Monday Poster Session
Category: Infections and Microbiome
P3500 - A Diagnostic Dilemma: Fulminant EBV Colitis Masquerading as Ulcerative Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Amir Harb, DO1, Nouman Shafique, MD1, Mahmoud Aldyab, MD2, Tasnuva Mahmud, MD1
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Pathology, AdventHealth Orlando, Orlando, FL
Introduction: Epstein-Barr virus (EBV) infection with gastrointestinal (GI) tract involvement is rare. Its clinical and histological features can mimic other etiologies. Here, we present a case of a 31-year-old male, initially suspected to have inflammatory bowel disease (IBD), later confirmed to have EBV colitis.
Case Description/
Methods: A 31-year-old male with congenital HIV infection and poor compliance to antiretroviral therapy (ART) presented with abdominal pain, hematochezia and unintentional weight loss for the past 2 months. Physical exam revealed diffuse abdominal tenderness. Laboratory tests showed leukocytosis, microcytic anemia, a CD4 count of 54 cells/uL, and an HIV viral load of 637,000 copies/mL. PCR stool studies for common bacteria and viruses were negative.
Colonoscopy showed mucosal erythema and loss of vascular markings. Mesalamine and steroids were started, but his symptoms worsened and abdominal computed tomography (CT) showed severe pancolitis with diffuse colonic distention. Repeat colonoscopy for decompression tube placement showed severely punched out, ulcerated mucosa. After decompression, his symptoms improved briefly before he developed intractable vomiting. Repeat CT revealed pneumoperitoneum (Figure 1). Emergent exploratory laparotomy showed toxic colitis with transverse colon perforation, requiring a total abdominal colectomy with end ileostomy. Pathological examination revealed neutrophilic infiltrate in the lamina propria and mild-moderate chronic inflammatory infiltrate without crypt architectural distortion or crypt abscesses. EBV RNA was by in situ hybridization (Figure 2). Next-generation-sequencing and PCR of colonic tissue showed normal GI flora. The patient had an uneventful post-operative course with symptom resolution. He was discharged on ART with infectious diseases outpatient follow up.
