Monday Poster Session
Category: Interventional Endoscopy
P3565 - Swallowing the Consequences: Paraesophageal Pseudocyst Following Acute on Chronic Alcoholic Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sydney Lovrien, MD (she/her/hers)
University of South Dakota Sanford School of Medicine
Sioux Falls, SD
Presenting Author(s)
Amna Gill, MBBS1, Sydney Lovrien, MD1, Joseph Schowalter, DO2
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Avera McKennan Hospital & University Health Center, Sioux Falls, SD
Introduction: Pancreatic pseudocysts (PPCs) are localized collections of amylase rich fluid with non-epithelialized walls. PPCs are often asymptomatic but can present with abdominal pain, nausea or emesis. The following case depicts an atypical presentation of a PPC.
Case Description/
Methods: A 38-year-old male with a past medical history of well-controlled HIV, chronic pancreatitis, alcohol use disorder and gastric reflux with esophagitis presented with two days of sternal chest pain, dysphagia, and fever (Tmax: 100.8 ℉). Evaluation showed no leukocytosis, anemia (Hgb: 11.3g/dL) and lipase elevation (542U/L). CTA abdomen showed distal esophageal thickening with compression from a peripherally enhancing fluid collection arising near the pancreatic body (Figure 1) concerning for abscess vs PPC. His condition worsened despite conservative treatments (NPO, fluids, antimicrobials). Esophagogastroduodenoscopy (EGD) showed a patent lumen without perforation but evidence of extrinsic compression. Endoscopic ultrasound (EUS) confirmed a fluid collection surrounding the distal esophagus (Figure 2) that was tracked inferiorly terminating at the distal pancreatic body. Aspiration yielded 3 mL of fluid with resolution of the compression. Fluid studies showed proteinaceous debris with amylase >12,000 U/L consistent with PPC. Antibiotics were discontinued and he had complete resolution of his symptoms without recurrence at follow up one week later.
Discussion: Pancreatitis accounts for 200,000 hospitalizations annually in the US and PPCs develop in 14.6% and 41.8% of acute and acute-on-chronic pancreatitis cases, respectively. Hence, unusual PPC presentations with mediastinal extension and compression of surrounding structures with odynophagia, dyspnea, chest pain, or weight loss must be recognized. Contrast enhanced CT has a high sensitivity for detecting PPCs but may not demonstrate the tract to the pancreas. Medical management is usually supportive and includes bowel rest, nutritional support and somatostatin analogues but percutaneous or surgical drainage is employed if conservative measures fail. EUS can characterize the fluid collection as an abscess vs PPC, is less invasive than other routes, and is often the preferred approach. There is limited data available about successful transmural drainage of PPCs. This case adds to this data, where a transesophageal approach was used for complete aspiration of the PPC (without stenting due to risk of migration), resolution of symptoms and discharge in good health.
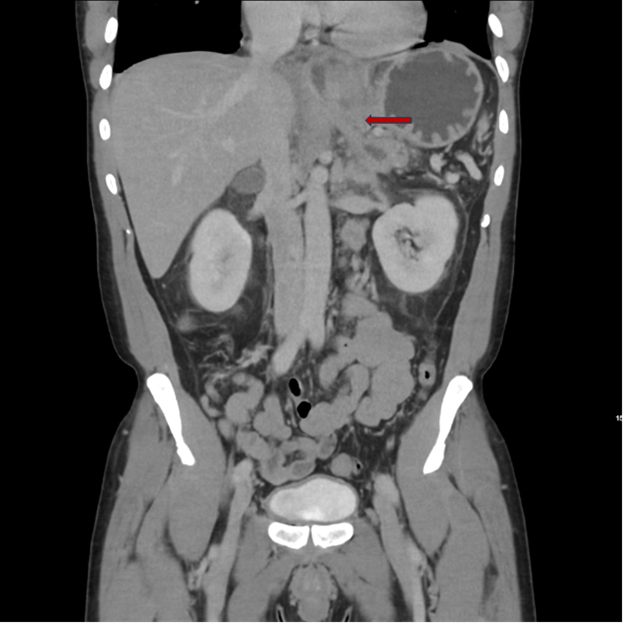
Figure: Figure 1: CTA abdomen/pelvis demonstrated increased stranding adjacent to the distal esophagus, a tubular 9mm diameter peripherally enhancing fluid collection partially surrounding the GE junction, and pancreatic stranding.

Figure: Figure 2: EUS visualization of PPC fluid accumulation (dimensions: 20.9mm x 8.6mm).
Disclosures:
Amna Gill indicated no relevant financial relationships.
Sydney Lovrien indicated no relevant financial relationships.
Joseph Schowalter indicated no relevant financial relationships.
