Monday Poster Session
Category: Liver
P3662 - Predictors, Prevalence, and Impact of Aspiration Pneumonia in Hospitalized Patients With Hepatic Encephalopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmet Sakiri, MD
Mercyhealth Internal Medicine Residency
Rockford, IL
Presenting Author(s)
Ahmet Sakiri, MD1, Mohammed Zaman, DO2, Fahad Sarvari, MD3, Abu Fahad Abbasi, MD4, Mubeen Khan Mohammed Abdul, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Thayer Hamoudah, MD5, Naser Khan, MD5, Altaf Dawood, MD5, Baseer Qazi, MD5
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercyhealth Rockford, Rockford, IL; 3Mercyhealth, Rockford, IL; 4Mercyhealth Gastroenterology Fellowship, Rockford, IL; 5Mercyhealth Gastroenterology, Rockford, IL
Introduction: Hepatic encephalopathy (HE) is a neuropsychiatric syndrome arising from liver dysfunction. Aspiration pneumonia (AP) is a serious complication in these high-risk patients. HE and AP share a bidirectional relationship: severe HE increases aspiration risk, while AP-induced inflammation worsens hyperammonemia and accelerates HE progression. Current AASLD and AGA guidelines highlight early airway protection and infection control as key strategies to prevent AP and reduce HE recurrence. Despite its clinical significance, the predictors, prevalence, and outcomes of AP in hospitalized HE patients remain underexplored in large NIS cohorts.
Methods: We used 2019–2021 National Inpatient Sample data to identify adult hepatic encephalopathy admissions and assess AP outcomes using adjusted multivariable logistic and linear regressions. Significance was set at p< 0.05.
Results: Among ~500,000 weighted HE hospitalizations, AP prevalence was 4.7–5.0%. Men had higher AP rates than women (5.4% vs. 3.9%; p< 0.001). Medicaid (5.2%) and no-charge (6.2%) patients showed higher prevalence (p=0.0013). Urban and teaching hospitals had higher AP rates (p=0.0008), with the Northeast and West regions showing the highest (p< 0.001). In regression models, mechanical ventilation (OR 7.62), septic shock (OR 2.26), hepatic coma (OR 1.78), and malnutrition (OR 1.51) were the strongest predictors of AP (p< 0.001). Dialysis (OR 0.90), ascites (OR 0.83), and spontaneous bacterial peritonitis (OR 0.62) were associated with reduced AP odds. AP was associated with lower adjusted mortality (aOR 0.885; p=0.009) but significantly increased hospital charges (~33% increase; p< 0.001) and LOS (~39% increase; p< 0.001).
Discussion: We highlighted key clinical factors that put hospitalized HE patients at high risk for AP. Acute illness severity —especially the need for mechanical ventilation, presence of septic shock, and altered mental status — stood out as the main driver of risk, with malnutrition and overall comorbidity also contributing. We also found striking differences across patient groups and regions, reflecting real-world variation in how care is delivered. These insights highlight clear priorities: identify high-risk HE patients early, implement simple but effective preventive steps (like head-of-bed elevation, oral care, and swallow precautions). This study provides a foundation to improve outcomes and guide future quality initiatives in this population.
