Monday Poster Session
Category: Liver
P3623 - Burden and Impact of Infections in Patients Undergoing Liver Transplant: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rahul Chikatimalla, MBBS
Kamineni Institute of Medical Sciences
Narketpalle, Telangana, India
Presenting Author(s)
Rahul Chikatimalla, MBBS1, Carol Singh, MBBS2, Vishnu Yanamaladoddi, MD3, Mohammad Naseem, MBBS4, Nishma Dhand, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD3, Mohanad Al-Qaisi, MD3
1Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 2Dayanand Medical College and Hospital, New Jersey, NJ; 3Creighton University School of Medicine, Phoenix, AZ; 4Maulana Azad Medical College, New Delhi, Delhi, India; 5Dayanand Medical College and Hospital, Moga, Punjab, India; 6Creighton University Medical Center, Phoenix, AZ
Introduction: Infections are common among patients with cirrhosis and in patients requiring liver transplantation. Studies have reported them to delay liver transplantation, as active infections are considered a contraindication to liver transplant. The aim of the study was to examine the current burden, types, and impact of infections during index LT hospitalization using a large national cohort.
Methods: We analyzed data from the National Inpatient Sample (NIS) Database (2016-2022) to identify all adult patients who underwent liver transplantation. Patients were stratified into two groups based on the presence or absence of infections. Data collected included patient demographics, liver disease etiology, liver-related decompensations, comorbidities, and clinical outcomes. Outcomes assessed were in-hospital mortality, total complications, non-home discharges, and resource utilization. The multivariate logistic/linear regression analysis was used to determine the impact of infections on these outcomes.
