Monday Poster Session
Category: Interventional Endoscopy
P3538 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Choledocholithiasis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Dinuka Bandara, DO2, Anne Jarvis, MD1, Gautam Maddineni, MD3, Keng-Yu Chuang, MD4, Savio Reddymasu, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Florida State University, Cape Coral, FL; 4GI Alliance, Phoenix, AZ
Introduction: Acute choledocholithiasis (AC), the presence of gallstones in the common bile duct, often necessitates timely intervention to prevent complications such as cholangitis or pancreatitis. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) are the primary interventions for managing this condition. The timing of these procedures—whether performed early or late—can significantly impact patient outcomes, including the rates of complications, hospital length of stay, and readmission. This study aims to compare the clinical outcomes associated with early versus late ERCP and LCBDE in patients with AC, providing essential insights to guide clinical decision-making and improve patient care.
Methods: Hospitalization data were obtained from the Nationwide Readmissions Database, from 2016 to 2021 with a primary diagnosis of choledocholithiasis with cholangitis and underwent either ERCP or LCBDE. The primary outcome was all-cause 30-day readmission rates, with secondary outcomes including length of stay (LOS), total cost adjusted to 2021 dollars, and in-hospital mortality. ERCP patients were categorized by timing into urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP, while LCBDE patients were stratified similarly.
Results: This study analyzed 77,863 AC admissions. Of the cohort, 60.8% were ERCP-only patients and 39.2% underwent LCBDE. Results indicated that LCBDE patients were significantly younger (mean age 49.6 vs. 62.6 years, p< 0.001) and had a higher female representation (73.6% vs. 62.9%, p< 0.001). Furthermore, LCBDE patients experienced fewer complications, such as septic shock and severe sepsis (p< 0.001), and had a shorter mean LOS (3.28 vs. 3.97 days, p< 0.001) and lower 30-day readmission rates (7.67% vs. 12.0%, p< 0.001). ERCP timing analysis revealed 39.2% of patients received no ERCP, with significant increase in age in late ERCP recipients (mean age 66.7 years, p< 0.001). Complications were highest in late ERCP patients, who also had the longest LOS and highest costs. Similarly, late LCBDE patients exhibited increased LOS (5.87 days) compared to no LCBDE patients (3.97 days), and higher readmission (odds ratio: 1.41) compared to no LCBDE, p< 0.001).
Discussion: In summary, LCBDE was associated with younger patients, fewer complications, and shorter stays compared to ERCP. ERCP timing affected clinical outcomes, with late procedures correlating with increased complications and costs.