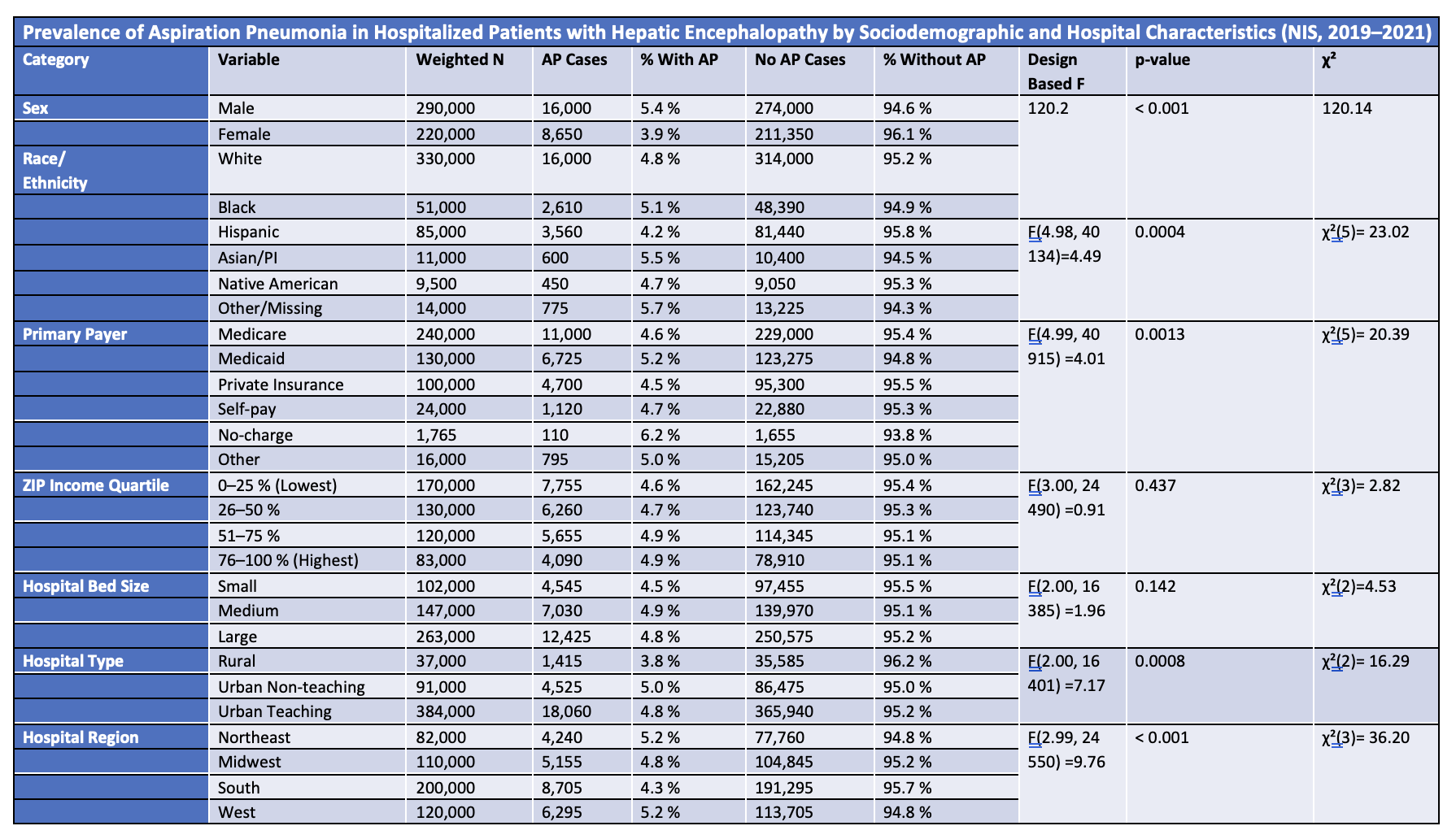
Figure: Weighted national estimates of aspiration pneumonia (AP) prevalence among hospitalized adults diagnosed with hepatic encephalopathy, stratified by demographic factors, insurance status, socioeconomic status, and hospital characteristics. Significance testing included survey-weighted design-based F statistics and chi-square tests, with statistically significant differences noted across sex, race/ethnicity, primary payer, hospital type, and region.
