Monday Poster Session
Category: Liver
P3691 - GLP-1 Analogs Linked to Lower Ascites, Paracentesis, and SBP Rates in Cirrhosis: Insights From a Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chidera Onwuzo, MBBS (he/him/his)
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Sharifeh Almasaid, MD, MPH5, Antoine Boustany, MD6, Al-Aman Shaukat, MBBS1
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5SUNY Upstate Medical University, Syracuse, NY; 6University of Florida College of Medicine, Jacksonville, FL
Introduction: Cirrhosis is a chronic liver condition marked by progressive dysfunction, leading to serious complications such as ascites, spontaneous bacterial peritonitis (SBP), and the need for paracentesis or transjugularintrahepatic portosystemic shunt (TIPS). Historically, management has focused on symptom control and preventing further liver damage. Glucagon-like peptide-1 (GLP-1) analogs, originally developed for type 2 diabetes, have recently drawn attention for potential liver-related benefits. Emerging data suggest GLP-1 agents may improve metabolic function and reduce inflammation, potentially lowering cirrhosis-related complications.
Methods: We conducted a retrospective analysis using the TriNetX research network. Adults (≥18 years) with cirrhosis were included. Patients who initiated GLP-1 therapy after cirrhosis diagnosis were identified. Primary outcomes included the incidence of ascites, SBP, paracentesis, and TIPS. To minimize confounding, 1:1 propensity score matching was performed based on demographics, comorbidities (e.g., diabetes, obesity, CKD, hypertension), and lifestyle factors (e.g., alcohol, tobacco use). Cox proportional hazards regression analysis was used to assess associations, and hazard ratios (HRs) with 95% confidence intervals (CI) were reported.
Results: The matched cohort analysis, which included 22,889 patients in both the GLP-1-treated and non-treated groups, revealed that GLP-1 analog use was significantly associated with a reduced risk of key cirrhosis- related complications. Patients treated with GLP-1 analogs exhibited a significantly lower risk of developing ascites (HR 0.499, 95% CI 0.480–0.520), requiring paracentesis (HR 0.379, 95% CI 0.352– 0.407), and experiencing spontaneous bacterial peritonitis (HR 0.454, 95% CI 0.403–0.513). Additionally, there was a trend toward reduced risk of undergoing TIPS procedures (HR 0.653, 95% CI 0.338–1.262).
Discussion: The matched cohort analysis, which included 22,889 patients in both the GLP-1-treated and non-treated groups, revealed that GLP-1 analog use was significantly associated with a reduced risk of key cirrhosis- related complications. Patients treated with GLP-1 analogs exhibited a significantly lower risk of developing ascites (HR 0.499, 95% CI 0.480–0.520), requiring paracentesis (HR 0.379, 95% CI 0.352– 0.407), and experiencing spontaneous bacterial peritonitis (HR 0.454, 95% CI 0.403–0.513). Additionally, there was a trend toward reduced risk of undergoing TIPS procedures (HR 0.653, 95% CI 0.338–1.262).
