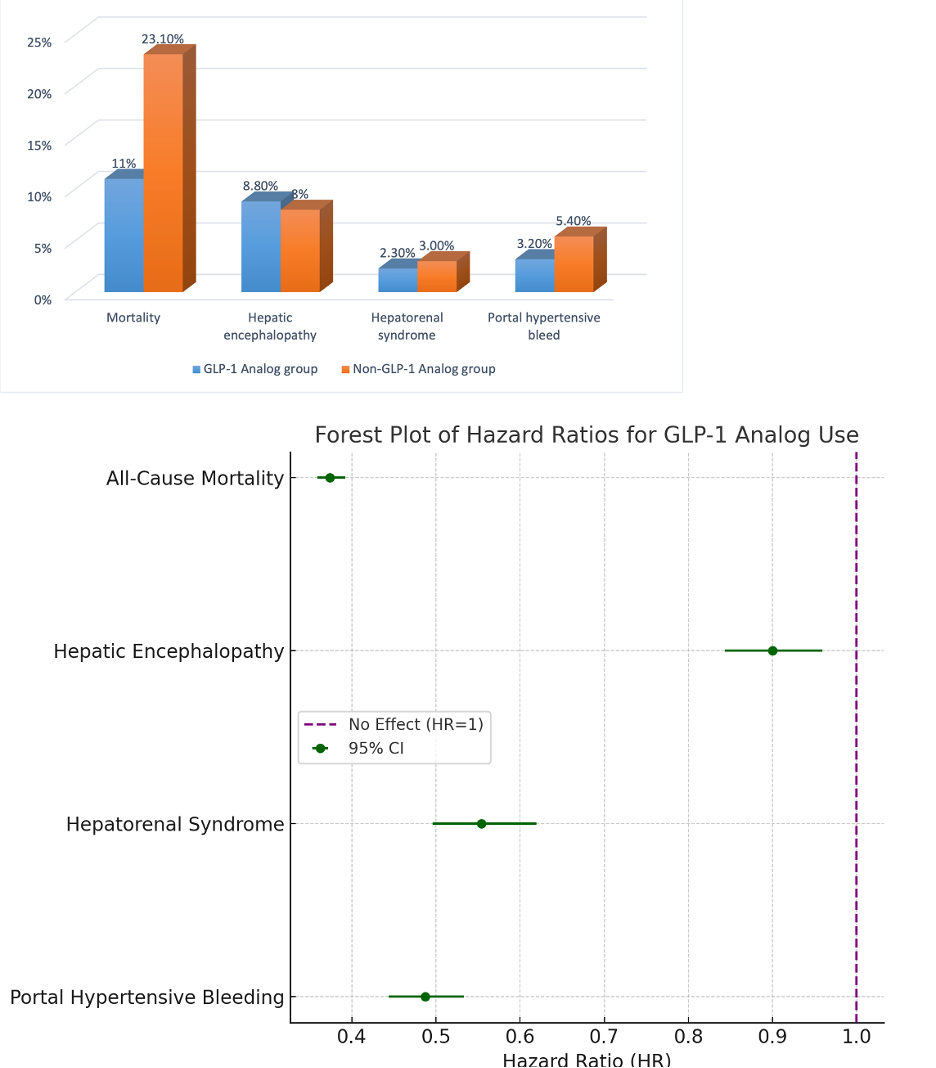
Figure: Figure 2: Bar chart showing complication rates & Forest plot comparing hazard ratios for events in GLP analog group vs non-GLP analog group.
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Sahith Kaki indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Vishal Busa indicated no relevant financial relationships.
Tavankit Singh indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Antoine Boustany, MD4, Sahith Kaki, BS5, Rashid Abdel-Razeq, MD6, Vishal Busa, MD1, Tavankit Singh, MD3. P3692 - GLP-1 Analogs in Cirrhosis: Reduced Mortality and Fewer Complications in a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
