Monday Poster Session
Category: Interventional Endoscopy
P3604 - Surgery-Sparing Management of Gastric GISTs Using Submucosal Tunneling Endoscopic Resection: Experience From 2 Distinct Anatomical Presentations
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aizaz Khan, MD (he/him/his)
University of Massachusetts Chan Medical School - Baystate Health
Springfield, MA
Presenting Author(s)
Award: ACG Presidential Poster Award
Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Kais Zakharia, MD3
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate Medical Center, Enfield, CT; 3Baystate Health, Springfield, MA
Introduction: Gastrointestinal stromal tumors (GISTs) arising from the muscularis propria have traditionally required surgical intervention for management. However, tumors near the gastroesophageal (GE) junction or in anatomically complex areas pose technical challenges that may necessitate subtotal or total gastrectomy. Submucosal tunneling endoscopic resection (STER) offers a minimally invasive, organ-preserving alternative. We present two cases of gastric GISTs—one near the GE junction and one in the mid-gastric body—successfully managed using STER.
Case Description/
Methods: Case 1: A 69-year-old female underwent MRI for follow-up of a presumed pancreatic cyst, incidentally revealing a 2.5 cm mass at the lesser curvature near the GE junction. EUS demonstrated a 2.1 × 1.8 cm hypoechoic lesion arising from the muscularis propria. Fine-needle biopsy (FNB) confirmed a spindle cell GIST (DOG1, desmin, caldesmin positive). Surgical oncology recommended near total gastrectomy, but the patient opted for STER. A submucosal tunnel was created 5 cm proximal to the lesion using a hybrid knife after methylene blue–saline injection. The mass was resected en bloc with traction-assisted dissection and retrieved using rat-tooth forceps. Mucosal entry was closed with through-the-scope clips. Pathology confirmed a 3.2 cm GIST with focal margin involvement likely due to retrieval artifact. No necrosis or high mitotic activity was noted.
Case 2: A 72-year-old male was evaluated for a gastric lesion found during imaging for abdominal pain. EUS showed a 2.3 × 2 cm homogenous, hypoechoic mass with central anechoic area in the anterior gastric body. FNB revealed a mixed epithelioid and spindle cell GIST (C-KIT, DOG1 positive). STER was performed similarly. A Mantis clip and thread were used for traction, and myotomy was performed using an IT nano knife. The mass was retrieved with a rescue net. Pathology confirmed a 2.5 cm low-grade GIST with negative margins.
Discussion: These cases demonstrate the feasibility and effectiveness of STER in managing gastric GISTs located in anatomically complex regions. STER enabled complete resection while preserving gastric anatomy and avoiding high-morbidity surgery. This approach may serve as a safe and durable alternative in carefully selected patients.
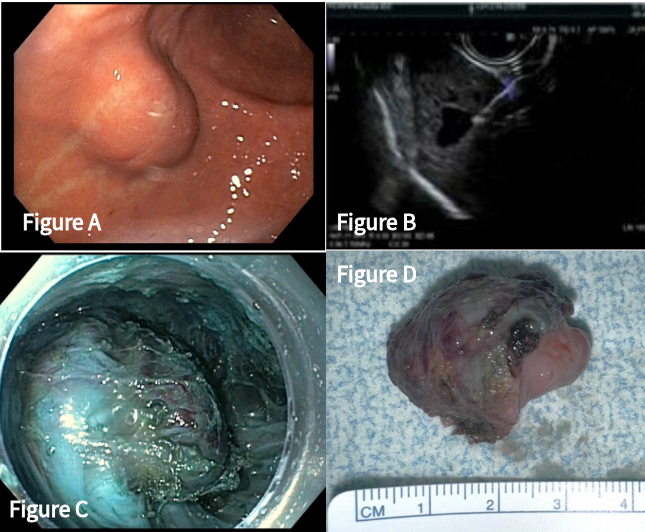
Figure: Figure A - 2.5cm exophytic mass seen on the medial aspect of the gastric fundus during upper endoscopy.
Figure B - 2.3 x 2cm hypoechoic mass with anechoic fluid center rising from the muscularis proprio noted on EUS.
Figure C - Visualized subepithelial mass during dissection process of STER procedure.
Figure D - 2.5cm tumor post-retrieval after STER

Figure: Figure E - 2cm subepithelial mass along less curvature on upper endoscopy
Figure F - 2.1 x 1.8cm well-circumscribed, hypoechoic masswith hyperechoic foci on EUS
Figure G - Submucosal tunneling with dissection of mass
Figure H - 3.2cm tumor post-retreival after STER
Disclosures:
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Kais Zakharia indicated no relevant financial relationships.
Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Kais Zakharia, MD3. P3604 - Surgery-Sparing Management of Gastric GISTs Using Submucosal Tunneling Endoscopic Resection: Experience From 2 Distinct Anatomical Presentations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Kais Zakharia, MD3
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate Medical Center, Enfield, CT; 3Baystate Health, Springfield, MA
Introduction: Gastrointestinal stromal tumors (GISTs) arising from the muscularis propria have traditionally required surgical intervention for management. However, tumors near the gastroesophageal (GE) junction or in anatomically complex areas pose technical challenges that may necessitate subtotal or total gastrectomy. Submucosal tunneling endoscopic resection (STER) offers a minimally invasive, organ-preserving alternative. We present two cases of gastric GISTs—one near the GE junction and one in the mid-gastric body—successfully managed using STER.
Case Description/
Methods: Case 1: A 69-year-old female underwent MRI for follow-up of a presumed pancreatic cyst, incidentally revealing a 2.5 cm mass at the lesser curvature near the GE junction. EUS demonstrated a 2.1 × 1.8 cm hypoechoic lesion arising from the muscularis propria. Fine-needle biopsy (FNB) confirmed a spindle cell GIST (DOG1, desmin, caldesmin positive). Surgical oncology recommended near total gastrectomy, but the patient opted for STER. A submucosal tunnel was created 5 cm proximal to the lesion using a hybrid knife after methylene blue–saline injection. The mass was resected en bloc with traction-assisted dissection and retrieved using rat-tooth forceps. Mucosal entry was closed with through-the-scope clips. Pathology confirmed a 3.2 cm GIST with focal margin involvement likely due to retrieval artifact. No necrosis or high mitotic activity was noted.
Case 2: A 72-year-old male was evaluated for a gastric lesion found during imaging for abdominal pain. EUS showed a 2.3 × 2 cm homogenous, hypoechoic mass with central anechoic area in the anterior gastric body. FNB revealed a mixed epithelioid and spindle cell GIST (C-KIT, DOG1 positive). STER was performed similarly. A Mantis clip and thread were used for traction, and myotomy was performed using an IT nano knife. The mass was retrieved with a rescue net. Pathology confirmed a 2.5 cm low-grade GIST with negative margins.
Discussion: These cases demonstrate the feasibility and effectiveness of STER in managing gastric GISTs located in anatomically complex regions. STER enabled complete resection while preserving gastric anatomy and avoiding high-morbidity surgery. This approach may serve as a safe and durable alternative in carefully selected patients.
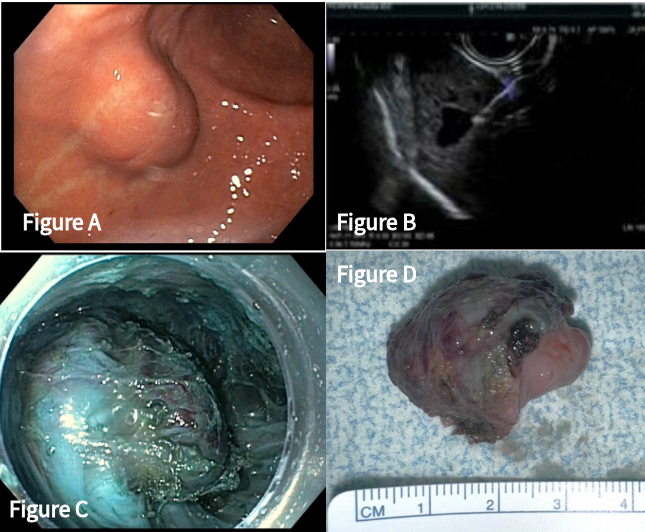
Figure: Figure A - 2.5cm exophytic mass seen on the medial aspect of the gastric fundus during upper endoscopy.
Figure B - 2.3 x 2cm hypoechoic mass with anechoic fluid center rising from the muscularis proprio noted on EUS.
Figure C - Visualized subepithelial mass during dissection process of STER procedure.
Figure D - 2.5cm tumor post-retrieval after STER

Figure: Figure E - 2cm subepithelial mass along less curvature on upper endoscopy
Figure F - 2.1 x 1.8cm well-circumscribed, hypoechoic masswith hyperechoic foci on EUS
Figure G - Submucosal tunneling with dissection of mass
Figure H - 3.2cm tumor post-retreival after STER
Disclosures:
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Kais Zakharia indicated no relevant financial relationships.
Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Kais Zakharia, MD3. P3604 - Surgery-Sparing Management of Gastric GISTs Using Submucosal Tunneling Endoscopic Resection: Experience From 2 Distinct Anatomical Presentations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