Results: Among 50,630 liver transplant (LT) recipients, 15,130 (29.9%) developed infections during hospitalization. Most infected patients were aged 45–64 years (56.2%), male (56.9%), and White (66.6%). The most common infections observed were hospital-acquired pneumonia (HAP) (8.5%), urinary tract infections (UTI) (8.3%), and Clostridiodes difficile infection (8.1%). Infections were significantly associated with adverse clinical outcomes, including higher in-hospital mortality (4.2% vs. 2.2%), total complications (71.2% vs. 56.0%), and non-home discharges (67.5% vs. 51.9%). After adjusting for confounding factors, patients with infections had a higher odds of non-home discharges (aOR-1.64, 95% CI-1.47-1.82, p< 0.001), total complications (aOR-1.35, 95% CI-1.22-1.49, p< 0.001), a longer length of stay (adj. coefficient- 10.74 days, 95% CI: 9.56-11.9, p< 0.001) and higher total hospitalization charges (adj. Coefficient- $185,320.80, 95% CI: $151527.5- $219114.2, p< 0.001). No differences were noted in the mortality between the two groups (aOR-1.07, p-0.64)
Discussion: Infections during LT hospitalization occurred in nearly one-third of patients. The presence of infection was not associated with increased mortality, but was associated with higher morbidity and resource utilization. These findings underscore the high clinical and economic burden of post-transplant infections and highlight the need for targeted preventive strategies.
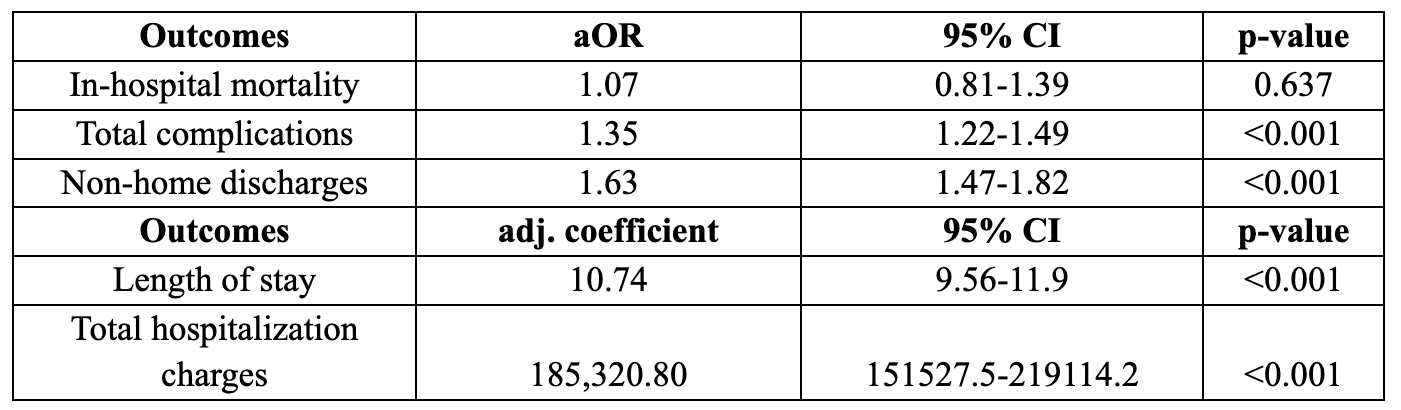
Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization
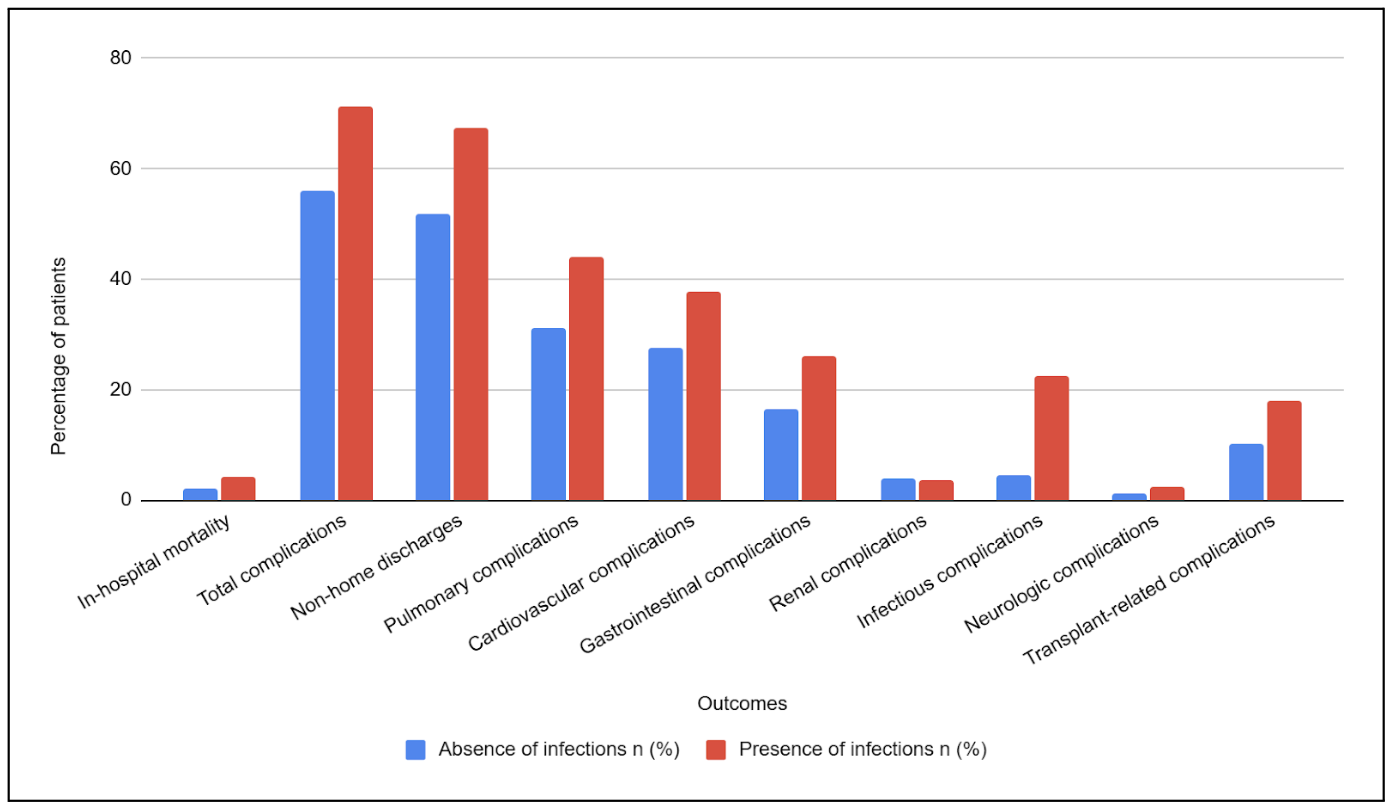
Figure: Figure 1. Bar chart comparing outcomes in patients undergoing LT stratified by the presence of infections
Disclosures:
Rahul Chikatimalla indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Mohammad Naseem indicated no relevant financial relationships.
Nishma Dhand indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Mohanad Al-Qaisi indicated no relevant financial relationships.