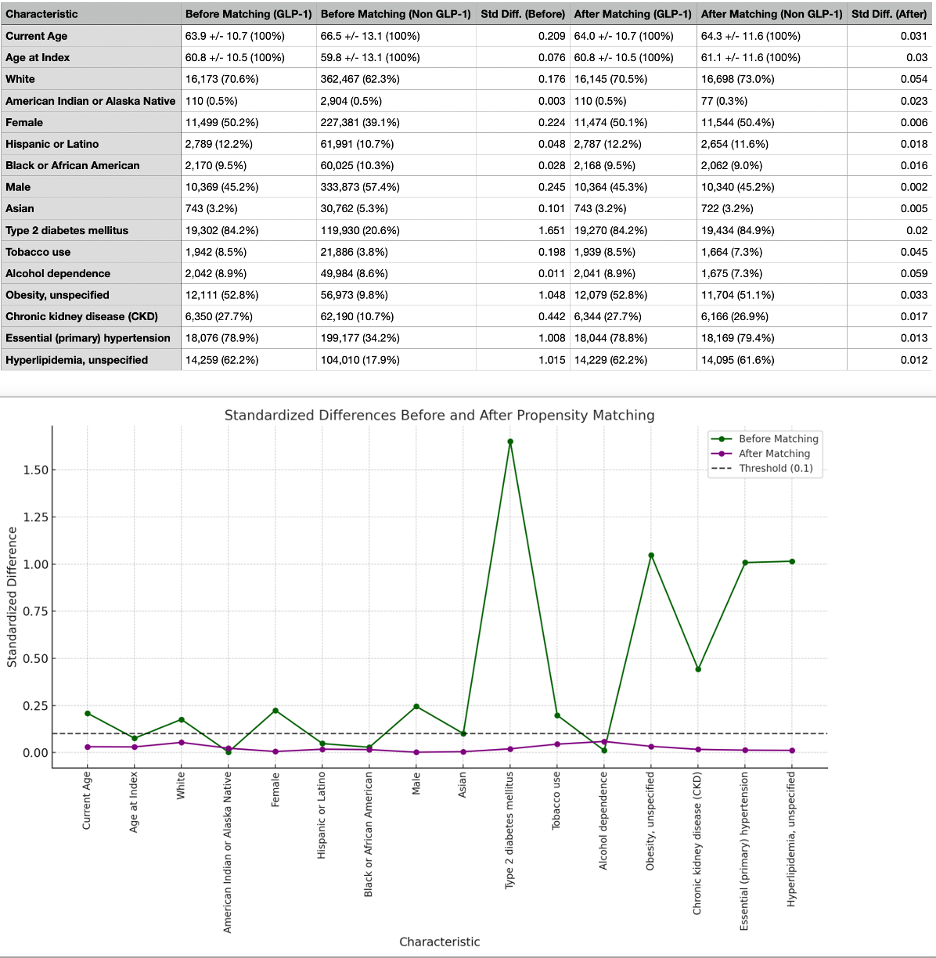
Figure: Figure 1: Comparison of Demographics and Comorbidities of GLP-1 Analog Users and Non-GLP-1 Analog Users Before and After Propensity Score Matching
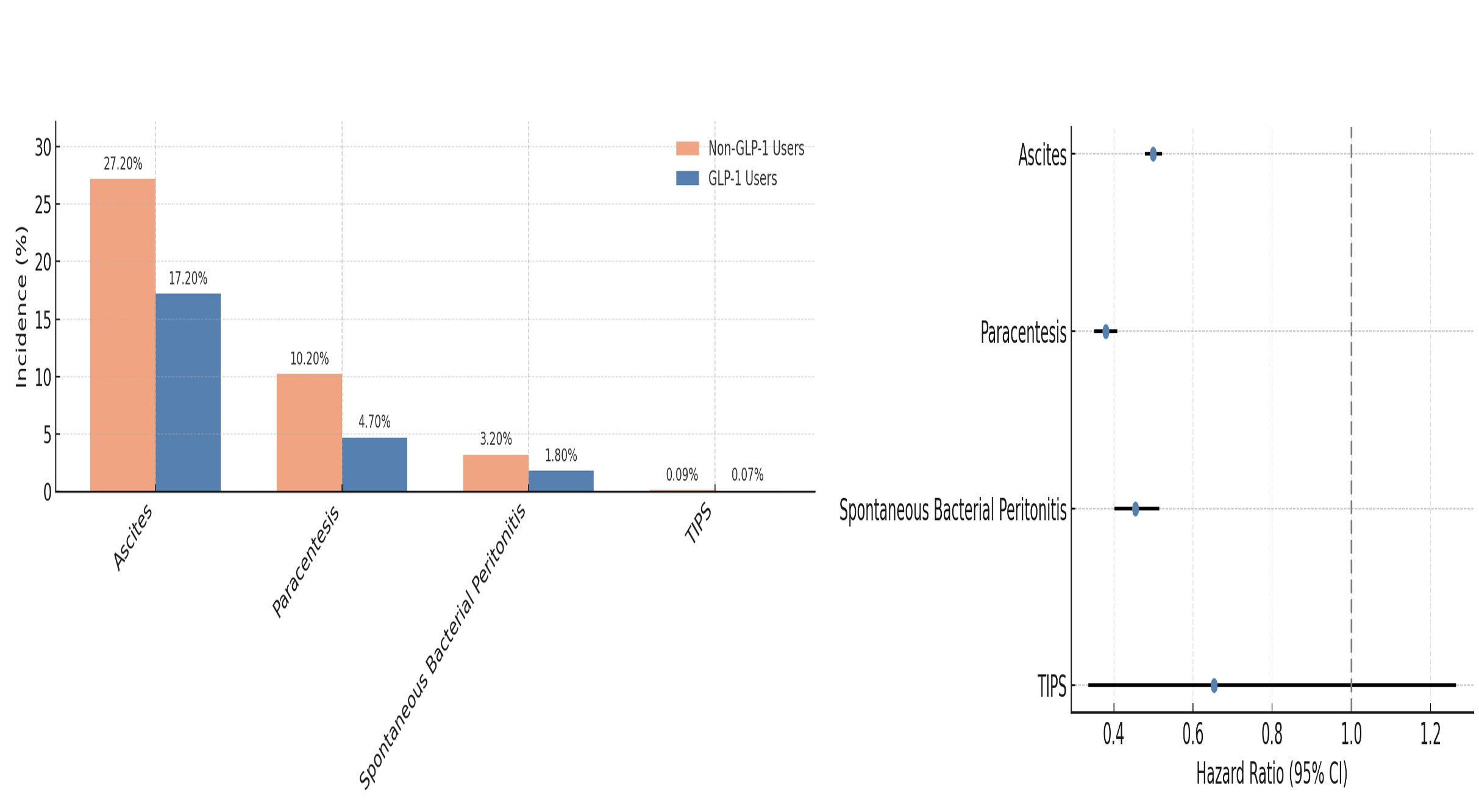
Figure: Figure 2: Risk of complications & Forest plot comparing Hazard ratios for in GLP-1 analog group versus non-GLP-1 analog group
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Al-Aman Shaukat indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Sharifeh Almasaid, MD, MPH5, Antoine Boustany, MD6, Al-Aman Shaukat, MBBS1. P3691 - GLP-1 Analogs Linked to Lower Ascites, Paracentesis, and SBP Rates in Cirrhosis: Insights From a Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5SUNY Upstate Medical University, Syracuse, NY; 6University of Florida College of Medicine, Jacksonville, FL
Introduction: Cirrhosis is a chronic liver condition marked by progressive dysfunction, leading to serious complications such as ascites, spontaneous bacterial peritonitis (SBP), and the need for paracentesis or transjugularintrahepatic portosystemic shunt (TIPS). Historically, management has focused on symptom control and preventing further liver damage. Glucagon-like peptide-1 (GLP-1) analogs, originally developed for type 2 diabetes, have recently drawn attention for potential liver-related benefits. Emerging data suggest GLP-1 agents may improve metabolic function and reduce inflammation, potentially lowering cirrhosis-related complications.
Methods: We conducted a retrospective analysis using the TriNetX research network. Adults (≥18 years) with cirrhosis were included. Patients who initiated GLP-1 therapy after cirrhosis diagnosis were identified. Primary outcomes included the incidence of ascites, SBP, paracentesis, and TIPS. To minimize confounding, 1:1 propensity score matching was performed based on demographics, comorbidities (e.g., diabetes, obesity, CKD, hypertension), and lifestyle factors (e.g., alcohol, tobacco use). Cox proportional hazards regression analysis was used to assess associations, and hazard ratios (HRs) with 95% confidence intervals (CI) were reported.
Results: The matched cohort analysis, which included 22,889 patients in both the GLP-1-treated and non-treated groups, revealed that GLP-1 analog use was significantly associated with a reduced risk of key cirrhosis- related complications. Patients treated with GLP-1 analogs exhibited a significantly lower risk of developing ascites (HR 0.499, 95% CI 0.480–0.520), requiring paracentesis (HR 0.379, 95% CI 0.352– 0.407), and experiencing spontaneous bacterial peritonitis (HR 0.454, 95% CI 0.403–0.513). Additionally, there was a trend toward reduced risk of undergoing TIPS procedures (HR 0.653, 95% CI 0.338–1.262).