.
Discussion: EBV is often implicated in self-limiting mononucleosis. It can also be associated with GI lymphoma, but involvement in the tract without overt lymphoma is rare, with only a few cases reported in the literature. GI-tract EBV infections can present as diarrhea, hematochezia, and abdominal pain, resembling IBD. However, fulminant colitis resulting in perforation and colectomy is highly unusual. Dense inflammatory infiltrates in the lamina propria and positive immunohistochemical staining differentiate it from other causes. It is crucial to consider EBV when evaluating severe colitis of unknown origin, especially in the setting of immune compromise, like in our patient.
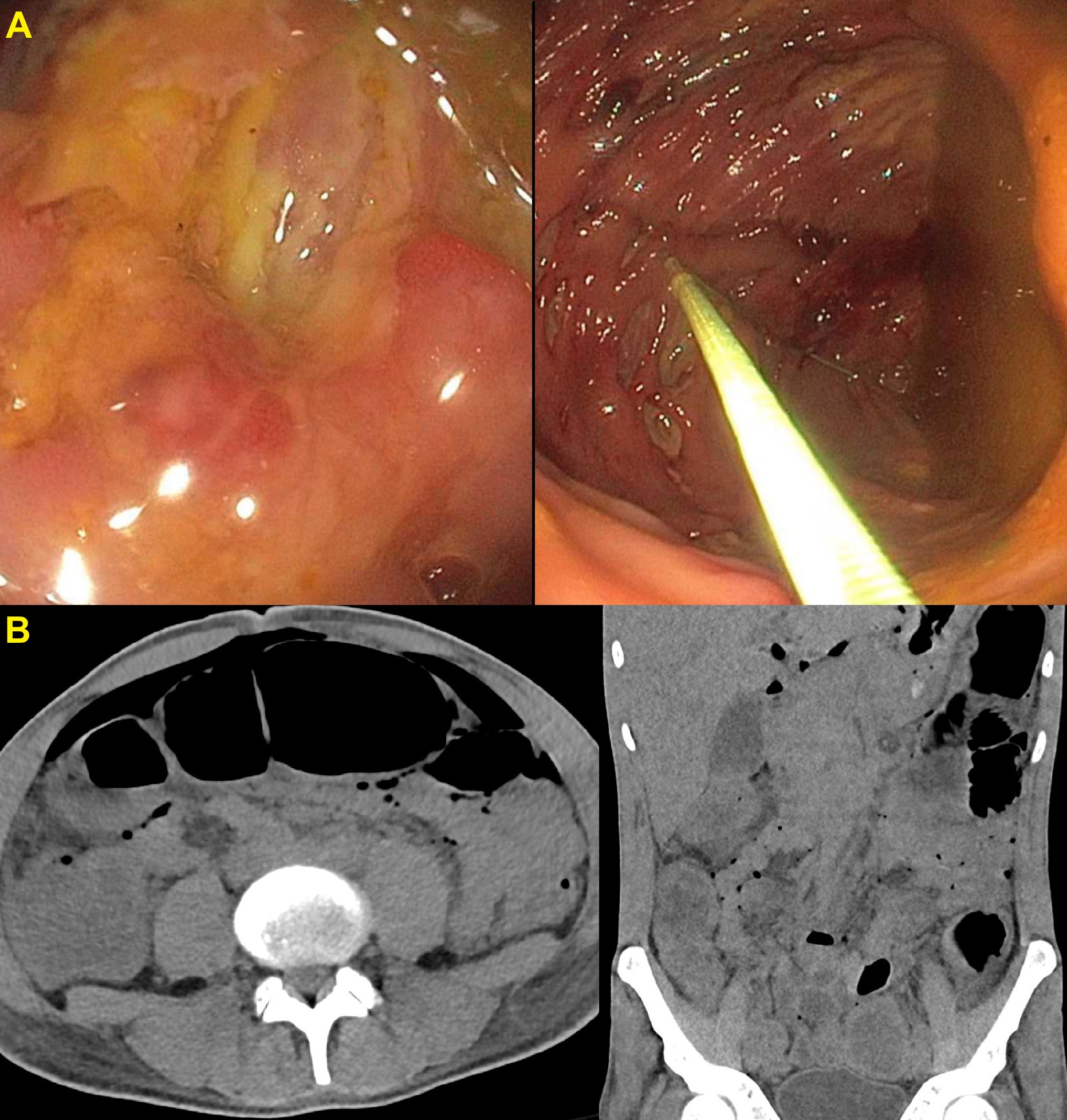
Figure: Figure 1.
A – Colonoscopy showing severely punched out, ulcerated mucosa. B – Abdominal CT scan showing colonic distension with pneumoperitoneum
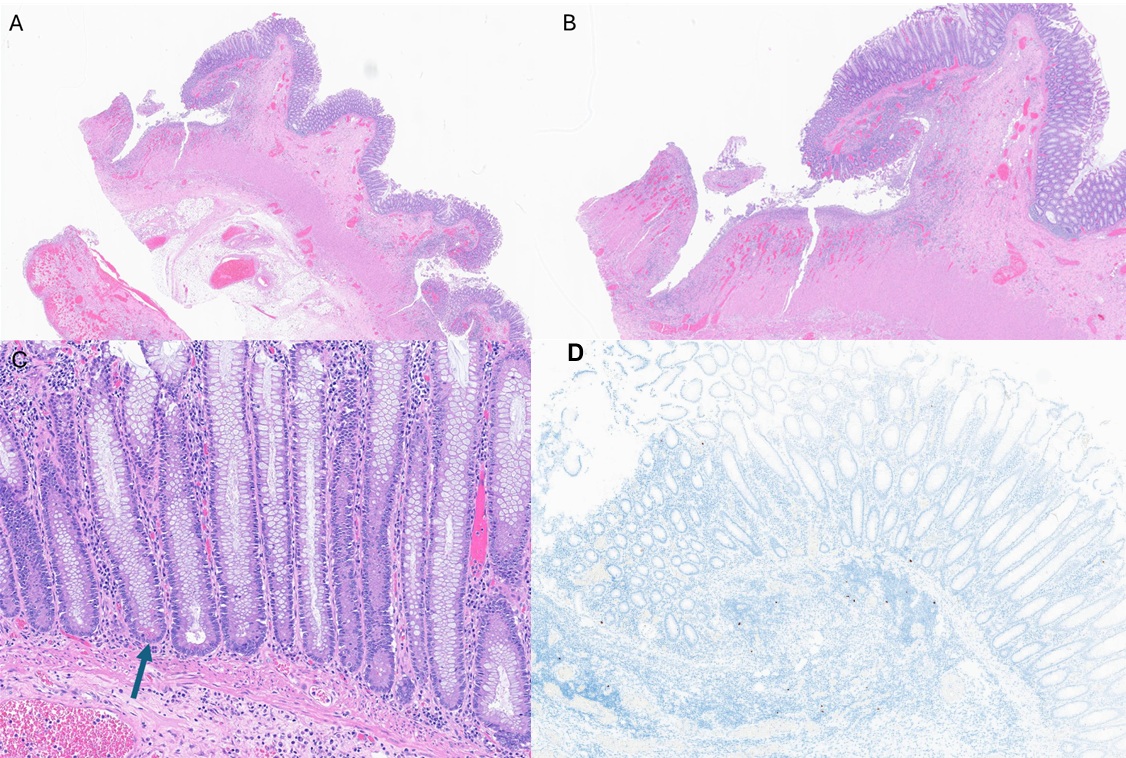
Figure: A & B - Section of colonic tissue with preserved crypts architecture and ulceration extending to muscularis propria. No granulomas identified
C - Paneth cell metaplasia identified in bases of crypts (arrow).
D - Epstein-Barr virus (EBV)-encoded RNA (EBER) by in situ hybridization: scattered small cells with expression of EBV RNA
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Amir Harb indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Mahmoud Aldyab indicated no relevant financial relationships.
Tasnuva Mahmud indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Amir Harb, DO1, Nouman Shafique, MD1, Mahmoud Aldyab, MD2, Tasnuva Mahmud, MD1. P3500 - A Diagnostic Dilemma: Fulminant EBV Colitis Masquerading as Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Pathology, AdventHealth Orlando, Orlando, FL
