Monday Poster Session
Category: Interventional Endoscopy
P3606 - Back to the Roux-tine: Glycemic Recovery After Fistula Closure
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LP
Lisa Pinero, MD (she/her/hers)
Icahn School of Medicine at Mount Sinai
New York City, NY
Presenting Author(s)
Lisa Pinero, MD1, Lily Ardente, MD1, Averill Guo, MD1, Anam Rizvi, MD1, Satish Nagula, MD2
1Icahn School of Medicine at Mount Sinai, New York City, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Roux-en-Y gastric bypass (RYGB) improves glycemic control by excluding the duodenum from nutrient flow, reducing insulin-antagonizing signals and enhancing GLP-1 secretion. Accessing the biliary system in RYGB patients often requires creation of a gastro-gastric (GG) fistula via Endoscopic ultrasound (EUS)-directed transgastric ERCP (EDGE). Our case illustrates the central role of duodenal nutrient exposure in glycemic regulation: a persistent gastro-gastric fistula led to diabetes, which fully resolved with endoscopic fistula closure.
Case Description/
Methods: A 72-year-old woman with a history of Roux-en-Y gastric bypass (RYGB) was diagnosed with choledocholithiasis after presenting with abdominal pain and elevated liver function tests. She underwent EUS-guided EDGE with gastro-gastric (GG) fistula creation using a 20 x 10 mm lumen-apposing metal stent (LAMS). A staged ERCP was subsequently performed with successful stone extraction. Although the LAMS was removed, the GG fistula was intentionally left open to allow future access to a duodenal polyp in case endoscopic mucosal resection became necessary.
Over the following 4 months, she developed new-onset diabetes mellitus without weight gain. Hemoglobin A1c rose from 6.2% (January 2023) to 9.4% (September 2023), peaking at 10.2% (June 2024) despite multiple anti-diabetic agents. The persistent GG fistula was suspected to be the cause, permitting nutrient flow to the excluded duodenum and disrupting glycemic control.
