Monday Poster Session
Category: Interventional Endoscopy
P3566 - Severe Malnutrition and Diarrhea due to Gastrocolic Fistula Post-Roux-en-Y: Role of Endoscopic Stenting in Bridging to Surgery
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Abdul Subhan Talpur, MD
United Health Services, Wilson Medical Center
Johnson City, NY
Presenting Author(s)
Abdul Subhan Talpur, MD1, Fawad Talat, MD1, Muhammad Ahmed, MD1, Sadia Tabassum, MD2, Hammad Qadri, DO3, Usama Sakhawat, MD1, Khandokar A. Talib, MD3, Mustafa Sajjad Cheema, MBBS4, Ibrar Atiq, MD1, Gegin George, MD2, Abdelhamid Ben Selma, MD1, Toseef Javaid, MD1
1United Health Services, Wilson Medical Center, Johnson City, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3United Health Services, Wilson Medical Center, Vestal, NY; 4CMH Lahore Medical College and Institute of Dentistry, Lahore, Punjab, Pakistan
Introduction: Gastrocolic fistula is a rare and serious problem that may occur after gastrointestinal surgery. It usually presents with chronic diarrhea and severe malnutrition. Although endoscopic interventions could act as a link to definitive surgical treatment, outcomes for severely debilitated patients remain poor. We report a case of a large size gastrocolic fistula that occurred after Roux-en-Y reconstruction and proved fatal, even with endoscopic stenting.
Case Description/
Methods: A 56-year-old male patient presented with symptoms of generalized weakness, cachexia, severe chronic diarrhea, and a history of perforated duodenal ulcer status post Roux-en-Y gastrojejunostomy, several surgical revisions, crohn's disease and HCV disease.
Initially, the patient was treated based on symptoms. All necessary laboratory tests were conducted, including a slightly elevated faecal calpoprotein and faecal analysis, which eliminated the possibility of an infectious cause. An endoscopy revealed a large gastrocolic fistula near the gastrojejunal anastomosis, as well as a clean-based marginal ulcer spanning the mid-gastric body to the transverse colon. Protein-calorie malnutrition was evident, so TPN was recommended. The patient left the hospital against doctors' advice, but was later readmitted as symptoms got worse.
Repeated EGD revealed a common fistulous cavity involving the colon and jejunum. A self-expandable metallic stent (18 mm x 149 mm) was placed via endoscopy to bridge the gastrojejunal and jejunojejunal anastomoses and cover the fistula. Subsequently, the patient showed signs of stabilization and leakage of contrast was not detected during fluoroscopy. This stenting was performed to stablilize the patient for subsequent surgical intervention.
Despite the successful endoscopic intervention, severe malnutrition and systemic deconditioning worsened the patient's condition. The patient succumbed within 20 days, before planned surgical intervention or stent removal.
Discussion: This case highlights the serious consequences of enteric fistula formation in post-surgical patients, especially when accompanied by chronic malnutrition and systemic illness. Although endoscopic stenting can be used as a temporary measure, survival rates are low without adequate nutritional reserves and timely definitive surgery. This case emphasises the importance of early detection, nutritional support, and close interdisciplinary management for patients suffering from complex post-surgical GI complications.
