Monday Poster Session
Category: Infections and Microbiome
P3499 - Gastrointestinal Basidiobolomycosis Presenting as Pancreatic Head Mass and Multifocal Colitis and Complicated by Colonic Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FK
Fred Karaisz, MD (he/him/his)
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Award: ACG Presidential Poster Award
Kenneth Kalikasingh, BA, MS, Akul Yajnik, MD, Fred Karaisz, MD, Adeeti Chiplunker, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Gastrointestinal basidiobolomycosis is a rare, potentially fatal infection caused by Basidiobolus ranarum, often presenting insidiously with non-specific symptoms. We report a case of a 50-year-old man with extensive abdominal involvement and perforation, successfully managed with antifungals and a diverting loop ileostomy.
Case Description/
Methods: A 50-year-old man with type II diabetes mellitus presented with progressive left-sided abdominal pain, night sweats, 20-lb weight loss, and altered bowel habits over 1 month while traveling in Tanzania. Computed tomography (CT) revealed a right upper quadrant mass involving the pancreatic head, distal stomach, duodenum, and hepatic flexure of the colon. Flexible sigmoidoscopy identified a suspicious mass in the transverse colon; biopsies demonstrated nonspecific ulceration.
A week later, the patient developed peritonitis, and CT showed a contained perforation at the transverse colon. Exploratory laparotomy revealed pan-colonic wall thickening with dense adhesions fixing the duodenum and pancreas to the hepatic flexure, along with a necrotic focus and perforation of the posterior transverse colon. The patient was managed with surgical drainage, a diverting loop ileostomy, and total parenteral nutrition. Surgical pathology of peri-colonic fat and omentum revealed fungal infection, and the patient was started on IV amphotericin and transitioned to voriconazole. Polymerase chain reaction (PCR) of the surgical specimen confirmed basidiobolomycosis. His postoperative course was complicated by duodenal bulb necrosis and fistula, and he gradually recovered and was discharged to a long-term care facility.