In November 2024, repeat EGD revealed a patent GG fistula in the gastric pouch. The tract was de-epithelialized with argon plasma coagulation, followed by endoscopic closure using suturing. Contrast injection confirmed successful closure with no leakage into the remnant stomach. By March 2025, her A1c had normalized to 5.3% without changes in weight or medications.
Discussion: This case highlights the duodenum’s active role in glucose homeostasis. In our case, restoration of nutrient flow to the duodenum via a persistent gastro-gastric fistula likely reactivated foregut-mediated hyperglycemic pathways, leading to new-onset diabetes despite stable weight. Resolution of hyperglycemia following fistula closure reinforces the impact of proximal gut nutrient exposure on glucose regulation and highlights this region as a potential target for metabolic disease therapy.
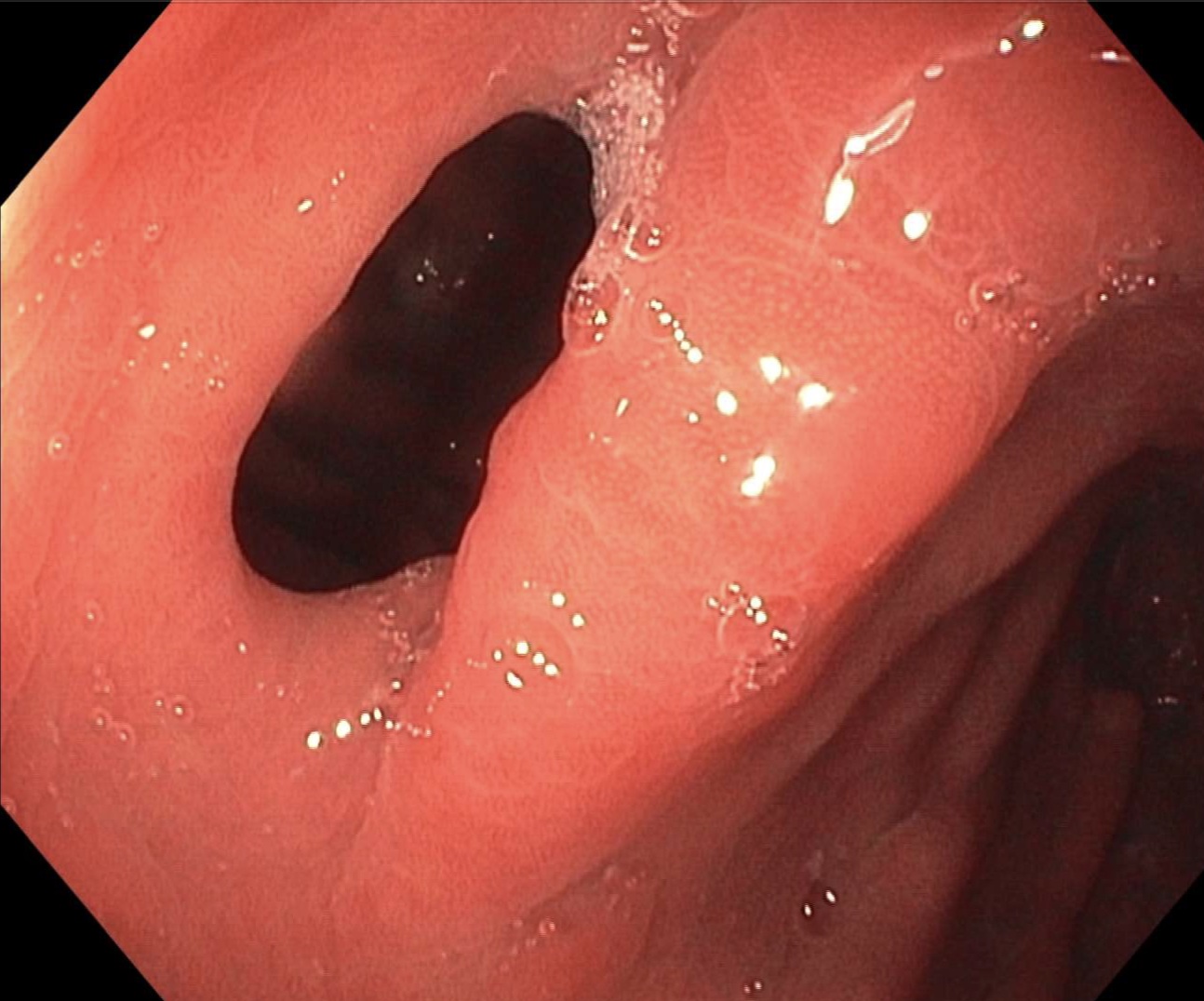
Figure: Image 1: Patent gastro-gastric fistula was identified in the mid gastric pouch.
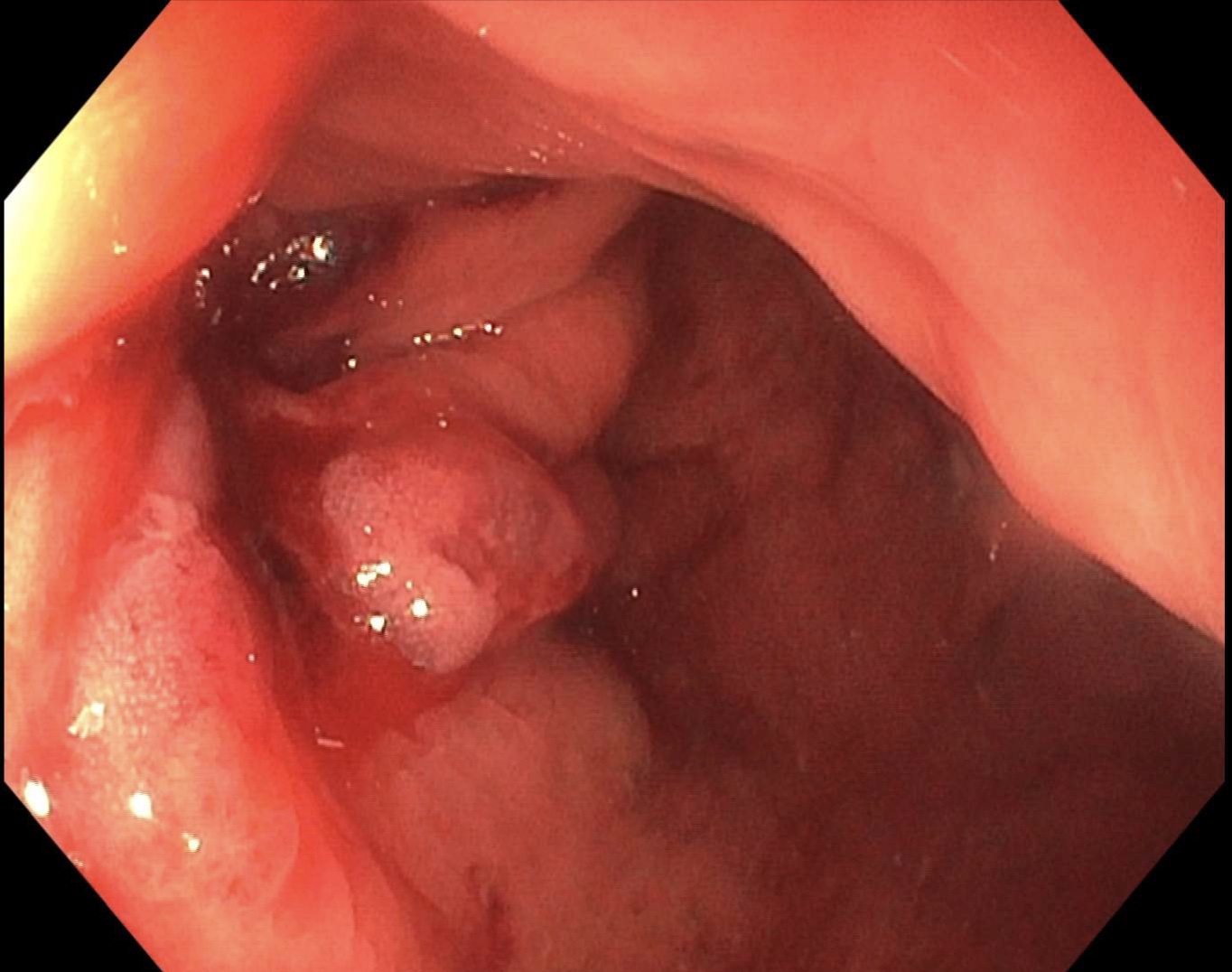
Figure: Image 2: Successful closure of gastro-gastric fistula.
Disclosures:
Lisa Pinero indicated no relevant financial relationships.
Lily Ardente indicated no relevant financial relationships.
Averill Guo indicated no relevant financial relationships.
Anam Rizvi indicated no relevant financial relationships.
Satish Nagula indicated no relevant financial relationships.
Lisa Pinero, MD1, Lily Ardente, MD1, Averill Guo, MD1, Anam Rizvi, MD1, Satish Nagula, MD2. P3606 - Back to the Roux-tine: Glycemic Recovery After Fistula Closure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York City, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Roux-en-Y