Monday Poster Session
Category: Liver
P3624 - Validation of NAFLD ICD Codes to Identify MASLD in a High-Risk Hispanic Population
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manuela Araque, MD, MPH
University of Miami/Jackson Medical Hospital
Miami, FL
Presenting Author(s)
Manuela Araque, MD, MPH1, Tyhanna Hibbert, MS2, Anthony Quiej, BA2, Cathy Zheng, MD2, Stephanie Garces, MSPH, CPH2, Yvonne N.. Flores, PhD, MPH3, Patricia D. Jones, MD, MSCR2
1University of Miami/Jackson Medical Hospital, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD), a common cause of chronic liver disease, can progress to cirrhosis and hepatocellular carcinoma. Through consensus, nonalcoholic fatty liver disease (NAFLD) was renamed MASLD. Given distinct case definitions, overlap between these diagnoses is variable. The global prevalence of MASLD is 30%, however risk is highest in Hispanics. This study aims to characterize the validity of historical ICD codes for NAFLD for MASLD diagnosis within a high-risk Hispanic patient population.
Methods: Using research informatics, we identified Hispanic adults with ICD-9 codes 571.8/571.9 and ICD-10 codes K76.0 and K75.81 without codes for alcohol use disorder or other chronic liver diseases seen from 7/2024-12/2024 (Figure 1). We reviewed the electronic medical records (EMR) of the subset of patients seen within the Gastroenterology or Hepatology clinics (GI/Hep). We characterize the proportion of patients with MASLD, metabolic dysfunction and alcohol-related liver disease (MetALD), or other liver diseases.
Results: There were 7,183 patients with relevant ICD-9/10 codes for NAFLD, of whom 4,688 were of Hispanic, 65.3%. Only 33.2%, n = 1,558, were seen by GI/Hep. Within that group, the median age was 58 years and 62% were females. According to race listed in the EMR, the sample was 95.3% White, 2% Multiracial, 1.8% Black, and 0.9% Other. Our Hispanic population is