Discussion: The matched cohort analysis, which included 22,889 patients in both the GLP-1-treated and non-treated groups, revealed that GLP-1 analog use was significantly associated with a reduced risk of key cirrhosis- related complications. Patients treated with GLP-1 analogs exhibited a significantly lower risk of developing ascites (HR 0.499, 95% CI 0.480–0.520), requiring paracentesis (HR 0.379, 95% CI 0.352– 0.407), and experiencing spontaneous bacterial peritonitis (HR 0.454, 95% CI 0.403–0.513). Additionally, there was a trend toward reduced risk of undergoing TIPS procedures (HR 0.653, 95% CI 0.338–1.262).
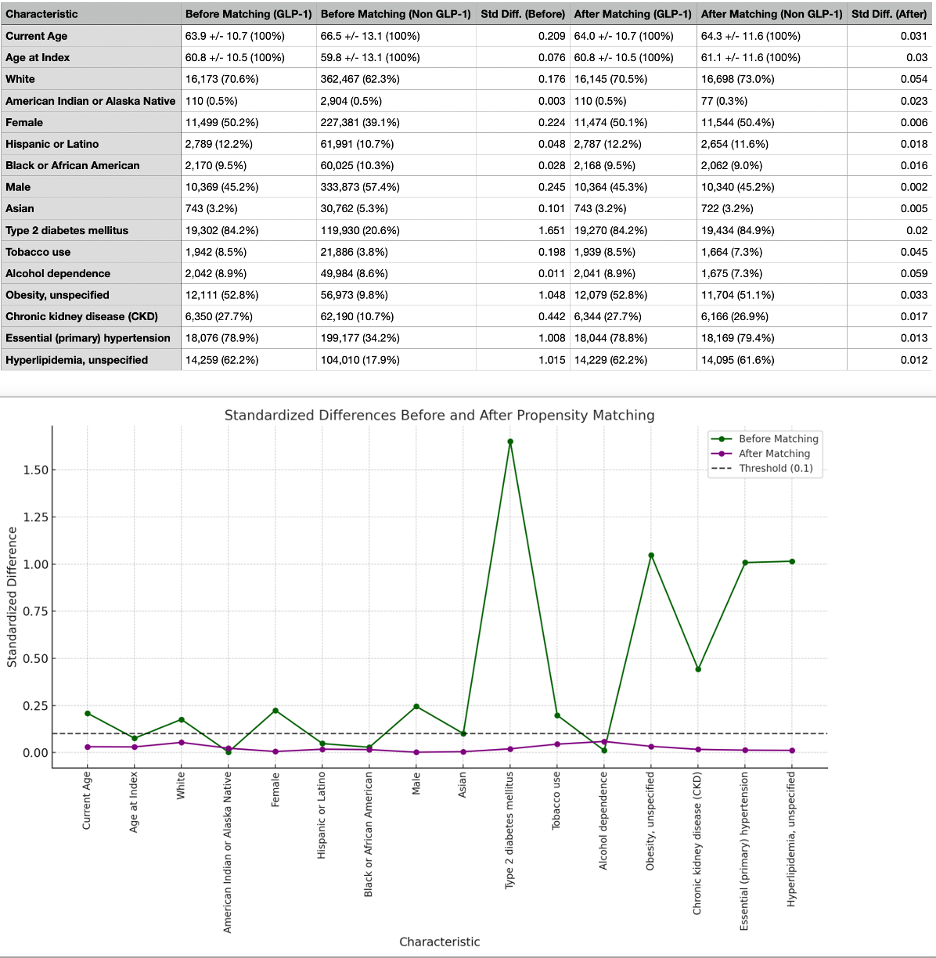
