Monday Poster Session
Category: Liver
P3664 - Impact of COVID-19 on Outcomes in Patients With Acute Alcoholic Hepatitis: A Propensity-Matched Analysis Using a National Federated Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Miguel Salazar, MD2, Khaled Al Smadi, MD3, Zeid Kayali, MD, MBA4
1University of California Riverside School of Medicine, Riverside, CA; 2University of California Riverside School of Medicine, Rialto, CA; 3University of California Riverside, Riverside, CA; 4Riverside Community Hospital, Riverside, CA
Introduction: The surge in excessive alcohol drinking during the COVID-19 pandemic had led to rising incidence of Acute Alcoholic hepatitis (AAH) nationwide. AAH is a life-threatening condition with poor outcome as these patients usually are not transplant candidates. The impact of COVID-19 infection on AAH survival has been scarcely documented. We aim to evaluate the impact of concomitant COVID-19 infection on clinical outcomes in patients with AAH using a large national federated dataset.
Methods: Using the TriNetX US Collaborative Network, we conducted a retrospective cohort study comparing patients with AAH and COVID-19 (Cohort A, n=6,593) to patients with AAH without COVID-19 (Cohort B, n=6,593) from January 2020 to May 2023. Propensity score matching (PSM) was performed on demographic and clinical covariates. Outcomes assessed included mortality, intubation, sepsis, and shock. Kaplan-Meier survival analysis and Cox proportional hazards modeling were used.
Results: After PSM, 6,593 patients were included in each cohort. The mean follow-up duration was similar between groups, with a median of 749 days for the COVID-19 group and 673 days for the non-COVID group. Interestingly, the mortality rate was significantly lower in patients with AAH and concurrent COVID-19 compared to those without COVID-19, with a hazard ratio (HR) of 0.831 (p< 0.001) and a higher survival probability at the end of the study period (68.88% vs. 61.24%). There was no statistically significant