Monday Poster Session
Category: Infections and Microbiome
P3502 - Protein-Losing Enteropathy With Severe Hypoalbuminemia Associated With Fulminant Clostridiodes Difficile Colitis: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelrhman Refaey, MD
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences
Teaneck, NJ
Presenting Author(s)
Abdelrhman Refaey, MD1, Simran Gupta, MD1, Katherine Rangoussis, BS, MS2, Marie L. Borum, MD, EdD, MPH, FACG1
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Clostridium difficile infection (CDI), one of the most common healthcare-associated infections, can be associated with significant morbidity and mortality, especially in older hospitalized patients. Manifestations range from asymptomatic carriage to fulminant disease with toxic megacolon. An unusual, but severe complication, is protein-losing enteropathy (PLE). We describe a case of fulminant CDI complicated by PLE with severe hypoalbuminemia, bilateral pleural effusions, pericardial effusion, and anasarca.
Case Description/
Methods: A 70-year-old woman with previous antibiotic exposure for Rocky Mountain Spotted Fever presented with 10 days of diarrhea up to 30 times daily and abdominal pain. On admission, she was hypotensive (72/55 mmHg), tachypneic, and tachycardic. Labs revealed a leukocytosis (WBC 29.8), anemia (Hb 11.2), hyponatremia (125 mmol/L), and hypoalbuminemia (1.9 g/dL). An abdominal/pelvic CT scan revealed pancolitis and small left-sided pleural effusion. Stool assay confirmed CDI. She was treated with vancomycin and metronidazole, then fidaxomicin. She was discharged in stable condition. She was readmitted 2 weeks later with bloody diarrhea and severe hypotension, requiring ICU management. She was transferred for continued care. Following transfer, labs revealed worsening leukocytosis (WBC 32.3), lactic acidosis (9.2 mmol/L), and critically low albumin level ( < 1g/dL). A CT scan revealed worsening pancolitis, bilateral pleural effusions, pericardial effusion, and anasarca consistent with PLE. Stool assay confirmed persistent/recurrent CDI. Endoscopic procedures could not be performed due to clinical instability. Despite aggressive antibiotic therapy with consideration for fecal microbiota transplantation (FMT), she developed multiple complications, including acute renal injury, transfusion-requiring anemia, ileus, and respiratory failure necessitating intubation, ultimately succumbing to clinical deterioration.
Discussion: This is a rare case of severe CDI complicated by PLE and critical hypoalbuminemia. Albumin is a prognostic marker for CDI; critically low levels highlight the extreme severity of PLE. This is the first reported case of CDI with albumin < 1 g/dL. While FMT is a potential treatment for CDI, the fulminant course and rapid deterioration did not allow for this intervention. This case underscores the importance of judicious antibiotic use, early recognition of PLE in CDI patients, and the need for aggressive disease management, especially in elderly patients.