Discussion: Basidiobolus ranarum is a broad, thin-walled filamentous fungus historically linked to subcutaneous infections, but has emerged as a rare cause of gastrointestinal basidiobolomycosis. Fewer than 102 cases have been reported globally, including ~25 in the United States. Infection is presumed to occur via ingestion of food contaminated with fungal spores, which germinate and form a Spitzenkörper that facilitates polarized hyphal growth and host tissue invasion. The disease primarily affects immunocompetent individuals and often mimics malignancy or inflammatory bowel disease due to mass-like lesions and bowel wall thickening. This case underscores the importance of recognizing the variable presentation of gastrointestinal basidiobolomycosis and highlights successful surgical and antifungal management without colonic resection.
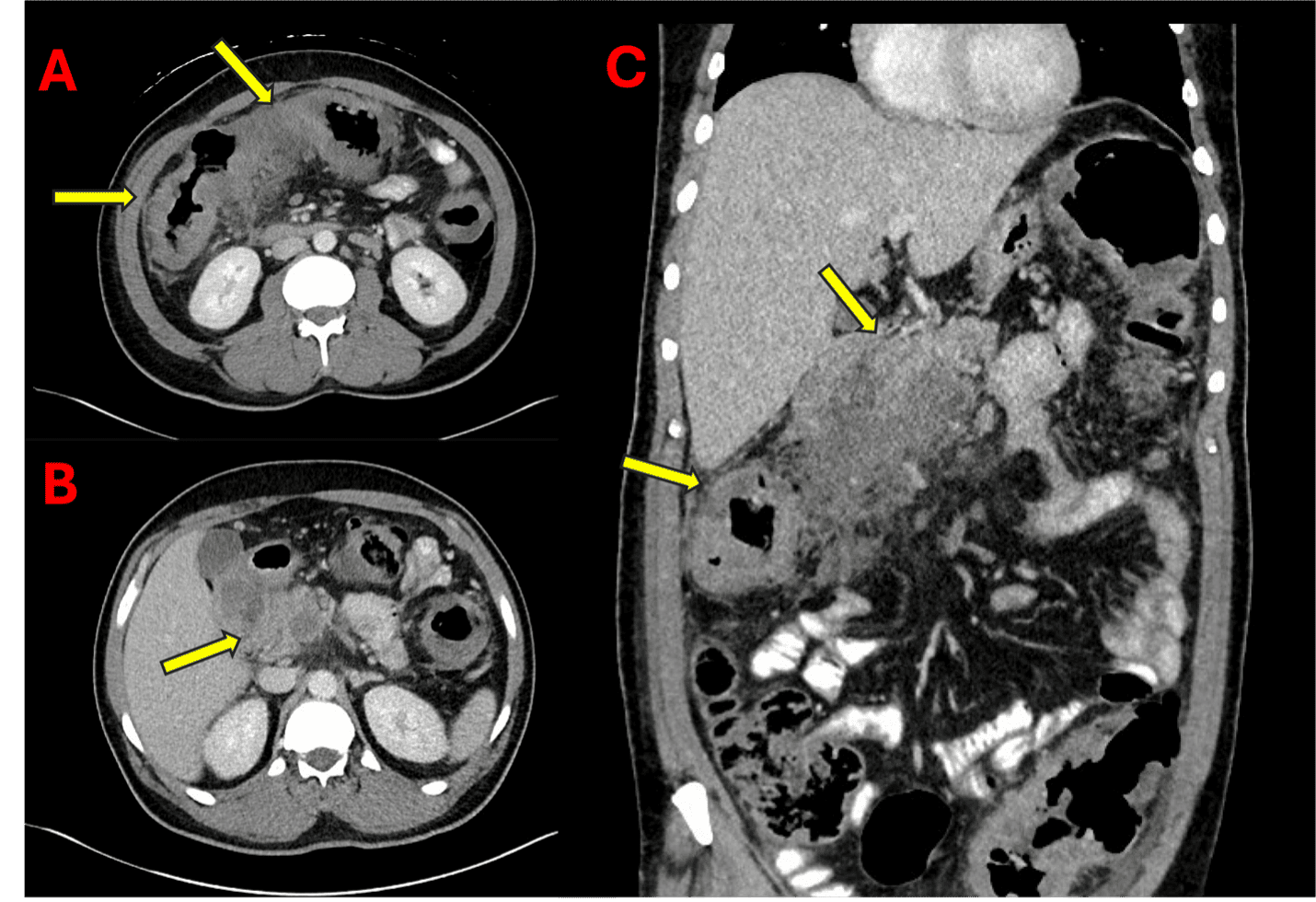
Figure: Figure 1. Computed tomography (CT) images of the patient’s gastrointestinal basidiobolomycosis. Cross-sectional images at the level of the transverse colon (A) and duodenum (B) demonstrate bowel wall thickening (yellow arrows), and a coronal view (C) shows a right upper quadrant mass involving the head of the pancreas, duodenum, and hepatic flexure of the colon (yellow arrows).
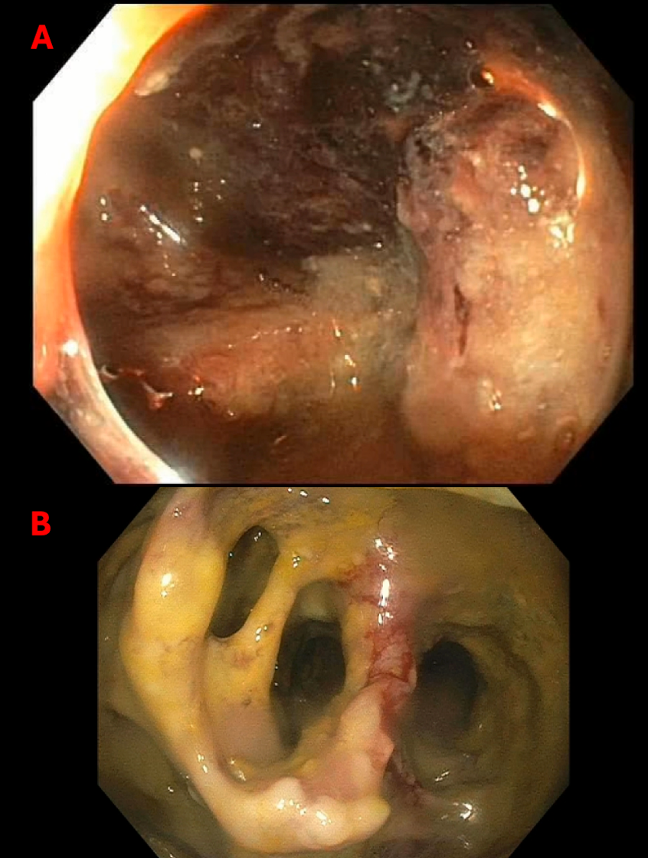
Figure: Figure 2. Endoscopic images of the gastrointestinal basidiobolomycosis. Esophagogastroduodenoscopy (EGD) images of the duodenal bulb (A) demonstrate duodenitis with fistula formation. Flexible sigmoidoscopy images of the transverse colon (B) revealed inflammatory tissue with colonic dilation.
Disclosures:
Kenneth Kalikasingh indicated no relevant financial relationships.
Akul Yajnik indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Adeeti Chiplunker: Ironwood Pharmaceuticals – Advisory Committee/Board Member.