difference in the risk of intubation between the groups (HR: 1.079, p=0.597), and Kaplan-Meier analysis showed overlapping survival curves for this outcome. Similarly, while patients in the COVID-19 group had a slightly higher incidence of sepsis, the difference did not reach statistical significance (HR: 1.092, p=0.078). For the outcome of shock, hazard ratios were nearly identical between groups, indicating no meaningful difference (HR: 0.961, p=1.000). Overall, the presence of COVID-19 in patients with AAH did not worsen critical care outcomes such as intubation, sepsis, or shock, and was paradoxically associated with lower mortality.
Discussion: Surprisingly, patients with AAH and concurrent COVID-19 had lower mortality compared to matched patients with AAH alone. Rates of intubation, sepsis, and shock were comparable. These findings highlight the evolving clinical management and outcomes of comorbid COVID-19 in liver disease and warrant further investigation.
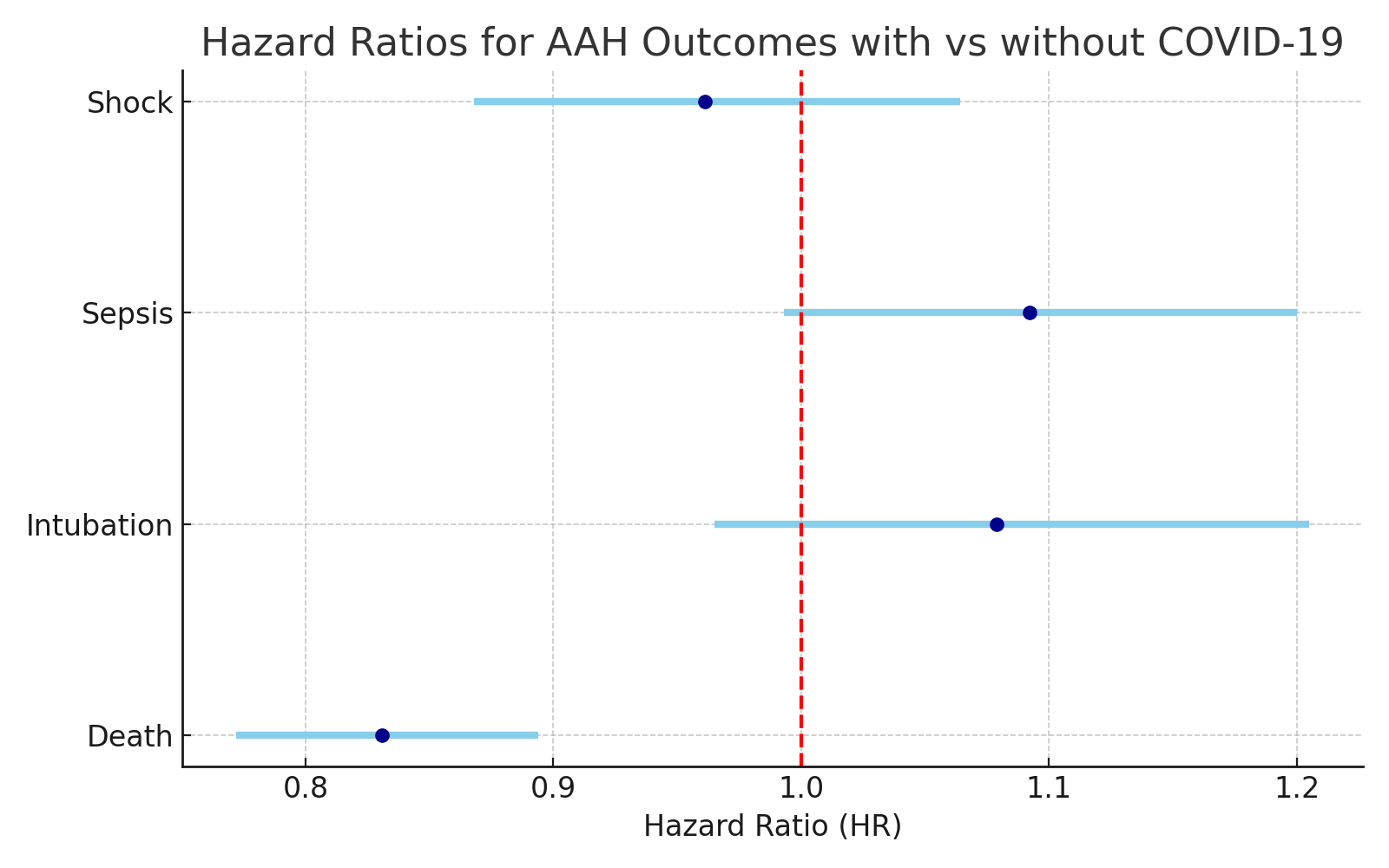
Figure: Figure 1: Hazard ratios for AAH outcomes with and without COVID-19
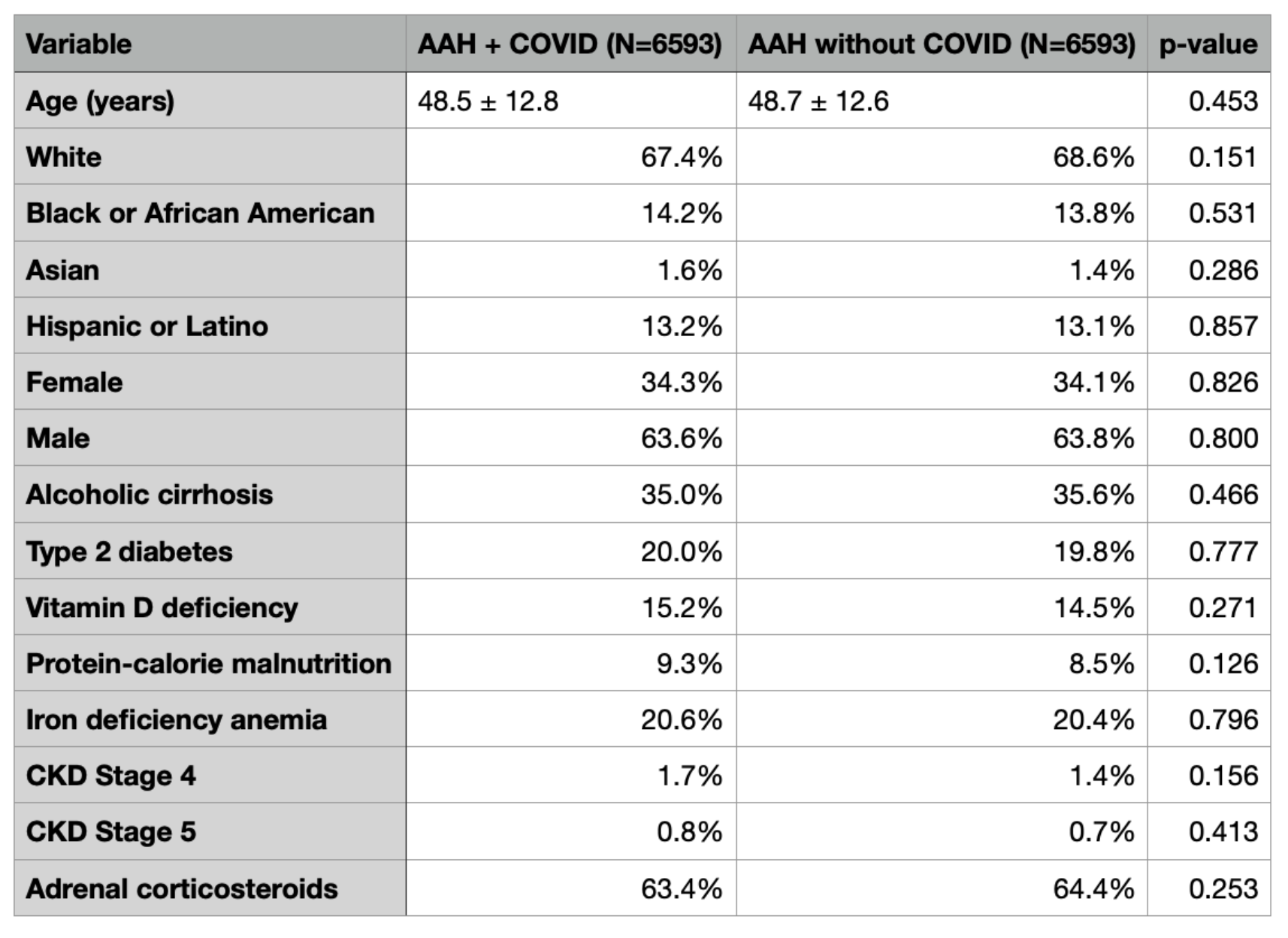
Figure: Table 1: Patient demographics and baseline characterstics after propensity score matching
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Miguel Salazar indicated no relevant financial relationships.
Khaled Al Smadi indicated no relevant financial relationships.
Zeid Kayali indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Miguel Salazar, MD2, Khaled Al Smadi, MD3, Zeid Kayali, MD, MBA4. P3664 - Impact of COVID-19 on Outcomes in Patients With Acute Alcoholic Hepatitis: A Propensity-Matched Analysis Using a National Federated Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2University of California Riverside School of Medicine, Rialto, CA; 3University of California Riverside, Riverside, CA; 4Riverside Community Hospital, Riverside, CA