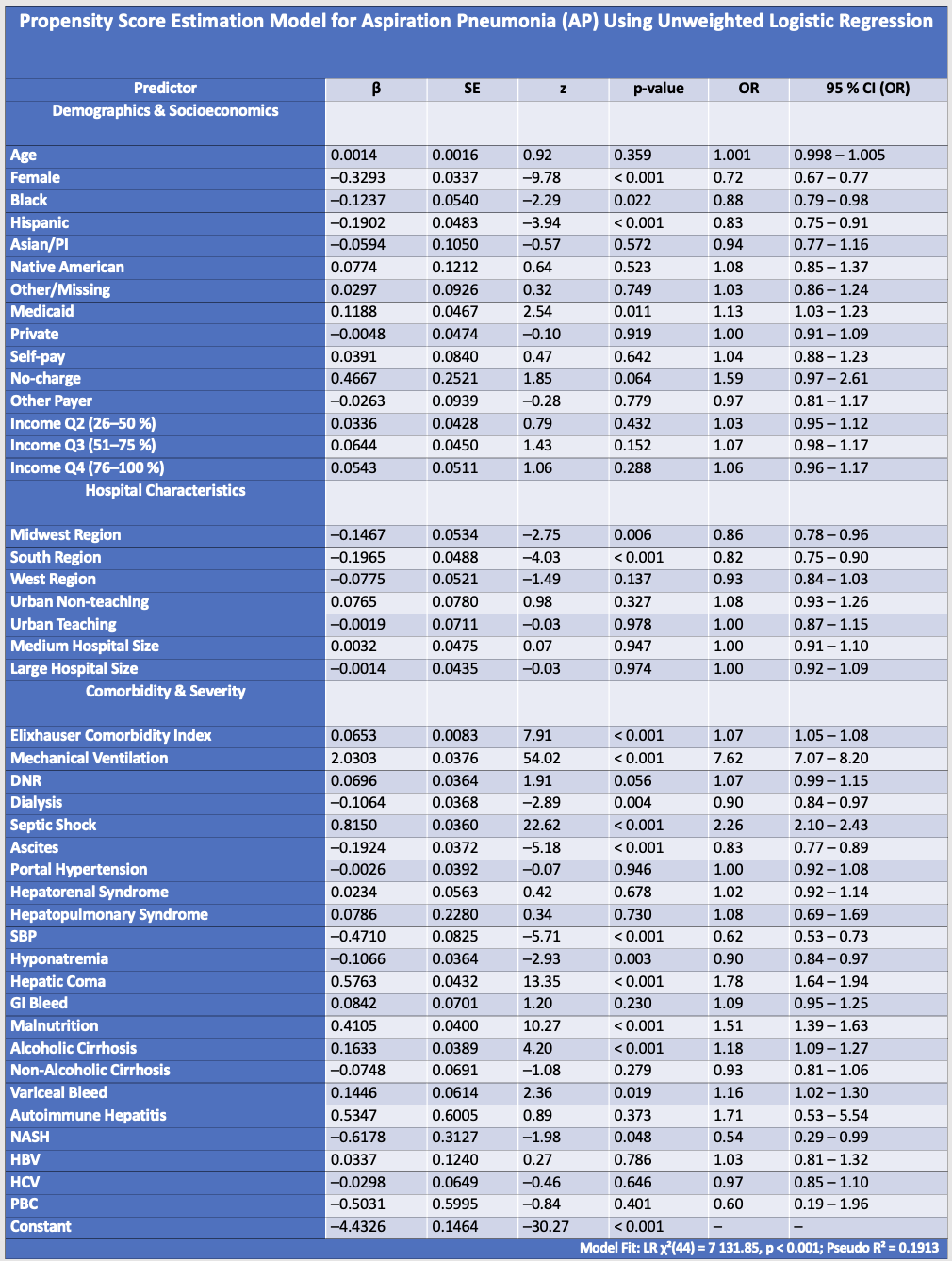
Figure: This unweighted logistic regression model estimates the likelihood of aspiration pneumonia (AP) in hospitalized patients and is used to generate propensity scores. The model includes demographic characteristics, socioeconomic status, hospital features, comorbidity burden, and hepatic/renal complications. Odds ratios (OR) are calculated as exp(β), where β is the regression coefficient from the logistic model.
Disclosures:
Ahmet Sakiri indicated no relevant financial relationships.
Mohammed Zaman indicated no relevant financial relationships.