Kenneth Kalikasingh, BA, MS, Akul Yajnik, MD, Fred Karaisz, MD, Adeeti Chiplunker, MD. P3499 - Gastrointestinal Basidiobolomycosis Presenting as Pancreatic Head Mass and Multifocal Colitis and Complicated by Colonic Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kenneth Kalikasingh, BA, MS, Akul Yajnik, MD, Fred Karaisz, MD, Adeeti Chiplunker, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Gastrointestinal basidiobolomycosis is a rare, potentially fatal infection caused by Basidiobolus ranarum, often presenting insidiously with non-specific symptoms. We report a case of a 50-year-old man with extensive abdominal involvement and perforation, successfully managed with antifungals and a diverting loop ileostomy.
Case Description/
Methods: A 50-year-old man with type II diabetes mellitus presented with progressive left-sided abdominal pain, night sweats, 20-lb weight loss, and altered bowel habits over 1 month while traveling in Tanzania. Computed tomography (CT) revealed a right upper quadrant mass involving the pancreatic head, distal stomach, duodenum, and hepatic flexure of the colon. Flexible sigmoidoscopy identified a suspicious mass in the transverse colon; biopsies demonstrated nonspecific ulceration.
A week later, the patient developed peritonitis, and CT showed a contained perforation at the transverse colon. Exploratory laparotomy revealed pan-colonic wall thickening with dense adhesions fixing the duodenum and pancreas to the hepatic flexure, along with a necrotic focus and perforation of the posterior transverse colon. The patient was managed with surgical drainage, a diverting loop ileostomy, and total parenteral nutrition. Surgical pathology of peri-colonic fat and omentum revealed fungal infection, and the patient was started on IV amphotericin and transitioned to voriconazole. Polymerase chain reaction (PCR) of the surgical specimen confirmed basidiobolomycosis. His postoperative course was complicated by duodenal bulb necrosis and fistula, and he gradually recovered and was discharged to a long-term care facility.
