Monday Poster Session
Category: Liver
P3658 - Association of Vitamin D Supplementation in the Development of Osteoporosis and Osteoporosis-Related Fractures in Primary Biliary Cholangitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Leandro Sierra, MD (he/him/his)
Department of Internal Medicine, Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4Cleveland Clinic Florida, Weston, FL; 5Cleveland Clinic Foundation, Hoover, AL; 6Cleveland Clinic, Cleveland, OH
Introduction: Vitamin D supplementation is recommended for osteoporosis with chronic liver disease, targeting calcium homeostasis and bone mineralization. Despite widespread use of Vitamin D supplementation, its clinical efficacy in osteoporosis progression and development of fractures has not been rigorously evaluated in PBC population.
Methods: We conducted a retrospective cohort study using data from two U.S.-based tertiary centers from 2005–2025. Participants included postmenopausal women aged >65 years with primary biliary cholangitis (PBC) and age- and baseline serum vitamin D level-matched controls. All participants maintained consistent vitamin D supplementation (800–1000 IU/day) for ≥1 year. Fracture incidence was ascertained via comprehensive medical record review. Risk factors for fractures were evaluated using univariate and multivariate logistic regression analyses, while longitudinal fracture outcomes were modeled with mixed-effects regression modelling.
Results: Among 101 PBC and 208 matched-control patients receiving vitamin D supplementation, PBC patients demonstrated lower mean T-scores (-1.98 vs. -1.63; p=0.05) and lumbar mineral density scores (0.99 vs. 1.07; p=0.01) despite comparable osteopenia and osteoporosis prevalence. Fracture prevalence was higher in PBC compared to controls (56.0% vs. 36.1%), with significantly increased risk of multiple fractures (OR=1.29, p< 0.001). Osteoporosis medication reduced fracture risk (OR=0.80, p=0.05). Mixed-effects models revealed diverging 10-year trajectories with only marginal risk reduction in PBC patients from 75% to 62% while substantial risk reduction from 59% to 24% in controls.
Discussion: Standard vitamin D supplementation may not adequately protect PBC patients from fractures, as evidenced by persistently elevated rates and marginal long-term risk reduction. However, in combination with osteoporosis medications, Vitamin D supplementation partially reduced risk of osteoporosis-related fractures. Further studies are needed to identify risk factors of metabolic bone disease progression and fracture development in PBC to individualize prevention and treatment approach in this population.
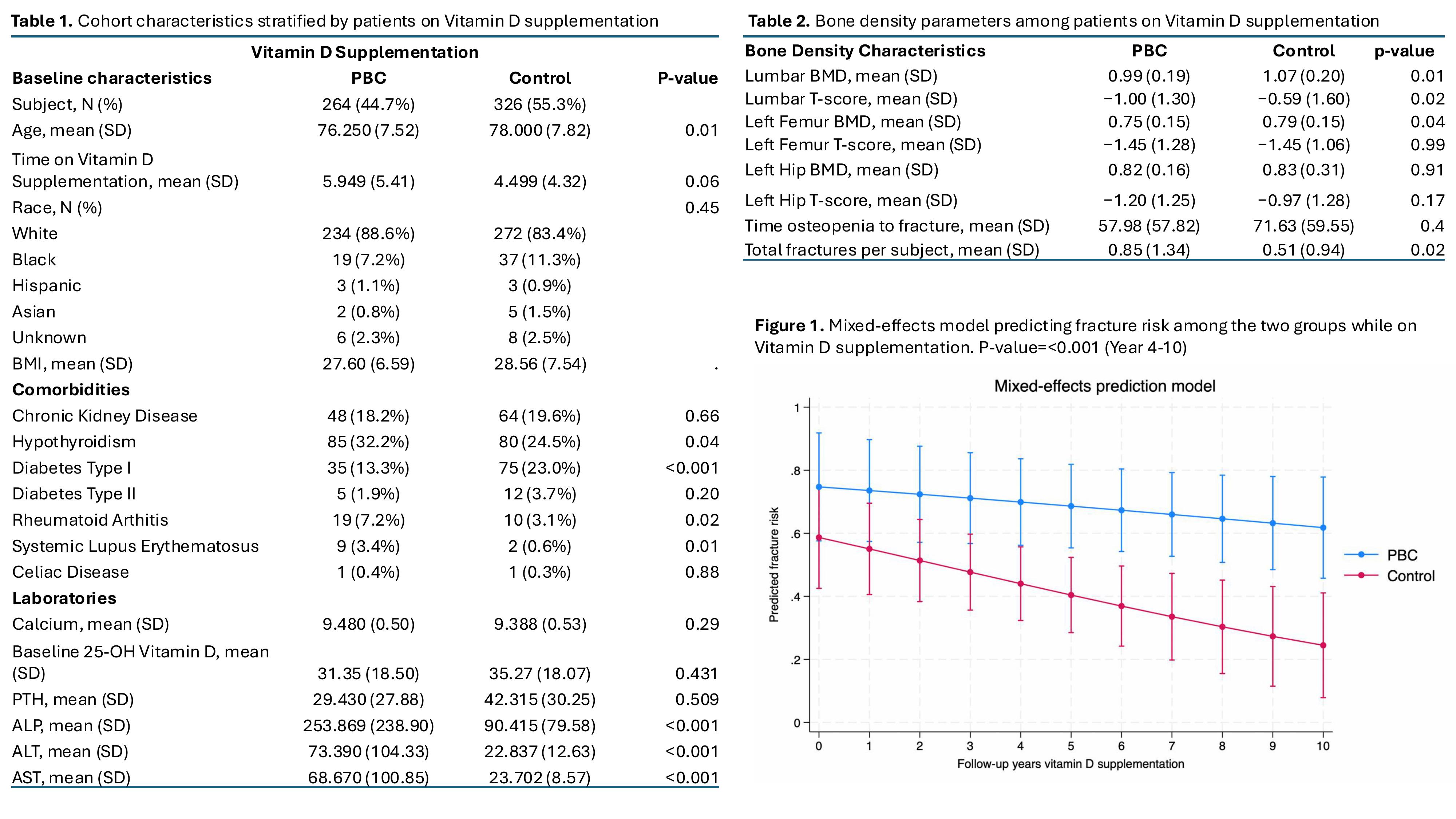
Figure: Figure: Clinical characteristics, bone density parameters, and predicted fracture risk among patients on Vitamin D supplementation.
(Table 1) Baseline demographics and comorbidities by group (PBC vs. Control).
(Table 2) Bone density metrics among those on Vitamin D.