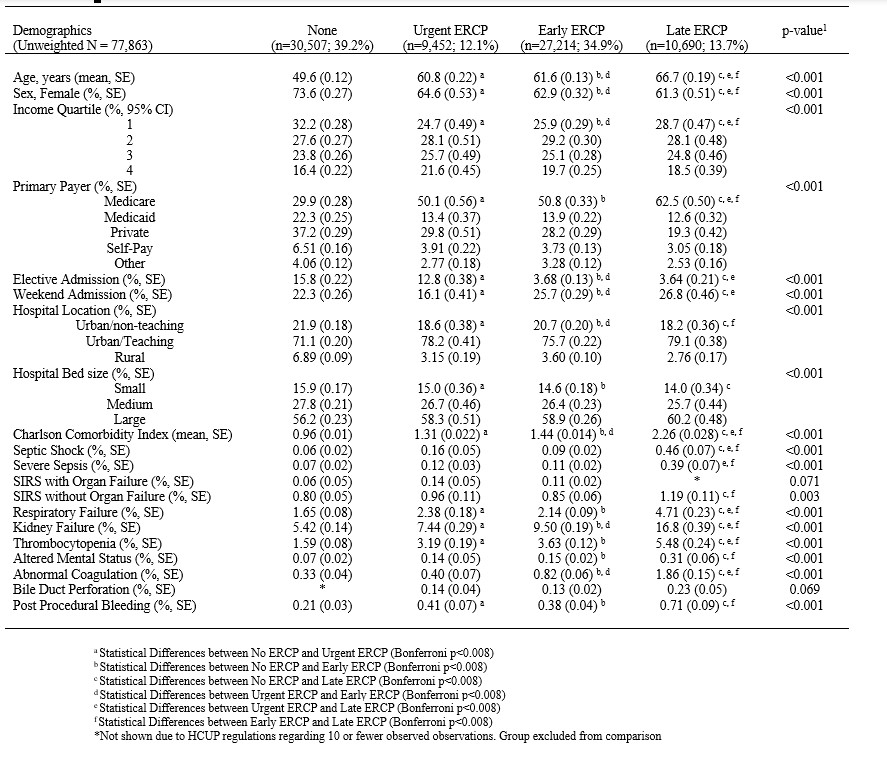
Figure: Table 1. Demographics and clinical characteristics by ECRP Timing
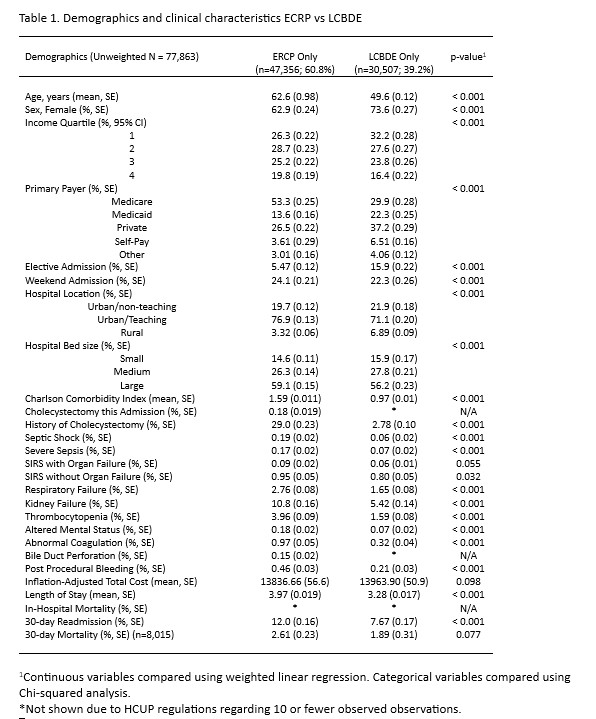
Figure: Table 2. Demographics and clinical characteristics ECRP vs LCBDE
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
Anne Jarvis indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, Anne Jarvis, MD1, Gautam Maddineni, MD3, Keng-Yu Chuang, MD4, Savio Reddymasu, MD1. P3538 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Choledocholithiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Florida State University, Cape Coral, FL; 4GI Alliance, Phoenix, AZ
Introduction: Acute choledocholithiasis (AC), the presence of gallstones in the common bile duct, often necessitates timely intervention to prevent complications such as cholangitis or pancreatitis. Endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) are the primary interventions for managing this condition. The timing of these procedures—whether performed early or late—can significantly impact patient outcomes, including the rates of complications, hospital length of stay, and readmission. This study aims to compare the clinical outcomes associated with early versus late ERCP and LCBDE in patients with AC, providing essential insights to guide clinical decision-making and improve patient care.
Methods: Hospitalization data were obtained from the Nationwide Readmissions Database, from 2016 to 2021 with a primary diagnosis of choledocholithiasis with cholangitis and underwent either ERCP or LCBDE. The primary outcome was all-cause 30-day readmission rates, with secondary outcomes including length of stay (LOS), total cost adjusted to 2021 dollars, and in-hospital mortality. ERCP patients were categorized by timing into urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP, while LCBDE patients were stratified similarly.
Results: This study analyzed 77,863 AC admissions. Of the cohort, 60.8% were ERCP-only patients and 39.2% underwent LCBDE. Results indicated that LCBDE patients were significantly younger (mean age 49.6 vs. 62.6 years, p< 0.001) and had a higher female representation (73.6% vs. 62.9%, p< 0.001). Furthermore, LCBDE patients experienced fewer complications, such as septic shock and severe sepsis (p< 0.001), and had a shorter mean LOS (3.28 vs. 3.97 days, p< 0.001) and lower 30-day readmission rates (7.67% vs. 12.0%, p< 0.001). ERCP timing analysis revealed 39.2% of patients received no ERCP, with significant increase in age in late ERCP recipients (mean age 66.7 years, p< 0.001). Complications were highest in late ERCP patients, who also had the longest LOS and highest costs. Similarly, late LCBDE patients exhibited increased LOS (5.87 days) compared to no LCBDE patients (3.97 days), and higher readmission (odds ratio: 1.41) compared to no LCBDE, p< 0.001).