Introduction: Epstein-Barr virus (EBV) infection with gastrointestinal (GI) tract involvement is rare. Its clinical and histological features can mimic other etiologies. Here, we present a case of a 31-year-old male, initially suspected to have inflammatory bowel disease (IBD), later confirmed to have EBV colitis.
Case Description/
Methods: A 31-year-old male with congenital HIV infection and poor compliance to antiretroviral therapy (ART) presented with abdominal pain, hematochezia and unintentional weight loss for the past 2 months. Physical exam revealed diffuse abdominal tenderness. Laboratory tests showed leukocytosis, microcytic anemia, a CD4 count of 54 cells/uL, and an HIV viral load of 637,000 copies/mL. PCR stool studies for common bacteria and viruses were negative.
Colonoscopy showed mucosal erythema and loss of vascular markings. Mesalamine and steroids were started, but his symptoms worsened and abdominal computed tomography (CT) showed severe pancolitis with diffuse colonic distention. Repeat colonoscopy for decompression tube placement showed severely punched out, ulcerated mucosa. After decompression, his symptoms improved briefly before he developed intractable vomiting. Repeat CT revealed pneumoperitoneum (Figure 1). Emergent exploratory laparotomy showed toxic colitis with transverse colon perforation, requiring a total abdominal colectomy with end ileostomy. Pathological examination revealed neutrophilic infiltrate in the lamina propria and mild-moderate chronic inflammatory infiltrate without crypt architectural distortion or crypt abscesses. EBV RNA was by in situ hybridization (Figure 2). Next-generation-sequencing and PCR of colonic tissue showed normal GI flora. The patient had an uneventful post-operative course with symptom resolution. He was discharged on ART with infectious diseases outpatient follow up.
.