Introduction: The surge in excessive alcohol drinking during the COVID-19 pandemic had led to rising incidence of Acute Alcoholic hepatitis (AAH) nationwide. AAH is a life-threatening condition with poor outcome as these patients usually are not transplant candidates. The impact of COVID-19 infection on AAH survival has been scarcely documented. We aim to evaluate the impact of concomitant COVID-19 infection on clinical outcomes in patients with AAH using a large national federated dataset.
Methods: Using the TriNetX US Collaborative Network, we conducted a retrospective cohort study comparing patients with AAH and COVID-19 (Cohort A, n=6,593) to patients with AAH without COVID-19 (Cohort B, n=6,593) from January 2020 to May 2023. Propensity score matching (PSM) was performed on demographic and clinical covariates. Outcomes assessed included mortality, intubation, sepsis, and shock. Kaplan-Meier survival analysis and Cox proportional hazards modeling were used.
Results: After PSM, 6,593 patients were included in each cohort. The mean follow-up duration was similar between groups, with a median of 749 days for the COVID-19 group and 673 days for the non-COVID group. Interestingly, the mortality rate was significantly lower in patients with AAH and concurrent COVID-19 compared to those without COVID-19, with a hazard ratio (HR) of 0.831 (p< 0.001) and a higher survival probability at the end of the study period (68.88% vs. 61.24%). There was no statistically significant difference in the risk of intubation between the groups (HR: 1.079, p=0.597), and Kaplan-Meier analysis showed overlapping survival curves for this outcome. Similarly, while patients in the COVID-19 group had a slightly higher incidence of sepsis, the difference did not reach statistical significance (HR: 1.092, p=0.078). For the outcome of shock, hazard ratios were nearly identical between groups, indicating no meaningful difference (HR: 0.961, p=1.000). Overall, the presence of COVID-19 in patients with AAH did not worsen critical care outcomes such as intubation, sepsis, or shock, and was paradoxically associated with lower mortality.