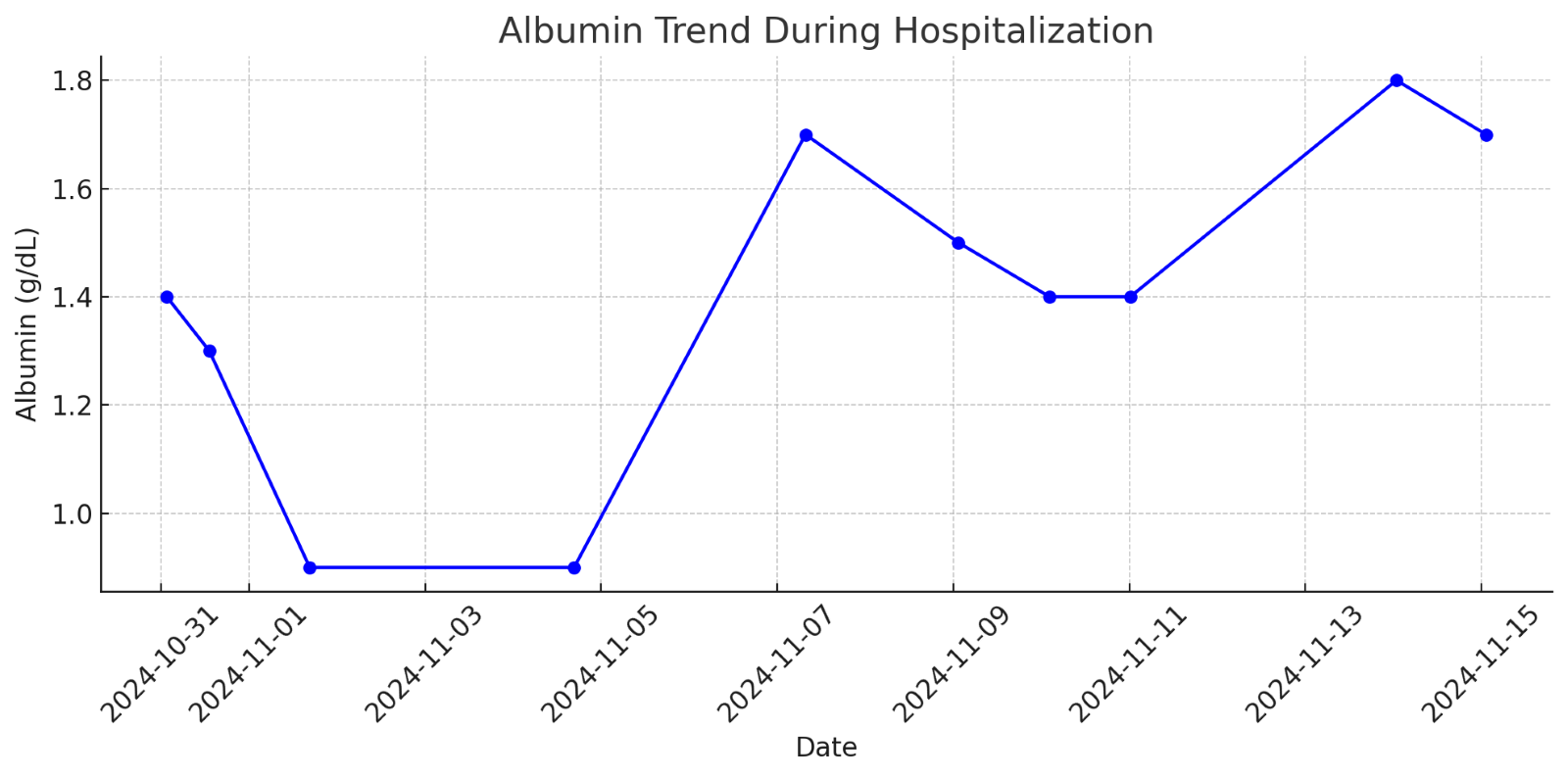
Figure: A graph showing the trend of serum albumin levels during hospitalization
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Simran Gupta indicated no relevant financial relationships.
Katherine Rangoussis indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Simran Gupta, MD1, Katherine Rangoussis, BS, MS2, Marie L. Borum, MD, EdD, MPH, FACG1. P3502 - Protein-Losing Enteropathy With Severe Hypoalbuminemia Associated With Fulminant Clostridiodes Difficile Colitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Clostridium difficile infection (CDI), one of the most common healthcare-associated infections, can be associated with significant morbidity and mortality, especially in older hospitalized patients. Manifestations range from asymptomatic carriage to fulminant disease with toxic megacolon. An unusual, but severe complication, is protein-losing enteropathy (PLE). We describe a case of fulminant CDI complicated by PLE with severe hypoalbuminemia, bilateral pleural effusions, pericardial effusion, and anasarca.
Case Description/
Methods: A 70-year-old woman with previous antibiotic exposure for Rocky Mountain Spotted Fever presented with 10 days of diarrhea up to 30 times daily and abdominal pain. On admission, she was hypotensive (72/55 mmHg), tachypneic, and tachycardic. Labs revealed a leukocytosis (WBC 29.8), anemia (Hb 11.2), hyponatremia (125 mmol/L), and hypoalbuminemia (1.9 g/dL). An abdominal/pelvic CT scan revealed pancolitis and small left-sided pleural effusion. Stool assay confirmed CDI. She was treated with vancomycin and metronidazole, then fidaxomicin. She was discharged in stable condition. She was readmitted 2 weeks later with bloody diarrhea and severe hypotension, requiring ICU management. She was transferred for continued care. Following transfer, labs revealed worsening leukocytosis (WBC 32.3), lactic acidosis (9.2 mmol/L), and critically low albumin level ( < 1g/dL). A CT scan revealed worsening pancolitis, bilateral pleural effusions, pericardial effusion, and anasarca consistent with PLE. Stool assay confirmed persistent/recurrent CDI. Endoscopic procedures could not be performed due to clinical instability. Despite aggressive antibiotic therapy with consideration for fecal microbiota transplantation (FMT), she developed multiple complications, including acute renal injury, transfusion-requiring anemia, ileus, and respiratory failure necessitating intubation, ultimately succumbing to clinical deterioration.