Figure: Figure 1: Comparison of Demographics and Comorbidities of GLP-1 Analog Users and Non-GLP-1 Analog Users Before and After Propensity Score Matching
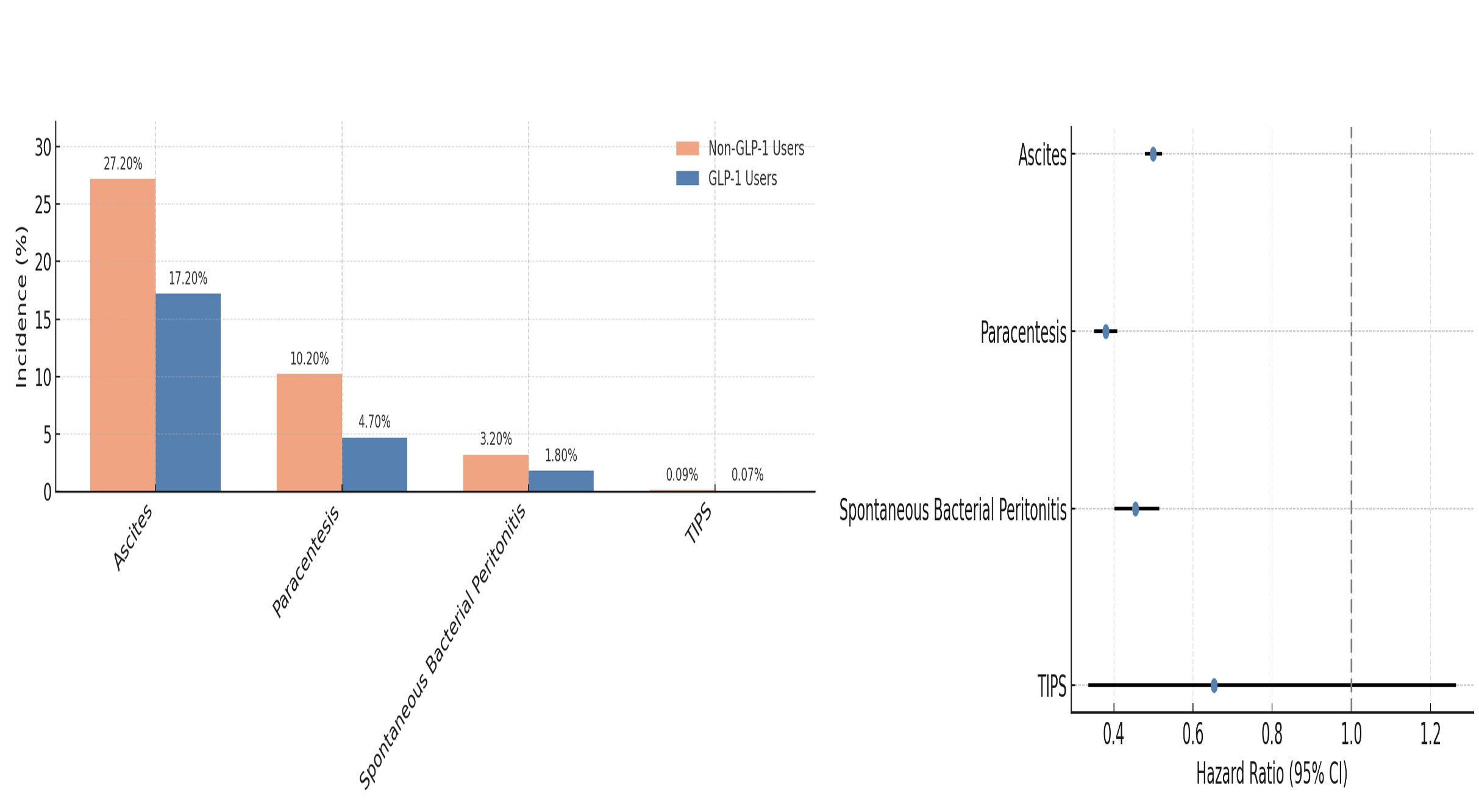
Figure: Figure 2: Risk of complications & Forest plot comparing Hazard ratios for in GLP-1 analog group versus non-GLP-1 analog group
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Al-Aman Shaukat indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Sharifeh Almasaid, MD, MPH5, Antoine Boustany, MD6, Al-Aman Shaukat, MBBS1. P3691 - GLP-1 Analogs Linked to Lower Ascites, Paracentesis, and SBP Rates in Cirrhosis: Insights From a Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