Discussion: Surprisingly, patients with AAH and concurrent COVID-19 had lower mortality compared to matched patients with AAH alone. Rates of intubation, sepsis, and shock were comparable. These findings highlight the evolving clinical management and outcomes of comorbid COVID-19 in liver disease and warrant further investigation.
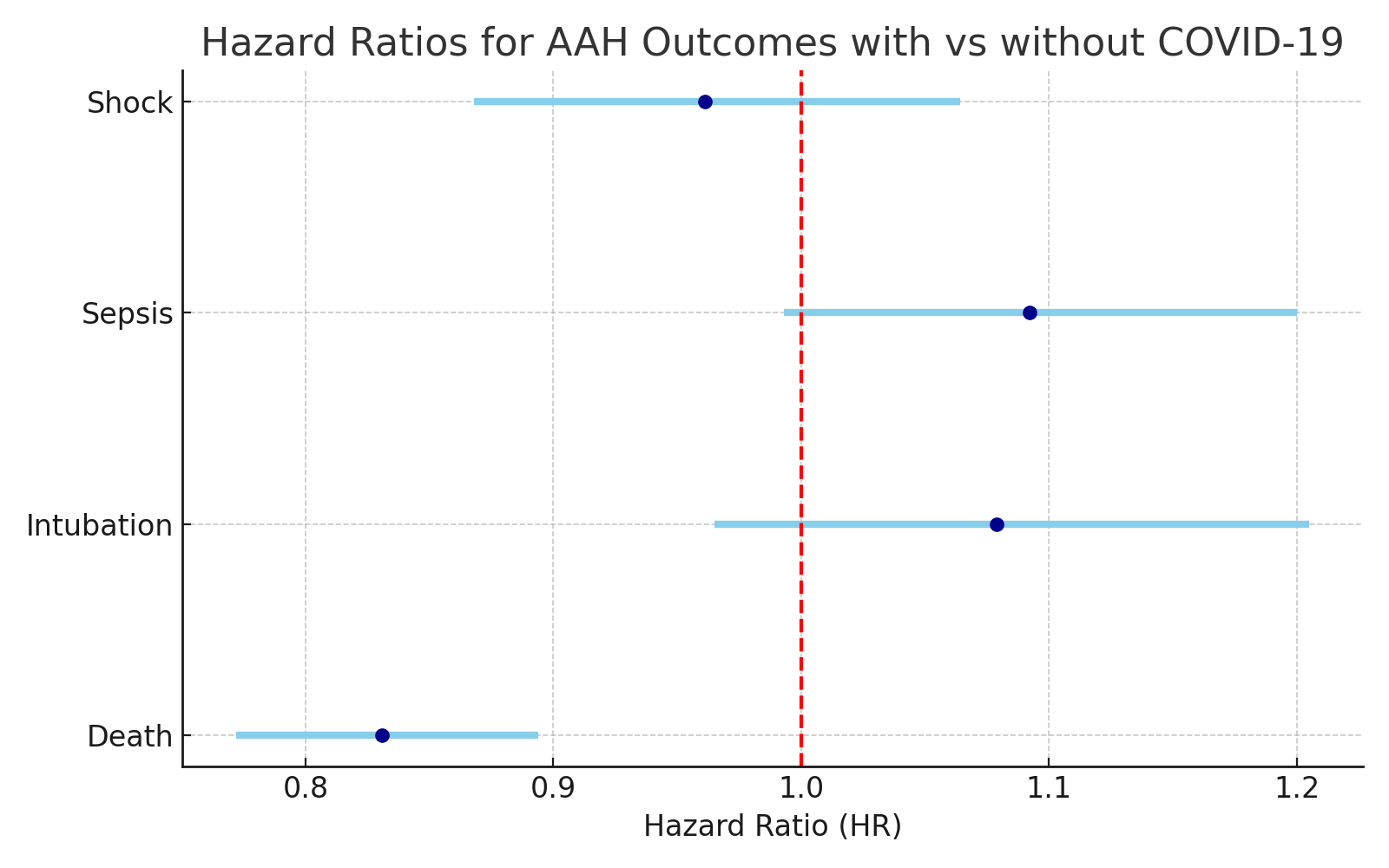
Figure: Figure 1: Hazard ratios for AAH outcomes with and without COVID-19
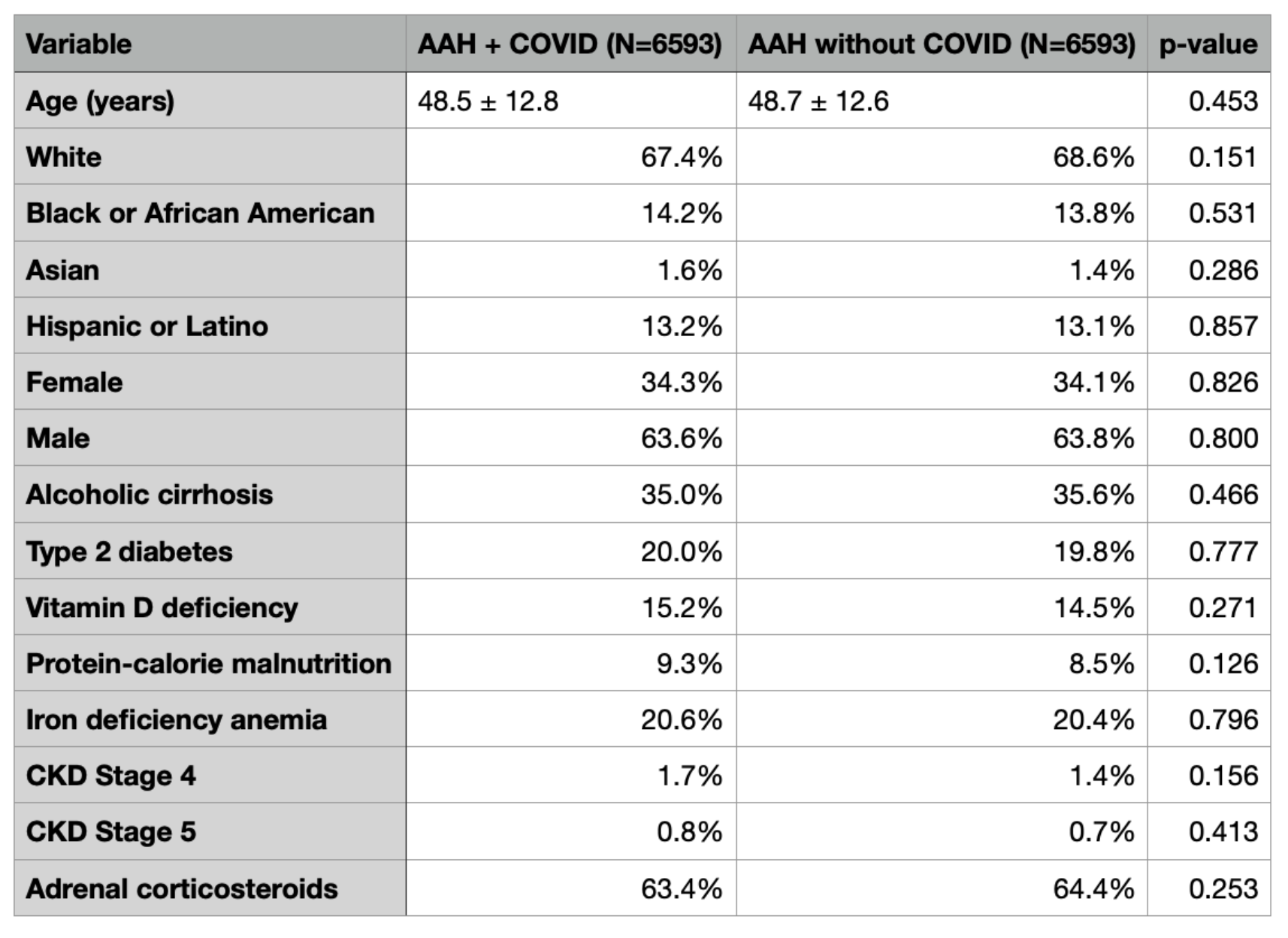
Figure: Table 1: Patient demographics and baseline characterstics after propensity score matching
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Miguel Salazar indicated no relevant financial relationships.
Khaled Al Smadi indicated no relevant financial relationships.
Zeid Kayali indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Miguel Salazar, MD2, Khaled Al Smadi, MD3, Zeid Kayali, MD, MBA4. P3664 - Impact of COVID-19 on Outcomes in Patients With Acute Alcoholic Hepatitis: A Propensity-Matched Analysis Using a National Federated Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