Discussion: EBV is often implicated in self-limiting mononucleosis. It can also be associated with GI lymphoma, but involvement in the tract without overt lymphoma is rare, with only a few cases reported in the literature. GI-tract EBV infections can present as diarrhea, hematochezia, and abdominal pain, resembling IBD. However, fulminant colitis resulting in perforation and colectomy is highly unusual. Dense inflammatory infiltrates in the lamina propria and positive immunohistochemical staining differentiate it from other causes. It is crucial to consider EBV when evaluating severe colitis of unknown origin, especially in the setting of immune compromise, like in our patient.
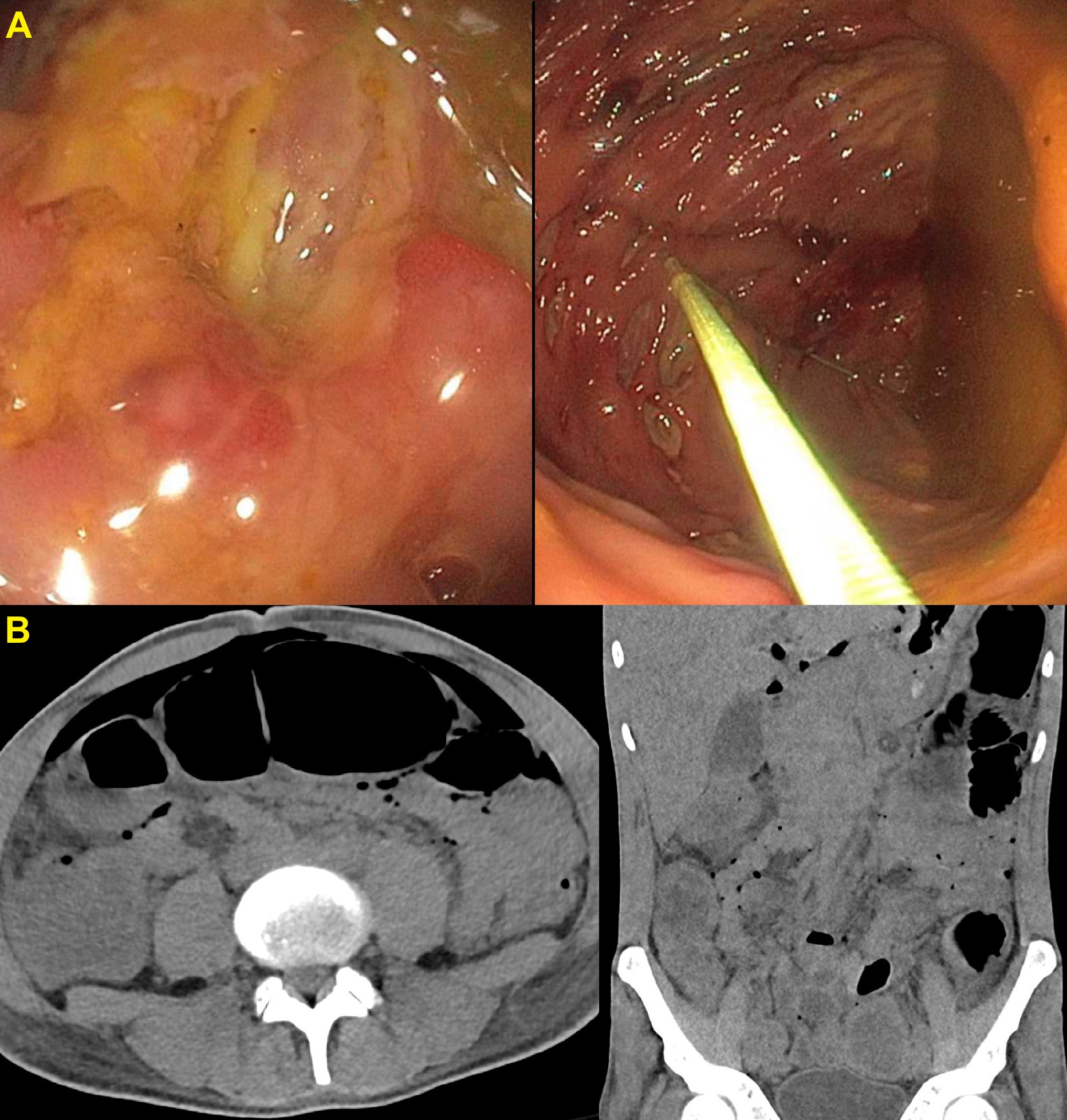
Figure: Figure 1.
