Monday Poster Session
Category: Interventional Endoscopy
P3597 - Here a LAMS, There a LAMS: Management of Refractory Hepaticojejunostomy Anastomotic Stricture With Lumen Apposing Metal Stent (LAMS) Following Recurrent Plastic Stent Migration
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SD
Sarah Dang, MD
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Sarah Dang, MD, Jerome C. Edelson, MD, Zachary Eagle, MD
Brooke Army Medical Center, San Antonio, TX
Introduction: We present a case of hepaticojejunostomy (HJ) anastomotic stricture after Whipple procedure with management complicated by multiple plastic stent migrations – infrequently a complication in a common management strategy. The stricture was ultimately managed with a lumen apposing metal stent (LAMS) - a potential new strategy for refractory strictures.
Case Description/
Methods: A 59-year-old male with history of a Whipple resection for a neuroendocrine tumor presented with abdominal pain, chills, and elevated LFTs, and was found to have acute cholangitis. MRI showed filling defects in the left and right hepatic ducts extending to the HJ. He underwent an ERCP with evidence of cholangitis and stenosis of the HJ, which was dilated with a balloon. A 7Fr x 5cm plastic stent was placed across the HJ. Due to a short extrahepatic bile duct, a fully covered self-expandable metal stent (FCSEMS) could not be placed as it would have been < 1cm from the bifurcation. Two months later, he returned for stent exchange and 3x 7Fr x 5cm plastic stents were placed. Repeat ERCP showed migration of one stent, and due to improvement in HJ stenosis, the remaining stents were removed. Nine days later he returned with cholangitis and underwent ERCP with placement of 2x 10Fr x 5cm plastic stents. Again, another stent migrated. With his next ERCP, he underwent placement of four plastic stents. Two of these stents migrated prior to his next ERCP performed two months later. With incomplete resolution of stricture complicated by recurrent stent migration, the decision was made to utilize a LAMS for management. A 10 mm x 10 mm LAMS was placed across the HJ and the patient has done well, without recurrent symptoms.
Discussion: This case highlights the complexities in management of HJ anastomotic strictures. Post operative strictures occurs in 2.6% of cases, most often presenting with jaundice by 13 months (1). Typical endoscopic management includes balloon dilation, plastic stent placement, or FCSEMS.
Given his persistent stricture, recurrent stent migration, and anatomy that did not allow for FCSEMS placement, alternative strategies were considered and ultimately a LAMS was used with good treatment response to date. There is a paucity of data on its use for this purpose, and it may be an alternative method for refractory anastomotic strictures; further investigation is needed regarding its long term outcomes.
(1) House, Michael et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. MAY2006, 571-576.
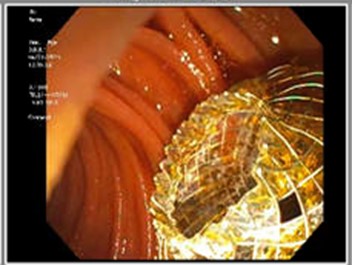
Figure: Filling defect due to HJ anastomotic stricture on initial ERCP, short extrahepatic bile duct (arrow)
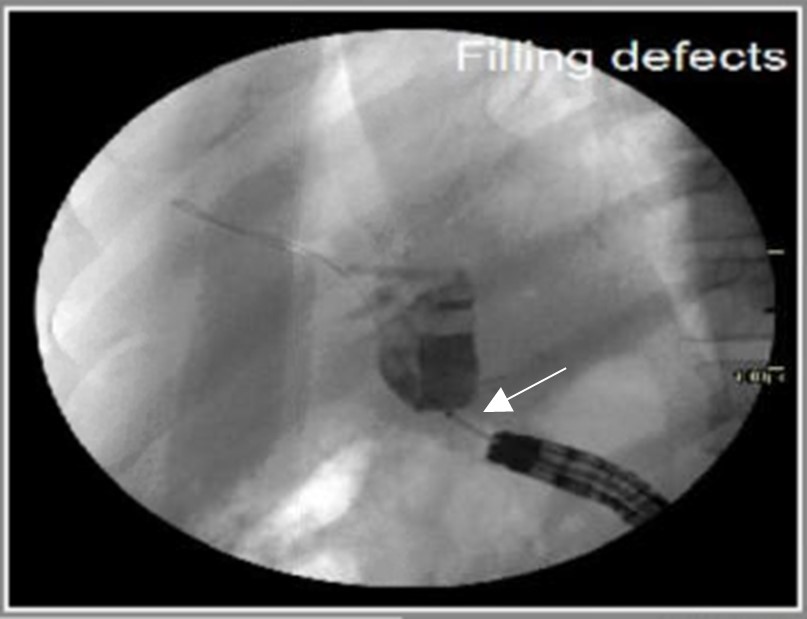
Figure: LAMS deployed across the HJ stricture
Disclosures:
Sarah Dang indicated no relevant financial relationships.
Jerome Edelson indicated no relevant financial relationships.
Zachary Eagle indicated no relevant financial relationships.