(Figure 1) Mixed-effects model shows significantly lower predicted fracture risk in PBC group over 10 years (p < 0.001 from year 4 onward).
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Hussam Kawas indicated no relevant financial relationships.
Rachel McNulty indicated no relevant financial relationships.
Sara Valencia indicated no relevant financial relationships.
Juan Armijos indicated no relevant financial relationships.
Xaralambos Zervos indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6. P3658 - Association of Vitamin D Supplementation in the Development of Osteoporosis and Osteoporosis-Related Fractures in Primary Biliary Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4Cleveland Clinic Florida, Weston, FL; 5Cleveland Clinic Foundation, Hoover, AL; 6Cleveland Clinic, Cleveland, OH
Introduction: Vitamin D supplementation is recommended for osteoporosis with chronic liver disease, targeting calcium homeostasis and bone mineralization. Despite widespread use of Vitamin D supplementation, its clinical efficacy in osteoporosis progression and development of fractures has not been rigorously evaluated in PBC population.
Methods: We conducted a retrospective cohort study using data from two U.S.-based tertiary centers from 2005–2025. Participants included postmenopausal women aged >65 years with primary biliary cholangitis (PBC) and age- and baseline serum vitamin D level-matched controls. All participants maintained consistent vitamin D supplementation (800–1000 IU/day) for ≥1 year. Fracture incidence was ascertained via comprehensive medical record review. Risk factors for fractures were evaluated using univariate and multivariate logistic regression analyses, while longitudinal fracture outcomes were modeled with mixed-effects regression modelling.
Results: Among 101 PBC and 208 matched-control patients receiving vitamin D supplementation, PBC patients demonstrated lower mean T-scores (-1.98 vs. -1.63; p=0.05) and lumbar mineral density scores (0.99 vs. 1.07; p=0.01) despite comparable osteopenia and osteoporosis prevalence. Fracture prevalence was higher in PBC compared to controls (56.0% vs. 36.1%), with significantly increased risk of multiple fractures (OR=1.29, p< 0.001). Osteoporosis medication reduced fracture risk (OR=0.80, p=0.05). Mixed-effects models revealed diverging 10-year trajectories with only marginal risk reduction in PBC patients from 75% to 62% while substantial risk reduction from 59% to 24% in controls.
Discussion: Standard vitamin D supplementation may not adequately protect PBC patients from fractures, as evidenced by persistently elevated rates and marginal long-term risk reduction. However, in combination with osteoporosis medications, Vitamin D supplementation partially reduced risk of osteoporosis-related fractures. Further studies are needed to identify risk factors of metabolic bone disease progression and fracture development in PBC to individualize prevention and treatment approach in this population.