Fahad Sarvari indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Mubeen Khan Mohammed Abdul indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Ahmet Sakiri, MD1, Mohammed Zaman, DO2, Fahad Sarvari, MD3, Abu Fahad Abbasi, MD4, Mubeen Khan Mohammed Abdul, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Thayer Hamoudah, MD5, Naser Khan, MD5, Altaf Dawood, MD5, Baseer Qazi, MD5. P3662 - Predictors, Prevalence, and Impact of Aspiration Pneumonia in Hospitalized Patients With Hepatic Encephalopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercyhealth Rockford, Rockford, IL; 3Mercyhealth, Rockford, IL; 4Mercyhealth Gastroenterology Fellowship, Rockford, IL; 5Mercyhealth Gastroenterology, Rockford, IL
Introduction: Hepatic encephalopathy (HE) is a neuropsychiatric syndrome arising from liver dysfunction. Aspiration pneumonia (AP) is a serious complication in these high-risk patients. HE and AP share a bidirectional relationship: severe HE increases aspiration risk, while AP-induced inflammation worsens hyperammonemia and accelerates HE progression. Current AASLD and AGA guidelines highlight early airway protection and infection control as key strategies to prevent AP and reduce HE recurrence. Despite its clinical significance, the predictors, prevalence, and outcomes of AP in hospitalized HE patients remain underexplored in large NIS cohorts.
Methods: We used 2019–2021 National Inpatient Sample data to identify adult hepatic encephalopathy admissions and assess AP outcomes using adjusted multivariable logistic and linear regressions. Significance was set at p< 0.05.