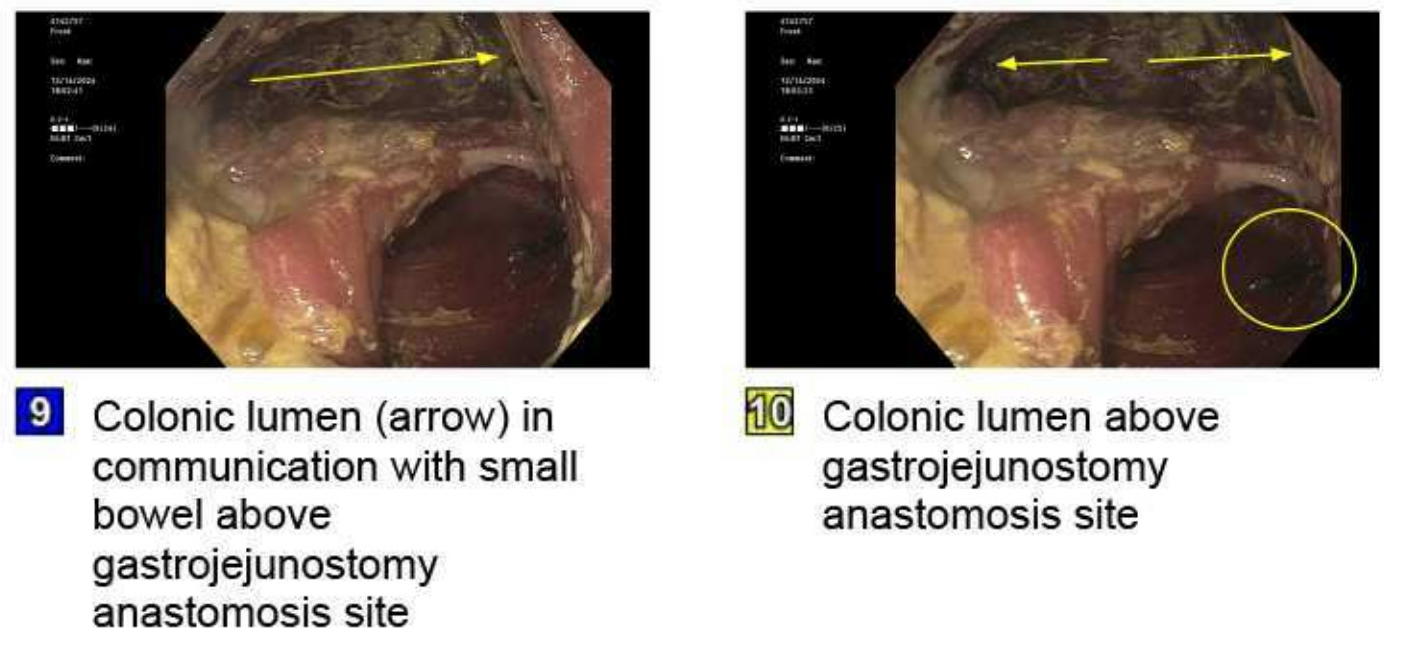
Figure: This image depicts colonic lumen in communication with small bowel above gastrojejunostomy anastomosis site.

Figure: A 18 mm X 149mm fully covered self expandable metallic stent (SEMS) was placed at Jejunojejunal anastomosis.
Disclosures:
Abdul Subhan Talpur indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Mustafa Sajjad Cheema indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Gegin George indicated no relevant financial relationships.
Abdelhamid Ben Selma indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Abdul Subhan Talpur, MD1, Fawad Talat, MD1, Muhammad Ahmed, MD1, Sadia Tabassum, MD2, Hammad Qadri, DO3, Usama Sakhawat, MD1, Khandokar A. Talib, MD3, Mustafa Sajjad Cheema, MBBS4, Ibrar Atiq, MD1, Gegin George, MD2, Abdelhamid Ben Selma, MD1, Toseef Javaid, MD1. P3566 - Severe Malnutrition and Diarrhea due to Gastrocolic Fistula Post-Roux-en-Y: Role of Endoscopic Stenting in Bridging to Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Johnson City, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3United Health Services, Wilson Medical Center, Vestal, NY; 4CMH Lahore Medical College and Institute of Dentistry, Lahore, Punjab, Pakistan
Introduction: Gastrocolic fistula is a rare and serious problem that may occur after gastrointestinal surgery. It usually presents with chronic diarrhea and severe malnutrition. Although endoscopic interventions could act as a link to definitive surgical treatment, outcomes for severely debilitated patients remain poor. We report a case of a large size gastrocolic fistula that occurred after Roux-en-Y reconstruction and proved fatal, even with endoscopic stenting.
Case Description/
Methods: A 56-year-old male patient presented with symptoms of generalized weakness, cachexia, severe chronic diarrhea, and a history of perforated duodenal ulcer status post Roux-en-Y gastrojejunostomy, several surgical revisions, crohn's disease and HCV disease.
Initially, the patient was treated based on symptoms. All necessary laboratory tests were conducted, including a slightly elevated faecal calpoprotein and faecal analysis, which eliminated the possibility of an infectious cause. An endoscopy revealed a large gastrocolic fistula near the gastrojejunal anastomosis, as well as a clean-based marginal ulcer spanning the mid-gastric body to the transverse colon. Protein-calorie malnutrition was evident, so TPN was recommended. The patient left the hospital against doctors' advice, but was later readmitted as symptoms got worse.
Repeated EGD revealed a common fistulous cavity involving the colon and jejunum. A self-expandable metallic stent (18 mm x 149 mm) was placed via endoscopy to bridge the gastrojejunal and jejunojejunal anastomoses and cover the fistula. Subsequently, the patient showed signs of stabilization and leakage of contrast was not detected during fluoroscopy. This stenting was performed to stablilize the patient for subsequent surgical intervention.
Despite the successful endoscopic intervention, severe malnutrition and systemic deconditioning worsened the patient's condition. The patient succumbed within 20 days, before planned surgical intervention or stent removal.