Rahul Chikatimalla, MBBS1, Carol Singh, MBBS2, Vishnu Yanamaladoddi, MD3, Mohammad Naseem, MBBS4, Nishma Dhand, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD3, Mohanad Al-Qaisi, MD3. P3623 - Burden and Impact of Infections in Patients Undergoing Liver Transplant: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 2Dayanand Medical College and Hospital, New Jersey, NJ; 3Creighton University School of Medicine, Phoenix, AZ; 4Maulana Azad Medical College, New Delhi, Delhi, India; 5Dayanand Medical College and Hospital, Moga, Punjab, India; 6Creighton University Medical Center, Phoenix, AZ
Introduction: Infections are common among patients with cirrhosis and in patients requiring liver transplantation. Studies have reported them to delay liver transplantation, as active infections are considered a contraindication to liver transplant. The aim of the study was to examine the current burden, types, and impact of infections during index LT hospitalization using a large national cohort.
Methods: We analyzed data from the National Inpatient Sample (NIS) Database (2016-2022) to identify all adult patients who underwent liver transplantation. Patients were stratified into two groups based on the presence or absence of infections. Data collected included patient demographics, liver disease etiology, liver-related decompensations, comorbidities, and clinical outcomes. Outcomes assessed were in-hospital mortality, total complications, non-home discharges, and resource utilization. The multivariate logistic/linear regression analysis was used to determine the impact of infections on these outcomes.
Results: Among 50,630 liver transplant (LT) recipients, 15,130 (29.9%) developed infections during hospitalization. Most infected patients were aged 45–64 years (56.2%), male (56.9%), and White (66.6%). The most common infections observed were hospital-acquired pneumonia (HAP) (8.5%), urinary tract infections (UTI) (8.3%), and Clostridiodes difficile