A – Colonoscopy showing severely punched out, ulcerated mucosa. B – Abdominal CT scan showing colonic distension with pneumoperitoneum
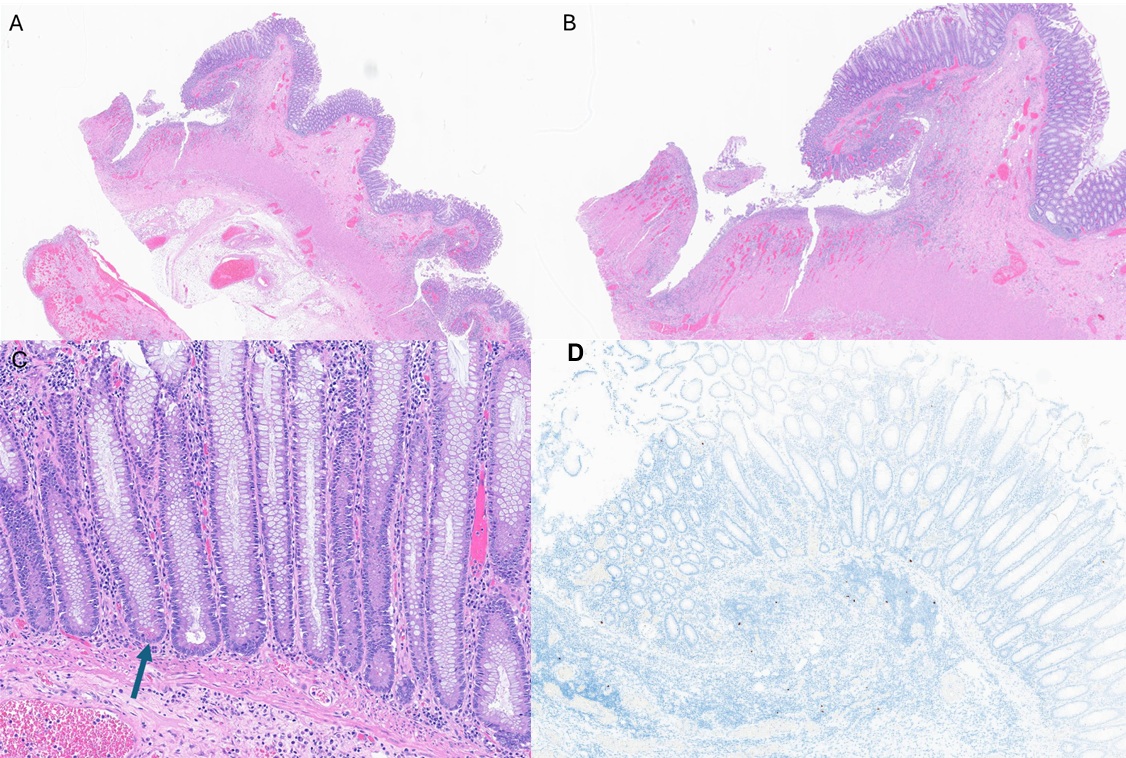
Figure: A & B - Section of colonic tissue with preserved crypts architecture and ulceration extending to muscularis propria. No granulomas identified
C - Paneth cell metaplasia identified in bases of crypts (arrow).
D - Epstein-Barr virus (EBV)-encoded RNA (EBER) by in situ hybridization: scattered small cells with expression of EBV RNA
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Amir Harb indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Mahmoud Aldyab indicated no relevant financial relationships.
Tasnuva Mahmud indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Amir Harb, DO1, Nouman Shafique, MD1, Mahmoud Aldyab, MD2, Tasnuva Mahmud, MD1. P3500 - A Diagnostic Dilemma: Fulminant EBV Colitis Masquerading as Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