Discussion: This is a rare case of severe CDI complicated by PLE and critical hypoalbuminemia. Albumin is a prognostic marker for CDI; critically low levels highlight the extreme severity of PLE. This is the first reported case of CDI with albumin < 1 g/dL. While FMT is a potential treatment for CDI, the fulminant course and rapid deterioration did not allow for this intervention. This case underscores the importance of judicious antibiotic use, early recognition of PLE in CDI patients, and the need for aggressive disease management, especially in elderly patients.
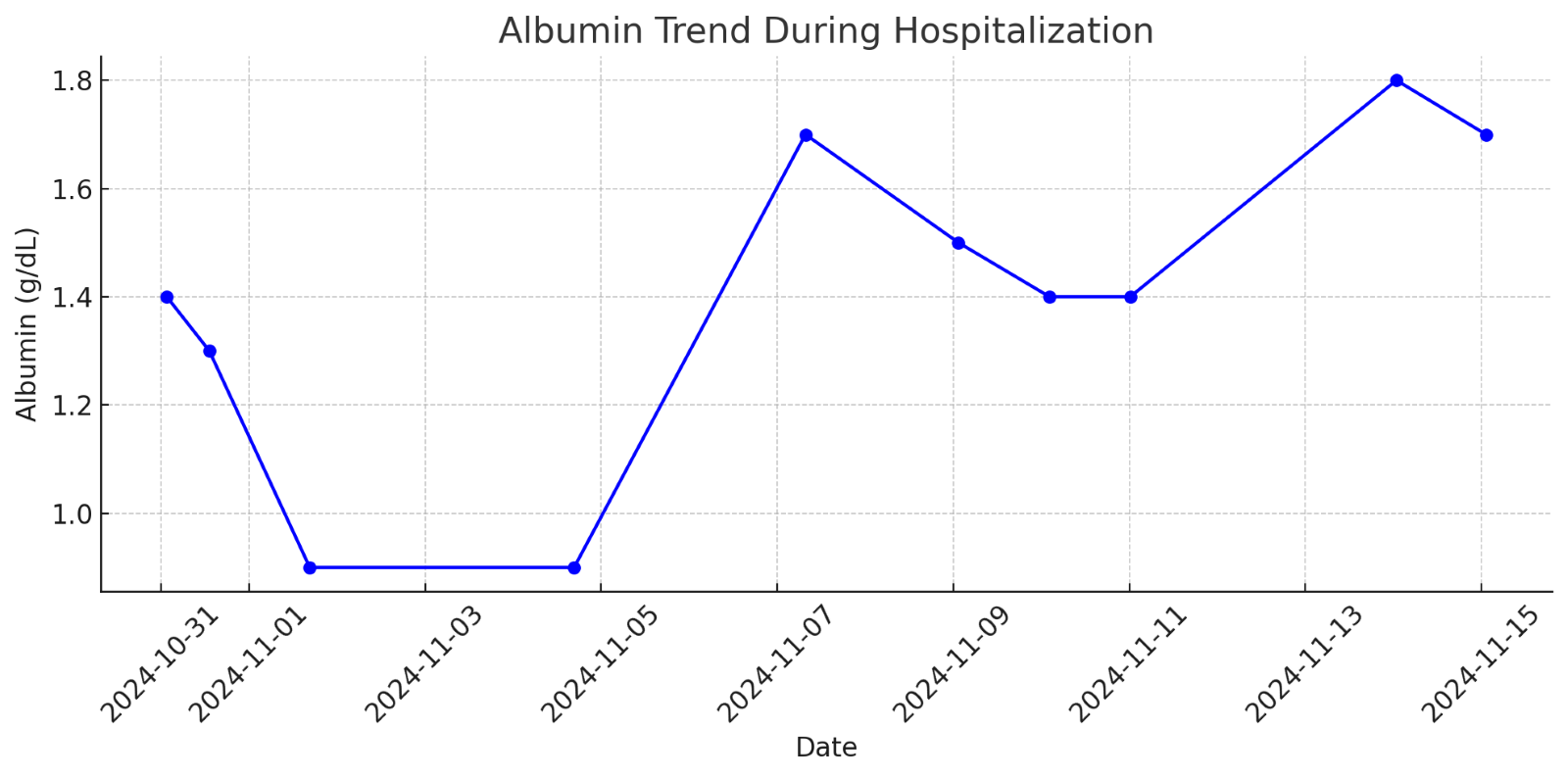
Figure: A graph showing the trend of serum albumin levels during hospitalization
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Simran Gupta indicated no relevant financial relationships.
Katherine Rangoussis indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Simran Gupta, MD1, Katherine Rangoussis, BS, MS2, Marie L. Borum, MD, EdD, MPH, FACG1. P3502 - Protein-Losing Enteropathy With Severe Hypoalbuminemia Associated With Fulminant Clostridiodes Difficile Colitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