diverse, representing 35 countries of origin; 21.4% were US-born and 53% have limited English proficiency. Of these 1,558 patients identified using codes for NAFLD, 1,511 (97%) had fatty liver present. Only 1,246 (80%) met diagnostic criteria for MASLD, 98 (6.3%) met criteria for MetALD , and 16 (1%) met criteria for ALD. There were 198 patients who did not meet criteria for MASLD because they had other concurrent liver diseases (151, 10%) or no evidence of steatosis (47, 3%).
Discussion: Previous reports have suggested high concordance of NAFLD and MASLD, ranging from 95-99%. We found high rates of steatosis, but expected higher concordance between NAFLD and MASLD, given that these patients were seen in subspecialty clinics and the Hispanic population has higher risk. Our results highlight the risk of diagnostic misclassification when using administrative data alone for case-finding and the need for prospective validation of MASLD diagnostic codes using novel diagnostic criteria.
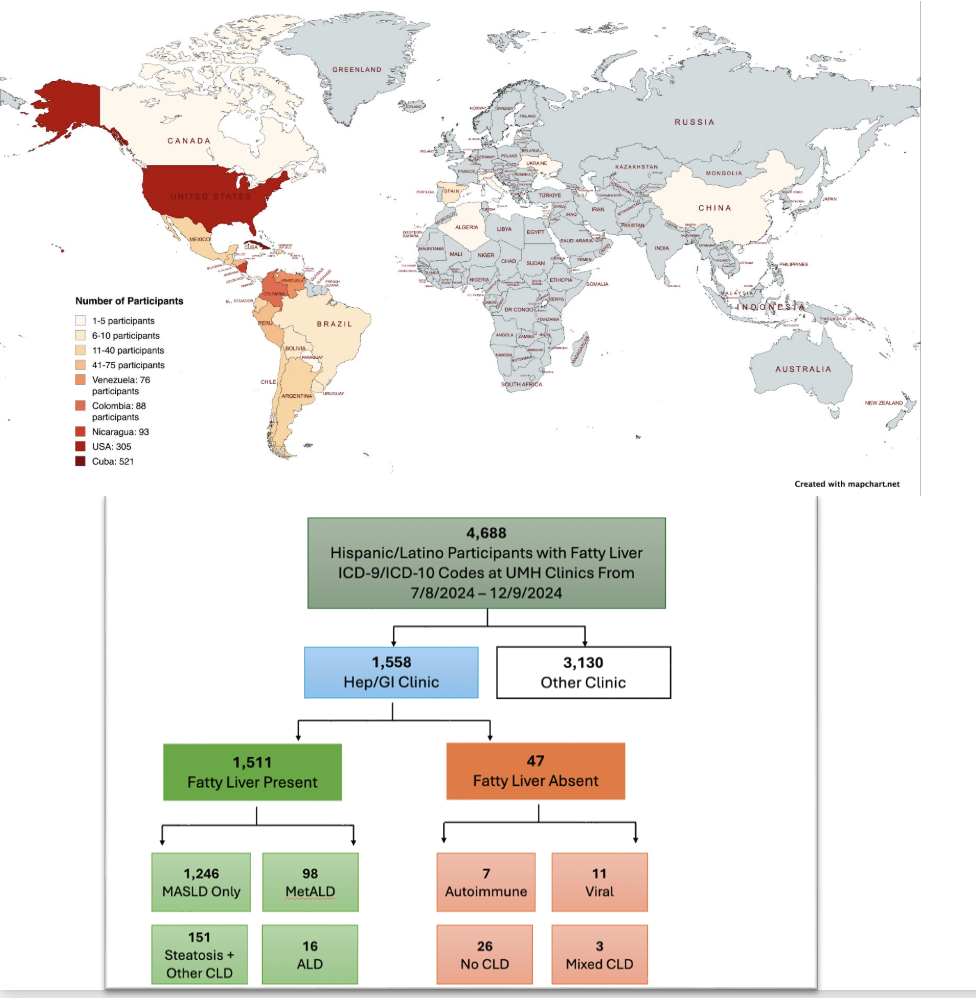
Figure: Figure 1A: Map of Participants Country of Origin and Figure 1B: Flow Chart of Validation of NAFLD ICD Codes
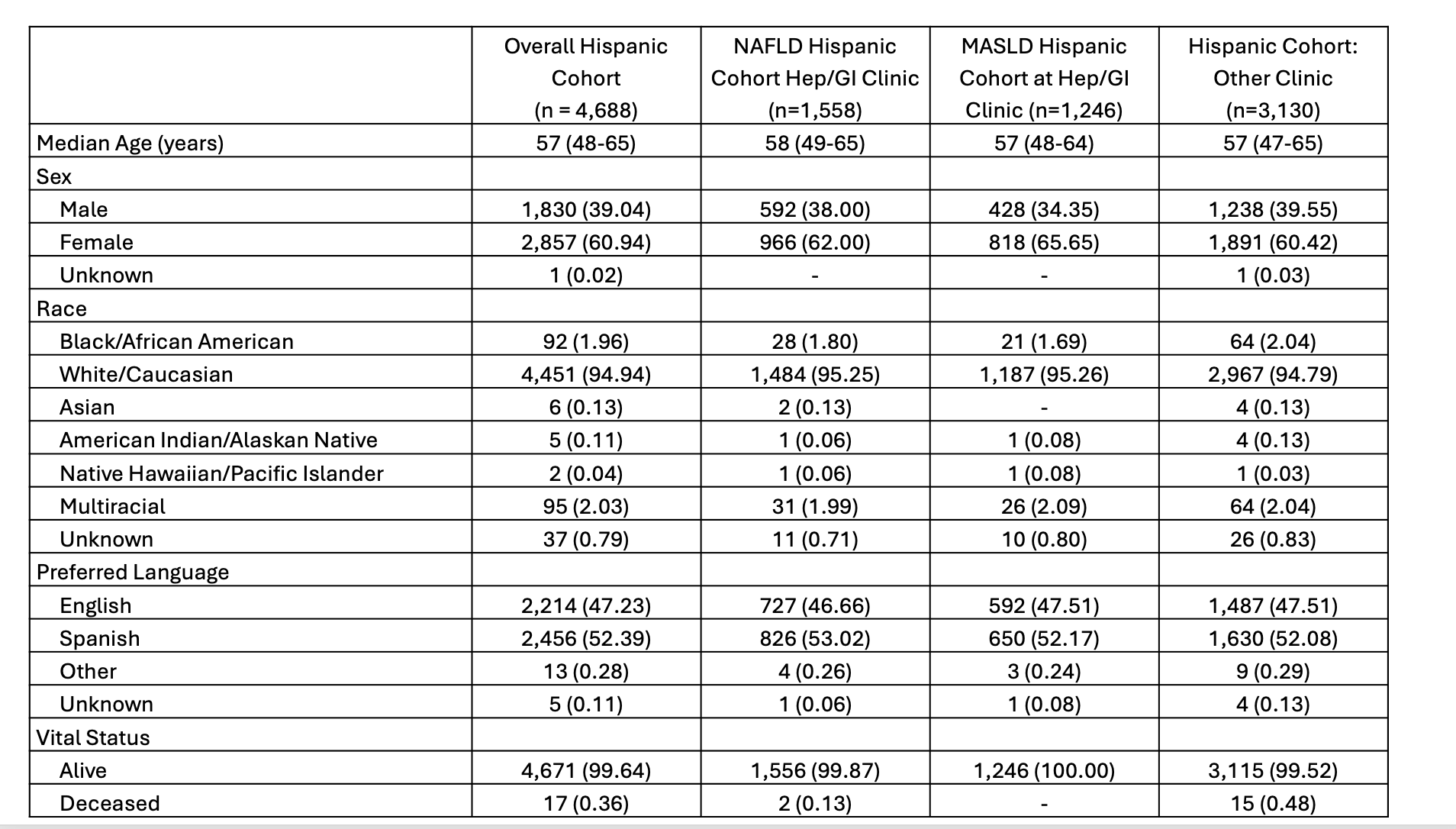
Figure: Table 1: Demographic Characteristics
Disclosures:
Manuela Araque indicated no relevant financial relationships.
Tyhanna Hibbert indicated no relevant financial relationships.
Anthony Quiej indicated no relevant financial relationships.
Cathy Zheng indicated no relevant financial relationships.
Stephanie Garces indicated no relevant financial relationships.
Yvonne Flores indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Manuela Araque, MD, MPH1, Tyhanna Hibbert, MS2, Anthony Quiej, BA2, Cathy Zheng, MD2, Stephanie Garces, MSPH, CPH2, Yvonne N.. Flores, PhD, MPH3, Patricia D. Jones, MD, MSCR2. P3624 - Validation of NAFLD ICD Codes to Identify MASLD in a High-Risk Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami/Jackson