Discussion: This case highlights the serious consequences of enteric fistula formation in post-surgical patients, especially when accompanied by chronic malnutrition and systemic illness. Although endoscopic stenting can be used as a temporary measure, survival rates are low without adequate nutritional reserves and timely definitive surgery. This case emphasises the importance of early detection, nutritional support, and close interdisciplinary management for patients suffering from complex post-surgical GI complications.
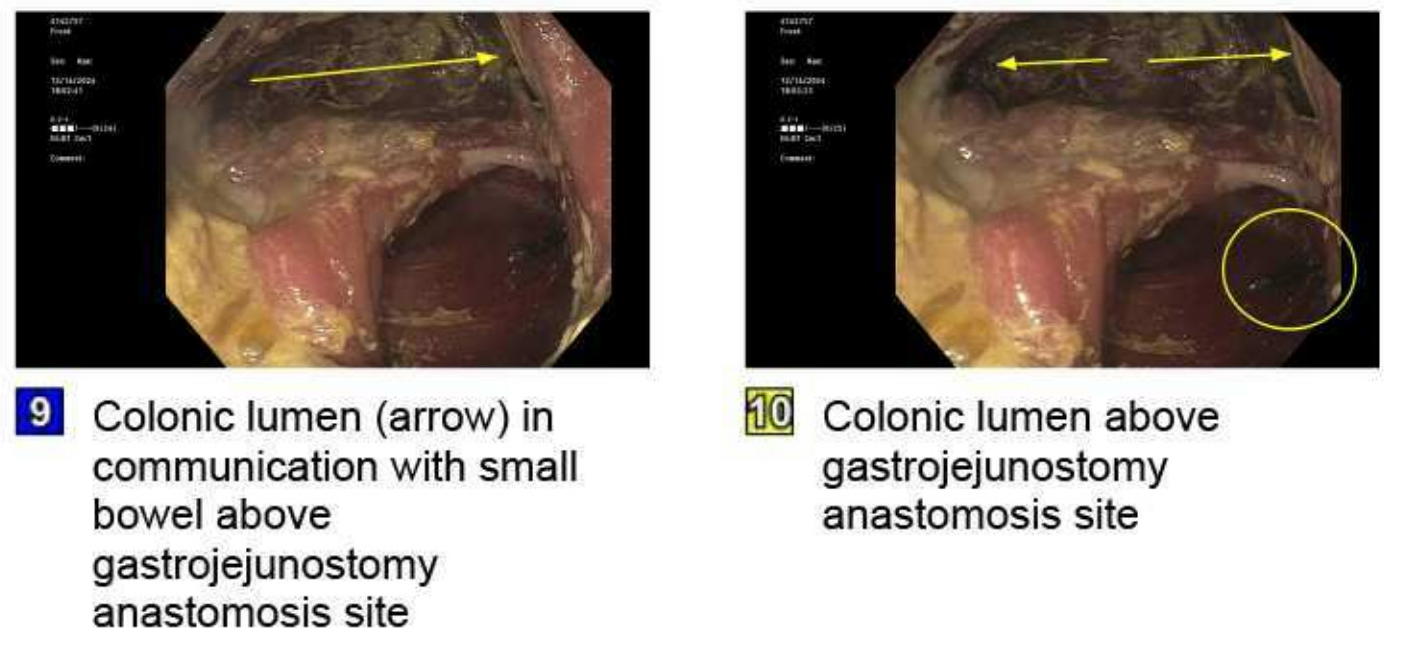
Figure: This image depicts colonic lumen in communication with small bowel above gastrojejunostomy anastomosis site.

Figure: A 18 mm X 149mm fully covered self expandable metallic stent (SEMS) was placed at Jejunojejunal anastomosis.
Disclosures:
Abdul Subhan Talpur indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Mustafa Sajjad Cheema indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Gegin George indicated no relevant financial relationships.
Abdelhamid Ben Selma indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Abdul Subhan Talpur, MD1, Fawad Talat, MD1, Muhammad Ahmed, MD1, Sadia Tabassum, MD2, Hammad Qadri, DO3, Usama Sakhawat, MD1, Khandokar A. Talib, MD3, Mustafa Sajjad Cheema, MBBS4, Ibrar Atiq, MD1, Gegin George, MD2, Abdelhamid Ben Selma, MD1, Toseef Javaid, MD1. P3566 - Severe Malnutrition and Diarrhea due to Gastrocolic Fistula Post-Roux-en-Y: Role of Endoscopic Stenting in Bridging to Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