infection (8.1%). Infections were significantly associated with adverse clinical outcomes, including higher in-hospital mortality (4.2% vs. 2.2%), total complications (71.2% vs. 56.0%), and non-home discharges (67.5% vs. 51.9%). After adjusting for confounding factors, patients with infections had a higher odds of non-home discharges (aOR-1.64, 95% CI-1.47-1.82, p< 0.001), total complications (aOR-1.35, 95% CI-1.22-1.49, p< 0.001), a longer length of stay (adj. coefficient- 10.74 days, 95% CI: 9.56-11.9, p< 0.001) and higher total hospitalization charges (adj. Coefficient- $185,320.80, 95% CI: $151527.5- $219114.2, p< 0.001). No differences were noted in the mortality between the two groups (aOR-1.07, p-0.64)
Discussion: Infections during LT hospitalization occurred in nearly one-third of patients. The presence of infection was not associated with increased mortality, but was associated with higher morbidity and resource utilization. These findings underscore the high clinical and economic burden of post-transplant infections and highlight the need for targeted preventive strategies.
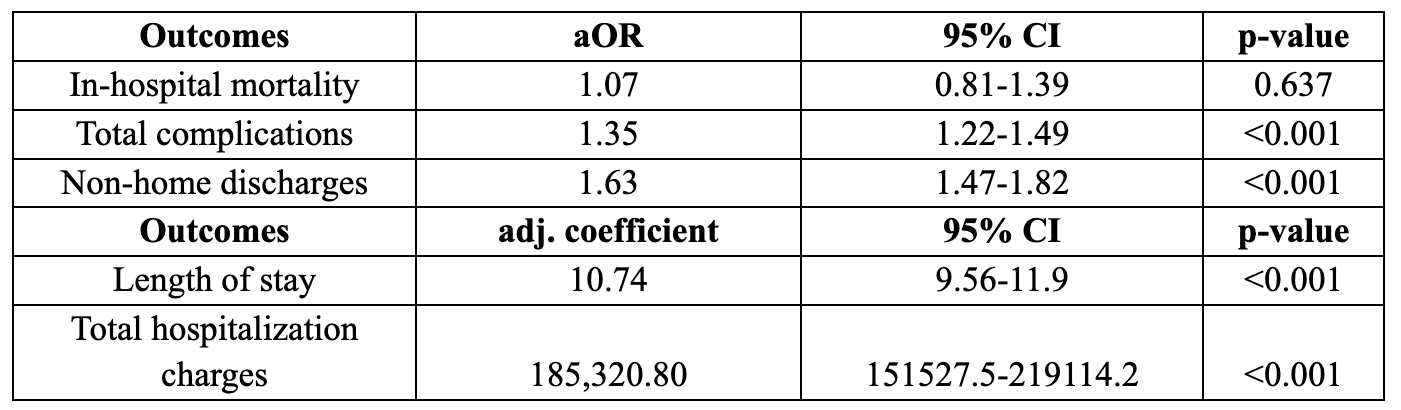
Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization
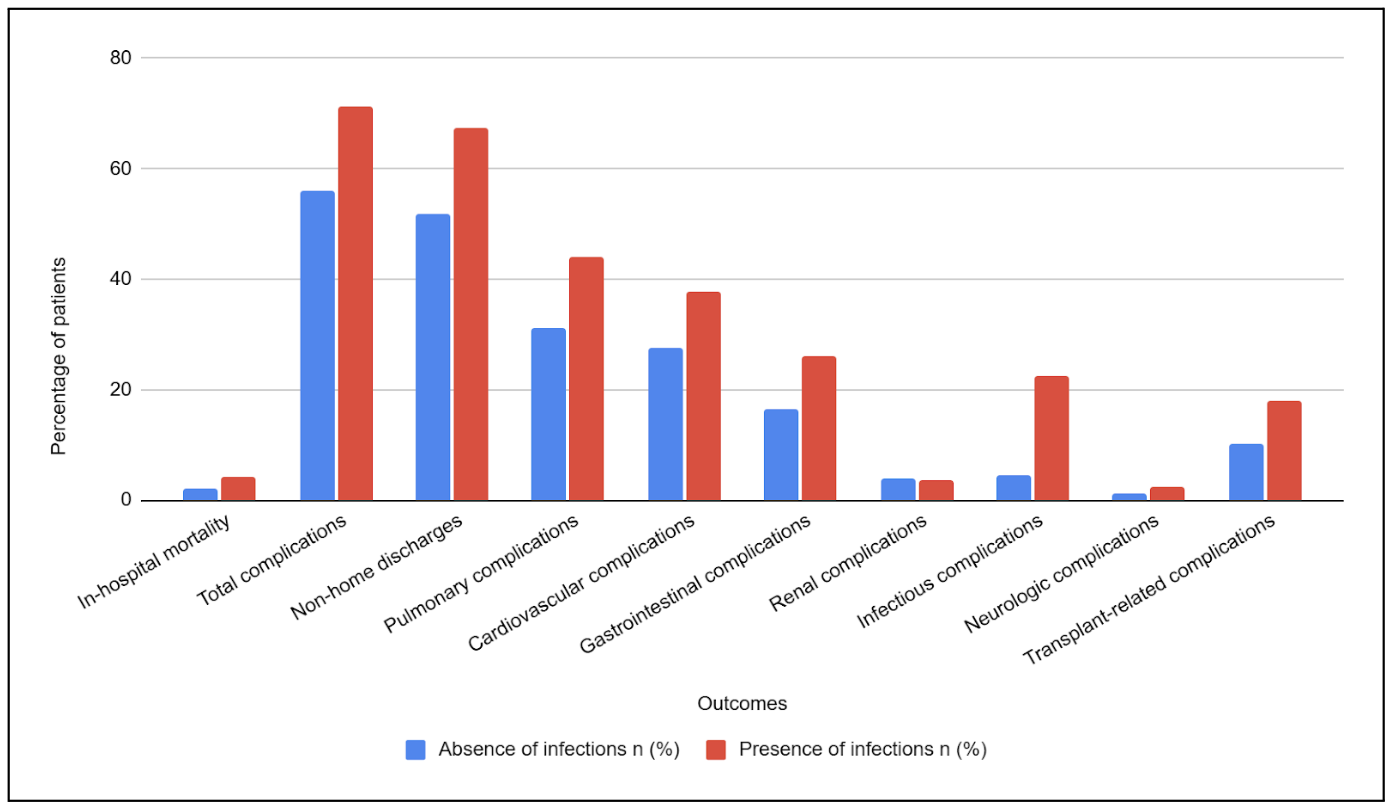
Figure: Figure 1. Bar chart comparing outcomes in patients undergoing LT stratified by the presence of infections
Disclosures:
Rahul Chikatimalla indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Mohammad Naseem indicated no relevant financial relationships.
Nishma Dhand indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Mohanad Al-Qaisi indicated no relevant financial relationships.
Rahul Chikatimalla, MBBS1, Carol Singh, MBBS2, Vishnu Yanamaladoddi, MD3, Mohammad Naseem, MBBS4, Nishma Dhand, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD3, Mohanad Al-Qaisi, MD3. P3623 - Burden and Impact of Infections in Patients Undergoing Liver Transplant: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