Medical Hospital, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD), a common cause of chronic liver disease, can progress to cirrhosis and hepatocellular carcinoma. Through consensus, nonalcoholic fatty liver disease (NAFLD) was renamed MASLD. Given distinct case definitions, overlap between these diagnoses is variable. The global prevalence of MASLD is 30%, however risk is highest in Hispanics. This study aims to characterize the validity of historical ICD codes for NAFLD for MASLD diagnosis within a high-risk Hispanic patient population.
Methods: Using research informatics, we identified Hispanic adults with ICD-9 codes 571.8/571.9 and ICD-10 codes K76.0 and K75.81 without codes for alcohol use disorder or other chronic liver diseases seen from 7/2024-12/2024 (Figure 1). We reviewed the electronic medical records (EMR) of the subset of patients seen within the Gastroenterology or Hepatology clinics (GI/Hep). We characterize the proportion of patients with MASLD, metabolic dysfunction and alcohol-related liver disease (MetALD), or other liver diseases.
Results: There were 7,183 patients with relevant ICD-9/10 codes for NAFLD, of whom 4,688 were of Hispanic, 65.3%. Only 33.2%, n = 1,558, were seen by GI/Hep. Within that group, the median age was 58 years and 62% were females. According to race listed in the EMR, the sample was 95.3% White, 2% Multiracial, 1.8% Black, and 0.9% Other. Our Hispanic population is diverse, representing 35 countries of origin; 21.4% were US-born and 53% have limited English proficiency. Of these 1,558 patients identified using codes for NAFLD, 1,511 (97%) had fatty liver present. Only 1,246 (80%) met diagnostic criteria for MASLD, 98 (6.3%) met criteria for MetALD , and 16 (1%) met criteria for ALD. There were 198 patients who did not meet criteria for MASLD because they had other concurrent liver diseases (151, 10%) or no evidence of steatosis (47, 3%).