Discussion: Basidiobolus ranarum is a broad, thin-walled filamentous fungus historically linked to subcutaneous infections, but has emerged as a rare cause of gastrointestinal basidiobolomycosis. Fewer than 102 cases have been reported globally, including ~25 in the United States. Infection is presumed to occur via ingestion of food contaminated with fungal spores, which germinate and form a Spitzenkörper that facilitates polarized hyphal growth and host tissue invasion. The disease primarily affects immunocompetent individuals and often mimics malignancy or inflammatory bowel disease due to mass-like lesions and bowel wall thickening. This case underscores the importance of recognizing the variable presentation of gastrointestinal basidiobolomycosis and highlights successful surgical and antifungal management without colonic resection.
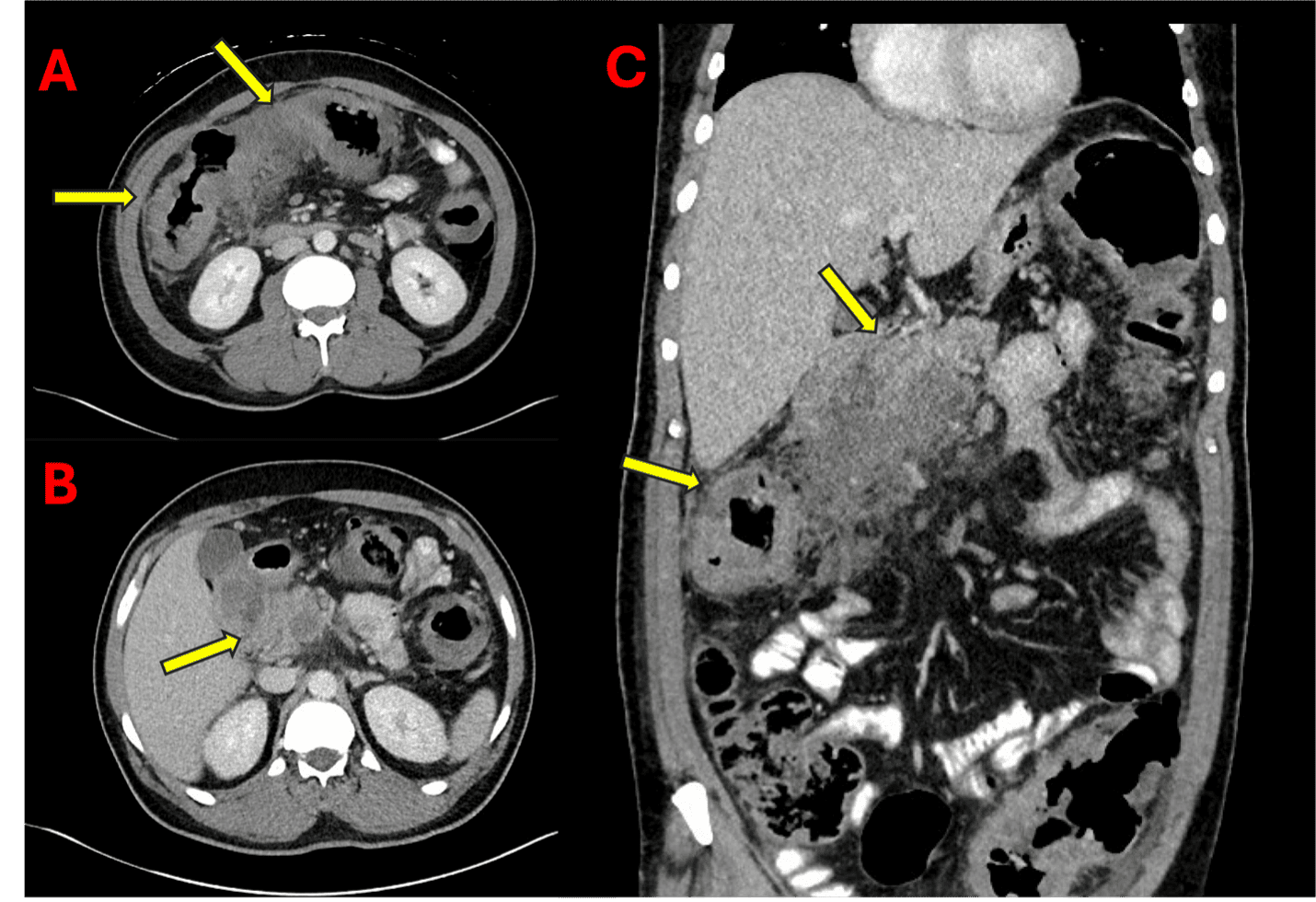
Figure: Figure 1. Computed tomography (CT) images of the patient’s gastrointestinal basidiobolomycosis. Cross-sectional images at the level of the transverse colon (A) and duodenum (B) demonstrate bowel wall thickening (yellow arrows), and a coronal view (C) shows a right upper quadrant mass involving the head of the pancreas, duodenum, and hepatic flexure of the colon (yellow arrows).
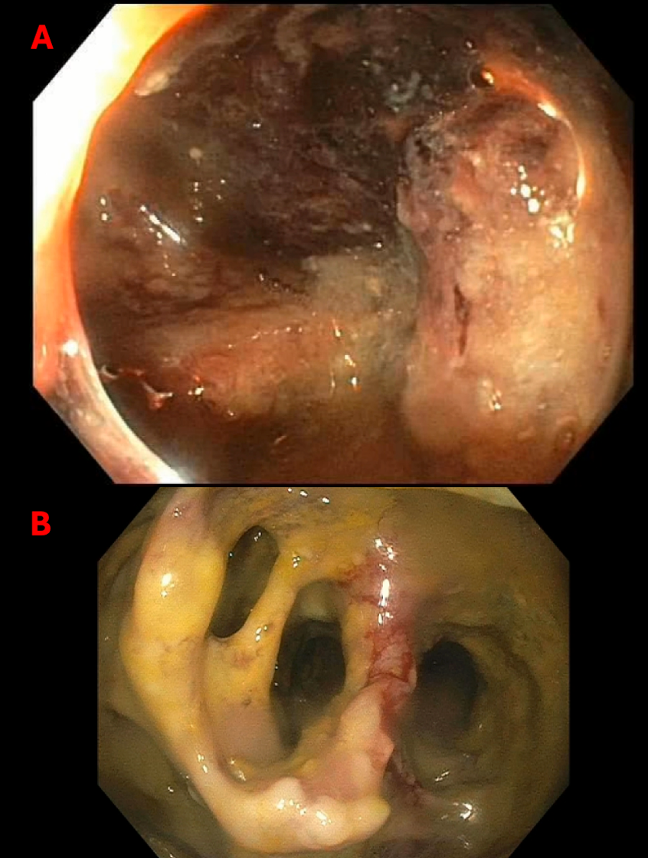
Figure: Figure 2. Endoscopic images of the gastrointestinal basidiobolomycosis. Esophagogastroduodenoscopy (EGD) images of the duodenal bulb (A) demonstrate duodenitis with fistula formation. Flexible sigmoidoscopy images of the transverse colon (B) revealed inflammatory tissue with colonic dilation.
Disclosures:
Kenneth Kalikasingh indicated no relevant financial relationships.
Akul Yajnik indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Adeeti Chiplunker: Ironwood Pharmaceuticals – Advisory Committee/Board Member.
Kenneth Kalikasingh, BA, MS, Akul Yajnik, MD, Fred Karaisz, MD, Adeeti Chiplunker, MD. P3499 - Gastrointestinal Basidiobolomycosis Presenting as Pancreatic Head Mass and Multifocal Colitis and Complicated by Colonic Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