Discussion: In summary, LCBDE was associated with younger patients, fewer complications, and shorter stays compared to ERCP. ERCP timing affected clinical outcomes, with late procedures correlating with increased complications and costs.
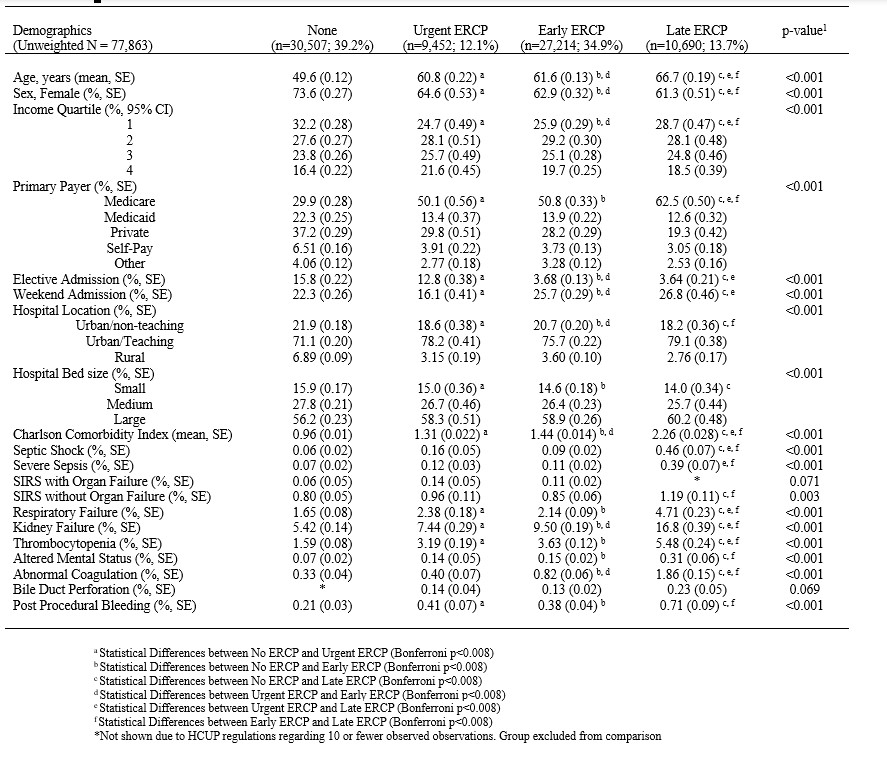
Figure: Table 1. Demographics and clinical characteristics by ECRP Timing
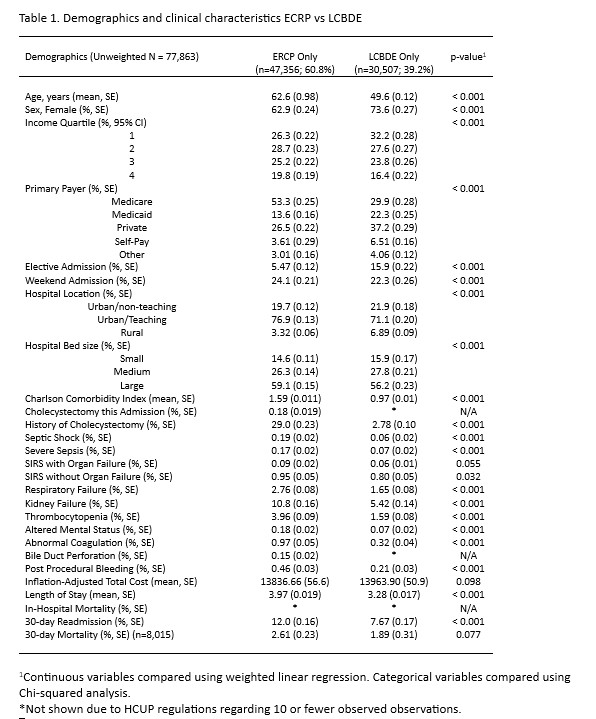
Figure: Table 2. Demographics and clinical characteristics ECRP vs LCBDE
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
Anne Jarvis indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, Anne Jarvis, MD1, Gautam Maddineni, MD3, Keng-Yu Chuang, MD4, Savio Reddymasu, MD1. P3538 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Choledocholithiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
