Monday Poster Session
Category: Interventional Endoscopy
P3596 - Cannabinoid Hyperemesis Syndrome and Gastroparesis: A Complex Case Resolved with Endoscopic Pyloric Dilation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Evelyn Inga, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Evelyn Inga, MD1, Christopher Chang, MD, PhD2
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Persistent nausea and abdominal pain have a broad differential, especially in patients with type 1 diabetes mellitus (T1DM). Cannabinoid Hyperemesis Syndrome (CHS) and diabetic gastroparesis may overlap. We present a 23 year-old woman with T1DM and chronic GI symptoms, initially diagnosed with CHS, later found to have pyloric stenosis and delayed gastric emptying. Despite conventional therapy, symptoms persisted until endoscopic pyloric balloon dilation was performed, resulting in sustained improvement. This case highlights the importance of ruling out anatomical causes, utilizing endoscopy, and adopting multidisciplinary care to optimize outcomes in complex GI presentations.
Case Description/
Methods: A 23-year-old female with T1DM presented with a year of persistent nausea, vomiting, and abdominal discomfort. She was previously diagnosed with CHS, with suspected gastroparesis. Her diabetes was poorly controlled (HbA1c of 8.1%) complicated by multiple episodes of DKA. She reported chronic daily cannabis use.
The patient first presented to the ED with worsening GI symptoms. She had tachycardia and mild generalized abdominal tenderness. Laboratory showed leukocytosis, hyperglycemia, and positive urinary THC. Imaging was benign. Given her chronic symptoms and cannabis use, CHS was suspected, but the overlap with gastroparesis symptoms required further evaluation. Initial treatments included proton pump inhibitors (PPIs), sucralfate, and dietary modifications: low-fat, small-volume meals. Despite these interventions, her symptoms persisted. A pre-endoscopy gastric emptying study was attempted to confirm gastroparesis but was inconclusive due to the patient’s inability to tolerate oral intake. Contrast esophagogram suggested delayed gastric emptying. Initial EGD showed Los Angeles grade D esophagitis, and a tight pylorus which was dilated to 15 mm using an endoscopic balloon. Repeat EGD showed improving esophagitis, normal pylorus. Sustained symptom improvement correlated with improved gastric function, although intermittent esophagitis required ongoing management with PPI’s.
Discussion: This case teaches clinicians to prioritize anatomic causes like pyloric stenosis in refractory T1DM cases, emphasizes glycemic control to prevent neuropathy, and leverage multidisciplinary teams. Future research should explore long-term outcomes of pyloric dilation and better biomarkers to distinguish CHS from gastroparesis. Until then, adaptability remains key to bridging gaps between evidence and patient care.
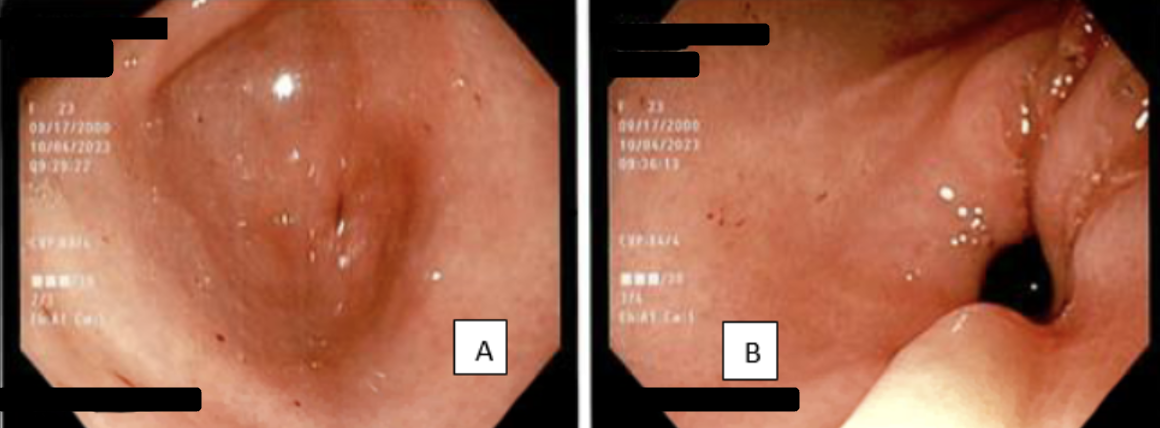
Figure: A) Pre-Dilation Pyloric Stenosis
B) Post-Dilation Pylorus is now normal sized
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Evelyn Inga, MD1, Christopher Chang, MD, PhD2. P3596 - Cannabinoid Hyperemesis Syndrome and Gastroparesis: A Complex Case Resolved with Endoscopic Pyloric Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Persistent nausea and abdominal pain have a broad differential, especially in patients with type 1 diabetes mellitus (T1DM). Cannabinoid Hyperemesis Syndrome (CHS) and diabetic gastroparesis may overlap. We present a 23 year-old woman with T1DM and chronic GI symptoms, initially diagnosed with CHS, later found to have pyloric stenosis and delayed gastric emptying. Despite conventional therapy, symptoms persisted until endoscopic pyloric balloon dilation was performed, resulting in sustained improvement. This case highlights the importance of ruling out anatomical causes, utilizing endoscopy, and adopting multidisciplinary care to optimize outcomes in complex GI presentations.