Results: Among ~500,000 weighted HE hospitalizations, AP prevalence was 4.7–5.0%. Men had higher AP rates than women (5.4% vs. 3.9%; p< 0.001). Medicaid (5.2%) and no-charge (6.2%) patients showed higher prevalence (p=0.0013). Urban and teaching hospitals had higher AP rates (p=0.0008), with the Northeast and West regions showing the highest (p< 0.001). In regression models, mechanical ventilation (OR 7.62), septic shock (OR 2.26), hepatic coma (OR 1.78), and malnutrition (OR 1.51) were the strongest predictors of AP (p< 0.001). Dialysis (OR 0.90), ascites (OR 0.83), and spontaneous bacterial peritonitis (OR 0.62) were associated with reduced AP odds. AP was associated with lower adjusted mortality (aOR 0.885; p=0.009) but significantly increased hospital charges (~33% increase; p< 0.001) and LOS (~39% increase; p< 0.001).
Discussion: We highlighted key clinical factors that put hospitalized HE patients at high risk for AP. Acute illness severity —especially the need for mechanical ventilation, presence of septic shock, and altered mental status — stood out as the main driver of risk, with malnutrition and overall comorbidity also contributing. We also found striking differences across patient groups and regions, reflecting real-world variation in how care is delivered. These insights highlight clear priorities: identify high-risk HE patients early, implement simple but effective preventive steps (like head-of-bed elevation, oral care, and swallow precautions). This study provides a foundation to improve outcomes and guide future quality initiatives in this population.
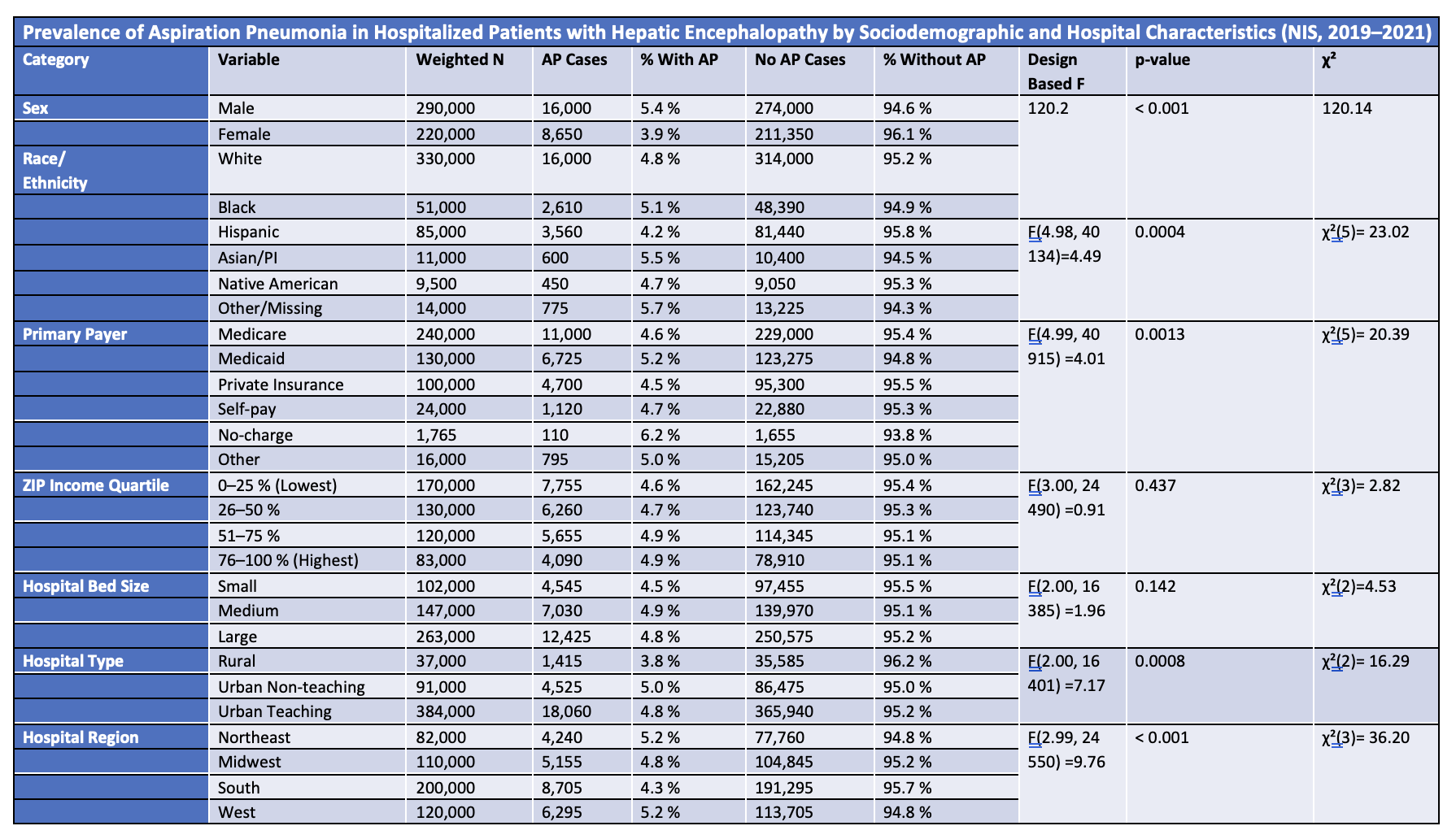
Figure: Weighted national estimates of aspiration pneumonia (AP) prevalence among hospitalized adults diagnosed with hepatic encephalopathy, stratified by demographic factors, insurance status, socioeconomic status, and hospital characteristics. Significance testing included survey-weighted design-based F statistics and chi-square tests, with statistically significant differences noted across sex, race/ethnicity, primary payer, hospital type, and region.