gastric bypass (RYGB) improves glycemic control by excluding the duodenum from nutrient flow, reducing insulin-antagonizing signals and enhancing GLP-1 secretion. Accessing the biliary system in RYGB patients often requires creation of a gastro-gastric (GG) fistula via Endoscopic ultrasound (EUS)-directed transgastric ERCP (EDGE). Our case illustrates the central role of duodenal nutrient exposure in glycemic regulation: a persistent gastro-gastric fistula led to diabetes, which fully resolved with endoscopic fistula closure.
Case Description/
Methods: A 72-year-old woman with a history of Roux-en-Y gastric bypass (RYGB) was diagnosed with choledocholithiasis after presenting with abdominal pain and elevated liver function tests. She underwent EUS-guided EDGE with gastro-gastric (GG) fistula creation using a 20 x 10 mm lumen-apposing metal stent (LAMS). A staged ERCP was subsequently performed with successful stone extraction. Although the LAMS was removed, the GG fistula was intentionally left open to allow future access to a duodenal polyp in case endoscopic mucosal resection became necessary.
Over the following 4 months, she developed new-onset diabetes mellitus without weight gain. Hemoglobin A1c rose from 6.2% (January 2023) to 9.4% (September 2023), peaking at 10.2% (June 2024) despite multiple anti-diabetic agents. The persistent GG fistula was suspected to be the cause, permitting nutrient flow to the excluded duodenum and disrupting glycemic control.
In November 2024, repeat EGD revealed a patent GG fistula in the gastric pouch. The tract was de-epithelialized with argon plasma coagulation, followed by endoscopic closure using suturing. Contrast injection confirmed successful closure with no leakage into the remnant stomach. By March 2025, her A1c had normalized to 5.3% without changes in weight or medications.