Case Description/
Methods: A 23-year-old female with T1DM presented with a year of persistent nausea, vomiting, and abdominal discomfort. She was previously diagnosed with CHS, with suspected gastroparesis. Her diabetes was poorly controlled (HbA1c of 8.1%) complicated by multiple episodes of DKA. She reported chronic daily cannabis use.
The patient first presented to the ED with worsening GI symptoms. She had tachycardia and mild generalized abdominal tenderness. Laboratory showed leukocytosis, hyperglycemia, and positive urinary THC. Imaging was benign. Given her chronic symptoms and cannabis use, CHS was suspected, but the overlap with gastroparesis symptoms required further evaluation. Initial treatments included proton pump inhibitors (PPIs), sucralfate, and dietary modifications: low-fat, small-volume meals. Despite these interventions, her symptoms persisted. A pre-endoscopy gastric emptying study was attempted to confirm gastroparesis but was inconclusive due to the patient’s inability to tolerate oral intake. Contrast esophagogram suggested delayed gastric emptying. Initial EGD showed Los Angeles grade D esophagitis, and a tight pylorus which was dilated to 15 mm using an endoscopic balloon. Repeat EGD showed improving esophagitis, normal pylorus. Sustained symptom improvement correlated with improved gastric function, although intermittent esophagitis required ongoing management with PPI’s.
Discussion: This case teaches clinicians to prioritize anatomic causes like pyloric stenosis in refractory T1DM cases, emphasizes glycemic control to prevent neuropathy, and leverage multidisciplinary teams. Future research should explore long-term outcomes of pyloric dilation and better biomarkers to distinguish CHS from gastroparesis. Until then, adaptability remains key to bridging gaps between evidence and patient care.
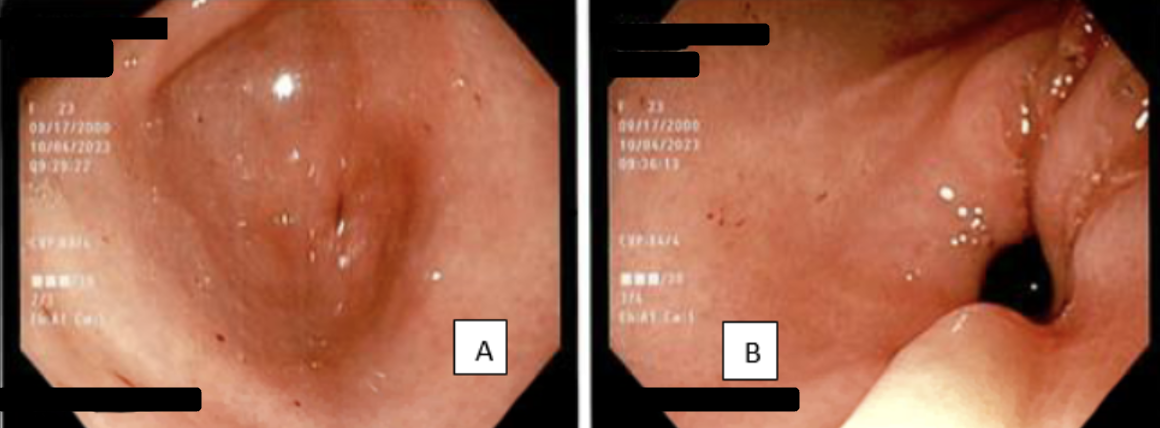
Figure: A) Pre-Dilation Pyloric Stenosis
B) Post-Dilation Pylorus is now normal sized
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Evelyn Inga, MD1, Christopher Chang, MD, PhD2. P3596 - Cannabinoid Hyperemesis Syndrome and Gastroparesis: A Complex Case Resolved with Endoscopic Pyloric Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