Amna Gill, MBBS1, Sydney Lovrien, MD1, Joseph Schowalter, DO2. P3565 - Swallowing the Consequences: Paraesophageal Pseudocyst Following Acute on Chronic Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Avera McKennan Hospital & University Health Center, Sioux Falls, SD
Introduction: Pancreatic pseudocysts (PPCs) are localized collections of amylase rich fluid with non-epithelialized walls. PPCs are often asymptomatic but can present with abdominal pain, nausea or emesis. The following case depicts an atypical presentation of a PPC.
Case Description/
Methods: A 38-year-old male with a past medical history of well-controlled HIV, chronic pancreatitis, alcohol use disorder and gastric reflux with esophagitis presented with two days of sternal chest pain, dysphagia, and fever (Tmax: 100.8 ℉). Evaluation showed no leukocytosis, anemia (Hgb: 11.3g/dL) and lipase elevation (542U/L). CTA abdomen showed distal esophageal thickening with compression from a peripherally enhancing fluid collection arising near the pancreatic body (Figure 1) concerning for abscess vs PPC. His condition worsened despite conservative treatments (NPO, fluids, antimicrobials). Esophagogastroduodenoscopy (EGD) showed a patent lumen without perforation but evidence of extrinsic compression. Endoscopic ultrasound (EUS) confirmed a fluid collection surrounding the distal esophagus (Figure 2) that was tracked inferiorly terminating at the distal pancreatic body. Aspiration yielded 3 mL of fluid with resolution of the compression. Fluid studies showed proteinaceous debris with amylase >12,000 U/L consistent with PPC. Antibiotics were discontinued and he had complete resolution of his symptoms without recurrence at follow up one week later.
Discussion: Pancreatitis accounts for 200,000 hospitalizations annually in the US and PPCs develop in 14.6% and 41.8% of acute and acute-on-chronic pancreatitis cases, respectively. Hence, unusual PPC presentations with mediastinal extension and compression of surrounding structures with odynophagia, dyspnea, chest pain, or weight loss must be recognized. Contrast enhanced CT has a high sensitivity for detecting PPCs but may not demonstrate the tract to the pancreas. Medical management is usually supportive and includes bowel rest, nutritional support and somatostatin analogues but percutaneous or surgical drainage is employed if conservative measures fail. EUS can characterize the fluid collection as an abscess vs PPC, is less invasive than other routes, and is often the preferred approach. There is limited data available about successful transmural drainage of PPCs. This case adds to this data, where a transesophageal approach was used for complete aspiration of the PPC (without stenting due to risk of migration), resolution of symptoms and discharge in good health.
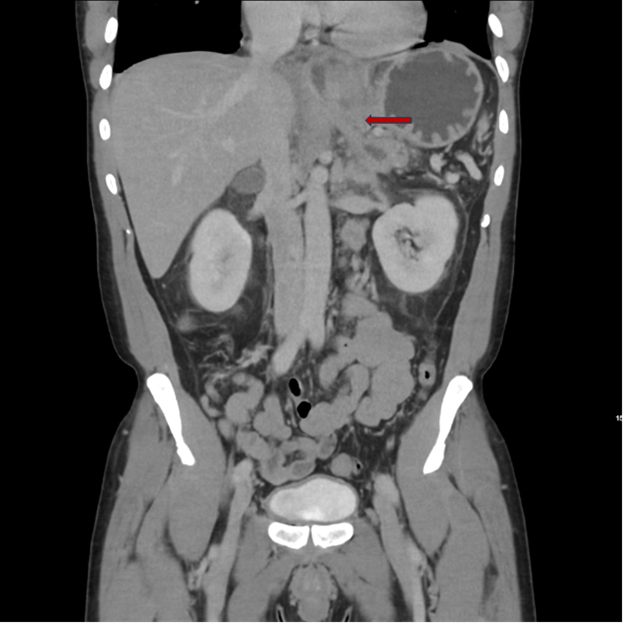
Figure: Figure 1: CTA abdomen/pelvis demonstrated increased stranding adjacent to the distal esophagus, a tubular 9mm diameter peripherally enhancing fluid collection partially surrounding the GE junction, and pancreatic stranding.

Figure: Figure 2: EUS visualization of PPC fluid accumulation (dimensions: 20.9mm x 8.6mm).
Disclosures:
Amna Gill indicated no relevant financial relationships.
Sydney Lovrien indicated no relevant financial relationships.
Joseph Schowalter indicated no relevant financial relationships.
Amna Gill, MBBS1, Sydney Lovrien, MD1, Joseph Schowalter, DO2. P3565 - Swallowing the Consequences: Paraesophageal Pseudocyst Following Acute on Chronic Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