Discussion: This case highlights the duodenum’s active role in glucose homeostasis. In our case, restoration of nutrient flow to the duodenum via a persistent gastro-gastric fistula likely reactivated foregut-mediated hyperglycemic pathways, leading to new-onset diabetes despite stable weight. Resolution of hyperglycemia following fistula closure reinforces the impact of proximal gut nutrient exposure on glucose regulation and highlights this region as a potential target for metabolic disease therapy.
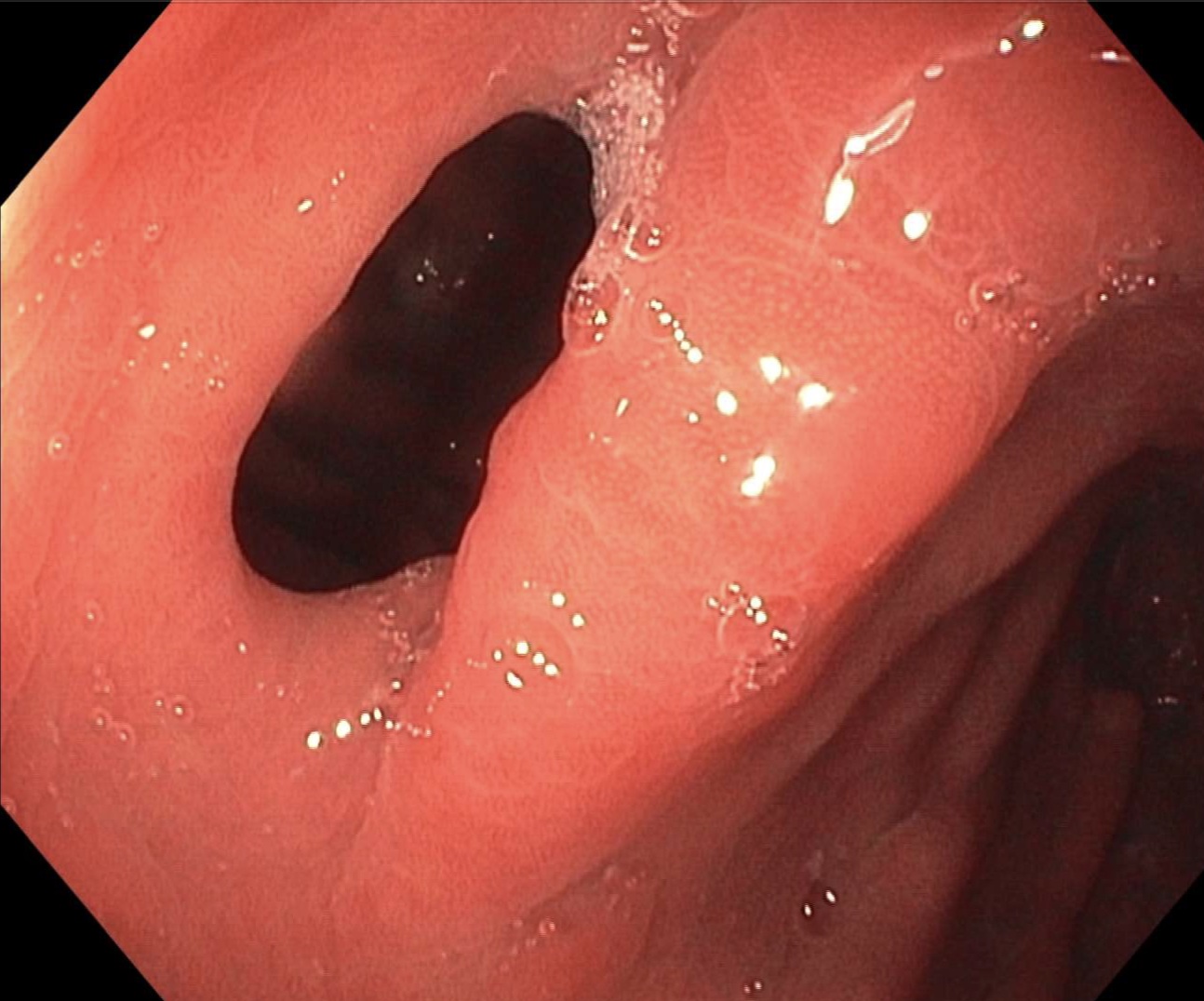
Figure: Image 1: Patent gastro-gastric fistula was identified in the mid gastric pouch.