Discussion: Previous reports have suggested high concordance of NAFLD and MASLD, ranging from 95-99%. We found high rates of steatosis, but expected higher concordance between NAFLD and MASLD, given that these patients were seen in subspecialty clinics and the Hispanic population has higher risk. Our results highlight the risk of diagnostic misclassification when using administrative data alone for case-finding and the need for prospective validation of MASLD diagnostic codes using novel diagnostic criteria.
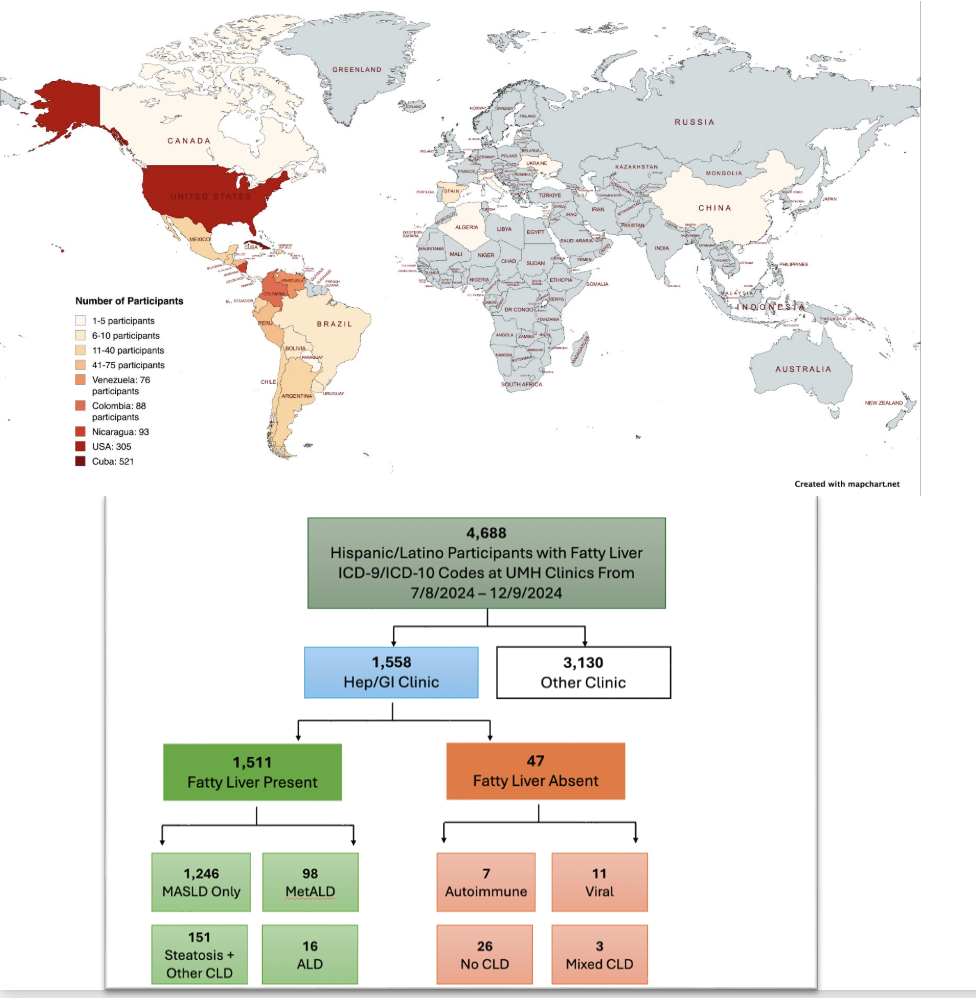
Figure: Figure 1A: Map of Participants Country of Origin and Figure 1B: Flow Chart of Validation of NAFLD ICD Codes
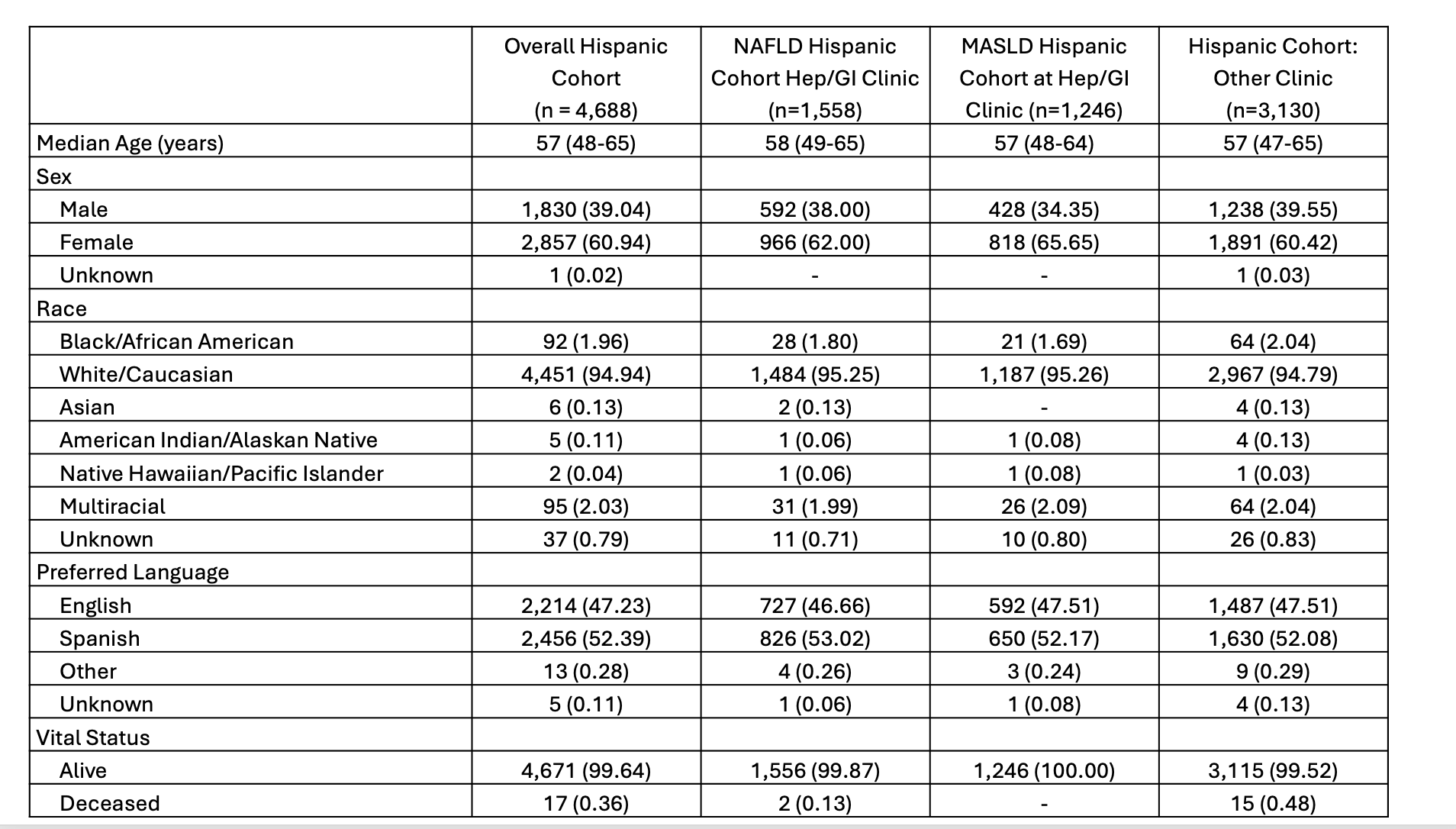
Figure: Table 1: Demographic Characteristics
Disclosures:
Manuela Araque indicated no relevant financial relationships.
Tyhanna Hibbert indicated no relevant financial relationships.
Anthony Quiej indicated no relevant financial relationships.
Cathy Zheng indicated no relevant financial relationships.
Stephanie Garces indicated no relevant financial relationships.
Yvonne Flores indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Manuela Araque, MD, MPH1, Tyhanna Hibbert, MS2, Anthony Quiej, BA2, Cathy Zheng, MD2, Stephanie Garces, MSPH, CPH2, Yvonne N.. Flores, PhD, MPH3, Patricia D. Jones, MD, MSCR2. P3624 - Validation of NAFLD ICD Codes to Identify MASLD in a High-Risk Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