Sarah Dang, MD, Jerome C. Edelson, MD, Zachary Eagle, MD. P3597 - Here a LAMS, There a LAMS: Management of Refractory Hepaticojejunostomy Anastomotic Stricture With Lumen Apposing Metal Stent (LAMS) Following Recurrent Plastic Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: We present a case of hepaticojejunostomy (HJ) anastomotic stricture after Whipple procedure with management complicated by multiple plastic stent migrations – infrequently a complication in a common management strategy. The stricture was ultimately managed with a lumen apposing metal stent (LAMS) - a potential new strategy for refractory strictures.
Case Description/
Methods: A 59-year-old male with history of a Whipple resection for a neuroendocrine tumor presented with abdominal pain, chills, and elevated LFTs, and was found to have acute cholangitis. MRI showed filling defects in the left and right hepatic ducts extending to the HJ. He underwent an ERCP with evidence of cholangitis and stenosis of the HJ, which was dilated with a balloon. A 7Fr x 5cm plastic stent was placed across the HJ. Due to a short extrahepatic bile duct, a fully covered self-expandable metal stent (FCSEMS) could not be placed as it would have been < 1cm from the bifurcation. Two months later, he returned for stent exchange and 3x 7Fr x 5cm plastic stents were placed. Repeat ERCP showed migration of one stent, and due to improvement in HJ stenosis, the remaining stents were removed. Nine days later he returned with cholangitis and underwent ERCP with placement of 2x 10Fr x 5cm plastic stents. Again, another stent migrated. With his next ERCP, he underwent placement of four plastic stents. Two of these stents migrated prior to his next ERCP performed two months later. With incomplete resolution of stricture complicated by recurrent stent migration, the decision was made to utilize a LAMS for management. A 10 mm x 10 mm LAMS was placed across the HJ and the patient has done well, without recurrent symptoms.
Discussion: This case highlights the complexities in management of HJ anastomotic strictures. Post operative strictures occurs in 2.6% of cases, most often presenting with jaundice by 13 months (1). Typical endoscopic management includes balloon dilation, plastic stent placement, or FCSEMS.
Given his persistent stricture, recurrent stent migration, and anatomy that did not allow for FCSEMS placement, alternative strategies were considered and ultimately a LAMS was used with good treatment response to date. There is a paucity of data on its use for this purpose, and it may be an alternative method for refractory anastomotic strictures; further investigation is needed regarding its long term outcomes.
(1) House, Michael et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. MAY2006, 571-576.
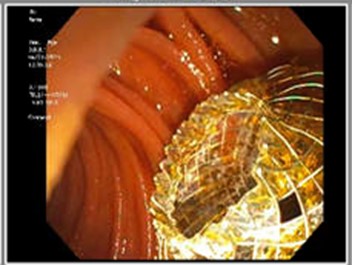
Figure: Filling defect due to HJ anastomotic stricture on initial ERCP, short extrahepatic bile duct (arrow)
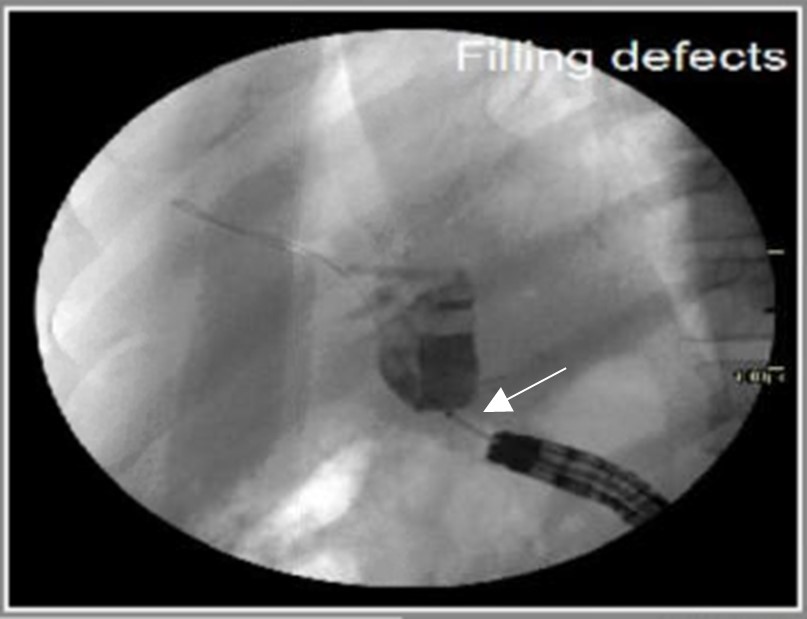
Figure: LAMS deployed across the HJ stricture
Disclosures:
Sarah Dang indicated no relevant financial relationships.
Jerome Edelson indicated no relevant financial relationships.
Zachary Eagle indicated no relevant financial relationships.
Sarah Dang, MD, Jerome C. Edelson, MD, Zachary Eagle, MD. P3597 - Here a LAMS, There a LAMS: Management of Refractory Hepaticojejunostomy Anastomotic Stricture With Lumen Apposing Metal Stent (LAMS) Following Recurrent Plastic Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