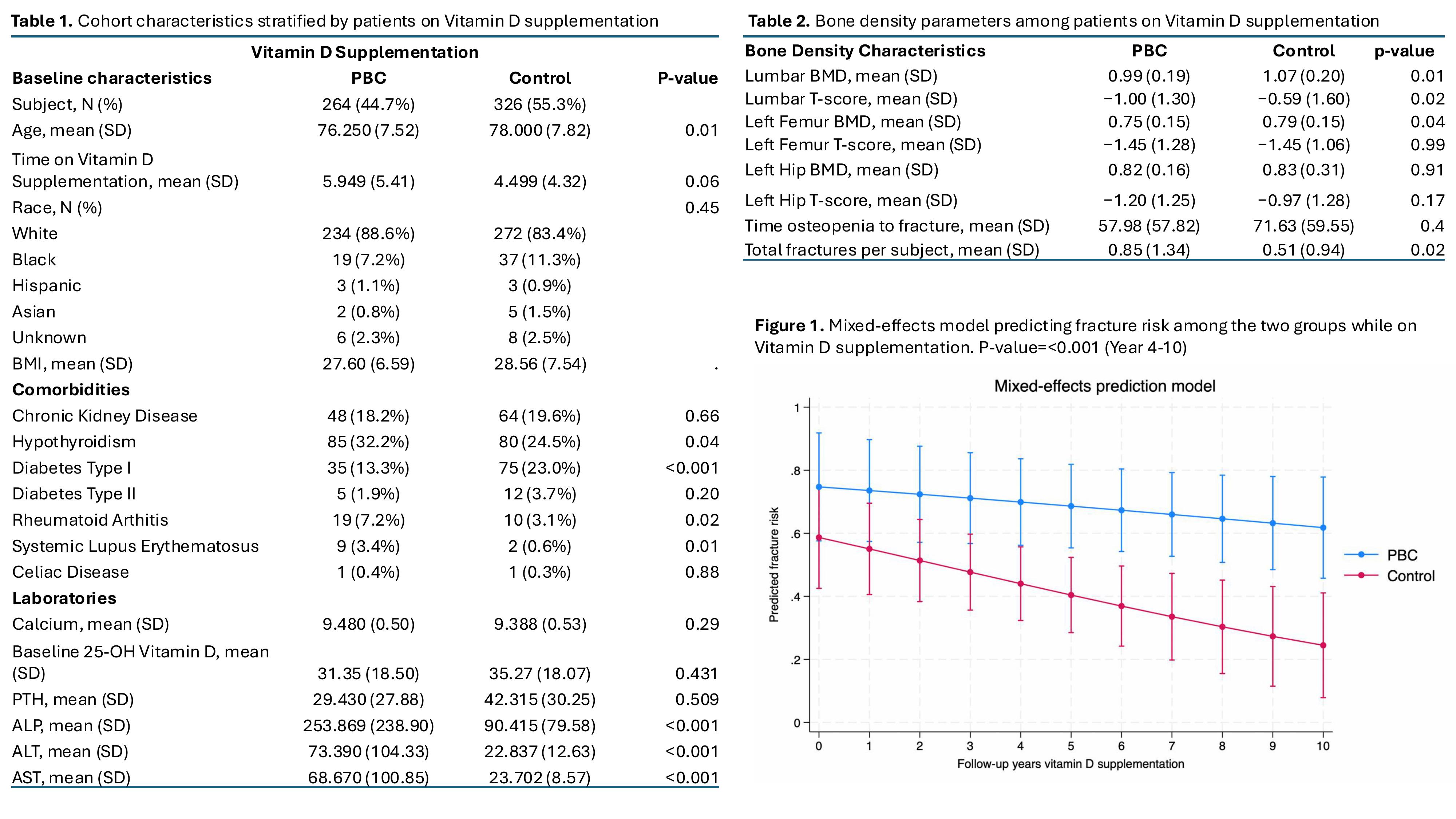
Figure: Figure: Clinical characteristics, bone density parameters, and predicted fracture risk among patients on Vitamin D supplementation.
(Table 1) Baseline demographics and comorbidities by group (PBC vs. Control).
(Table 2) Bone density metrics among those on Vitamin D.
(Figure 1) Mixed-effects model shows significantly lower predicted fracture risk in PBC group over 10 years (p < 0.001 from year 4 onward).
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Hussam Kawas indicated no relevant financial relationships.
Rachel McNulty indicated no relevant financial relationships.
Sara Valencia indicated no relevant financial relationships.
Juan Armijos indicated no relevant financial relationships.
Xaralambos Zervos indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6. P3658 - Association of Vitamin D Supplementation in the Development of Osteoporosis and Osteoporosis-Related Fractures in Primary Biliary Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