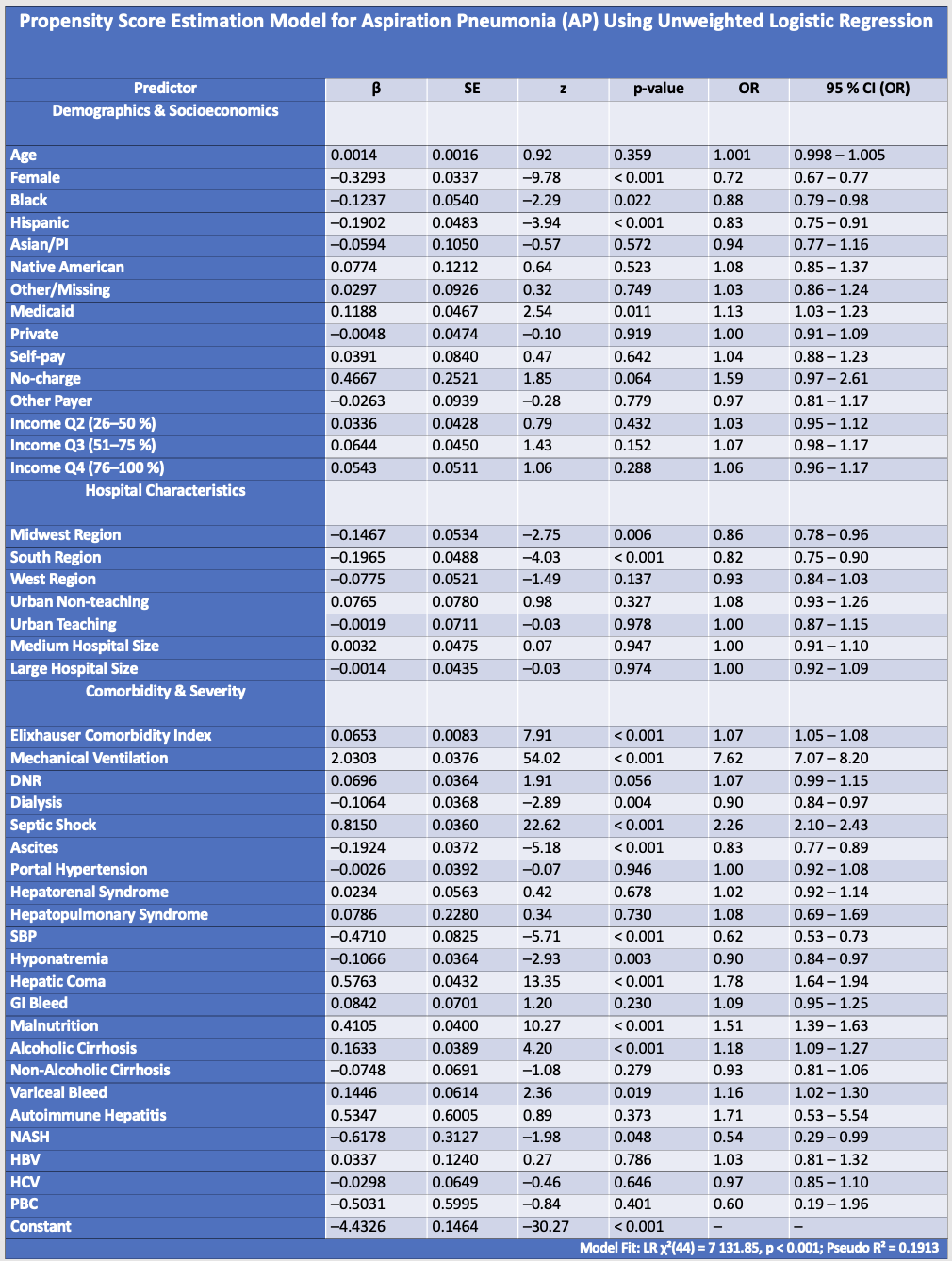
Figure: This unweighted logistic regression model estimates the likelihood of aspiration pneumonia (AP) in hospitalized patients and is used to generate propensity scores. The model includes demographic characteristics, socioeconomic status, hospital features, comorbidity burden, and hepatic/renal complications. Odds ratios (OR) are calculated as exp(β), where β is the regression coefficient from the logistic model.
Disclosures:
Ahmet Sakiri indicated no relevant financial relationships.
Mohammed Zaman indicated no relevant financial relationships.
Fahad Sarvari indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Mubeen Khan Mohammed Abdul indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Ahmet Sakiri, MD1, Mohammed Zaman, DO2, Fahad Sarvari, MD3, Abu Fahad Abbasi, MD4, Mubeen Khan Mohammed Abdul, MD3, Luqman Baloch, MD3, Ammar Aqeel, MD3, Thayer Hamoudah, MD5, Naser Khan, MD5, Altaf Dawood, MD5, Baseer Qazi, MD5. P3662 - Predictors, Prevalence, and Impact of Aspiration Pneumonia in Hospitalized Patients With Hepatic Encephalopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