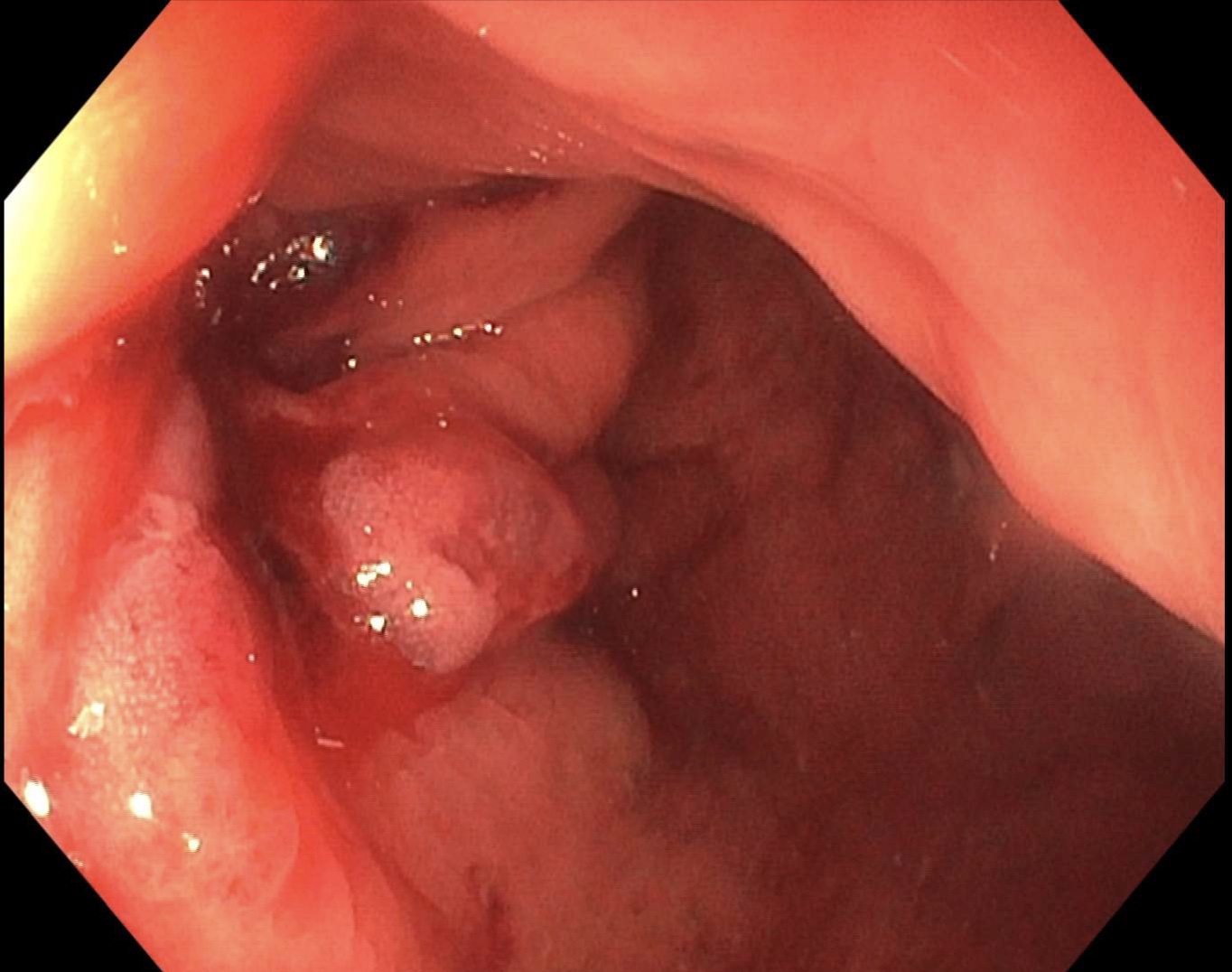
Figure: Image 2: Successful closure of gastro-gastric fistula.
Disclosures:
Lisa Pinero indicated no relevant financial relationships.
Lily Ardente indicated no relevant financial relationships.
Averill Guo indicated no relevant financial relationships.
Anam Rizvi indicated no relevant financial relationships.
Satish Nagula indicated no relevant financial relationships.
Lisa Pinero, MD1, Lily Ardente, MD1, Averill Guo, MD1, Anam Rizvi, MD1, Satish Nagula, MD2. P3606 - Back to the Roux-tine: Glycemic Recovery After Fistula Closure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
