Monday Poster Session
Category: Infections and Microbiome
P3498 - Beyond Colonization: A Rare Case of Invasive Gastric Candidiasis Without Traditional Risk Factors
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sevag Hamamah, DO
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Garrett Teskey, DO1, Wesley Chow, MD2, Sevag Hamamah, DO2, Steven Gauerke, MD2, Faizi Hai, MD2
1Scripps Mercy Hospital, Yorba Linda, CA; 2Scripps Mercy Hospital, San Diego, CA
Introduction: Gastric candidiasis is a rare fungal infection of the stomach that typically arises with immunosuppression, critical illness, or mucosal disruption. Symptoms such as abdominal pain, nausea, vomiting, or gastrointestinal bleeding are nonspecific. We report a case of an 89-year-old immunocompetent male presenting with acute upper gastrointestinal bleeding, in whom gastric ulcers were found to be due to candidiasis on biopsy.
Case Description/
Methods: An 89-year-old male with diabetes, hypertension, and iron deficiency anemia presented with two syncopal episodes, coffee-ground emesis, melena, and abdominal pain. He denied prior NSAID use. One month earlier, he underwent cholecystectomy for gangrenous cholecystitis; no cultures were obtained. On examination, he was hypertensive with conjunctival pallor, dry mucous membranes, and mild diffuse abdominal tenderness. Labs showed leukocytosis of 22.3, normocytic anemia of 8.9, and elevated inflammatory markers. HIV was negative. Abdominal CT revealed ascending colon wall thickening. Blood cultures grew ESBL-producing E. coli, and stool was positive for C. diff. He was treated with meropenem and oral vancomycin. Upper endoscopy showed multiple large deep cratered gastric ulcers with dark adherent material on both curvatures and normal esophagus and duodenum. Biopsies revealed marked chronic active gastritis with ulceration, intestinal metaplasia, and necroinflammatory debris with abundant fungal pseudohyphae on PAS staining. Gastrin, chromogranin, H. pylori, CMV, and AFB stains were negative. Fluconazole was initiated, but despite clinical improvement the patient unexpectedly passed away and autopsy was declined.
Discussion: Pathologic gastric candidiasis is rare in immunocompetent hosts. Although Candida species can be part of normal gastrointestinal flora, mucosal injury can allow pathogenic transition. This patient lacked classic risk factors like HIV, malignancy, or prolonged antibiotic or antacid use, but age and diabetes may have contributed to relative immunosuppression. Diagnosing gastrointestinal candidiasis is challenging, as blood cultures often fail to detect Candida. Endoscopic biopsy and histopathology are critical for diagnosis. In this case the necrosis with fungal pseudohyphae suggests true infection over colonization. Prompt recognition is essential, as gastric candidiasis carries high morbidity and mortality. This case highlights the need to consider fungal infections in atypical gastric ulcers, even without overt immunosuppression.
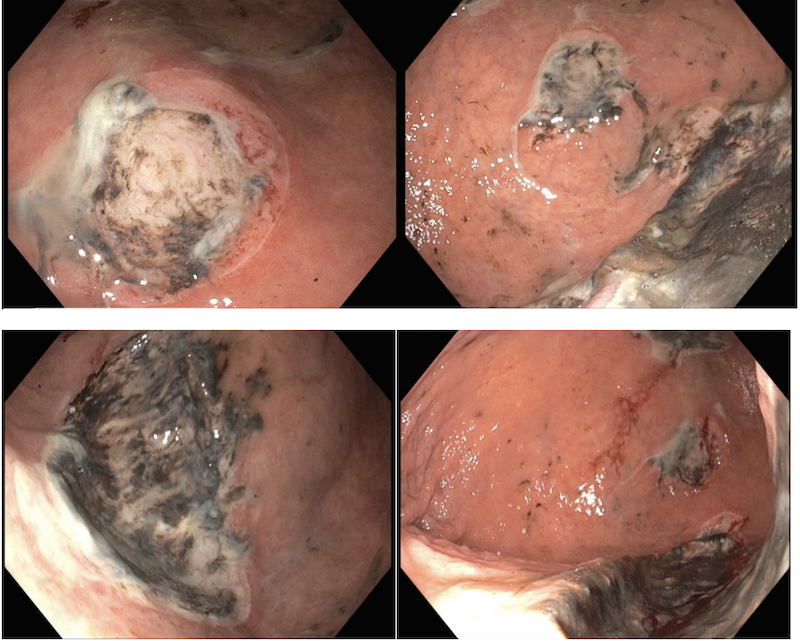
Figure: Figure 1. Endoscopy with multiple large deep cratered ulcers with adherent dark material
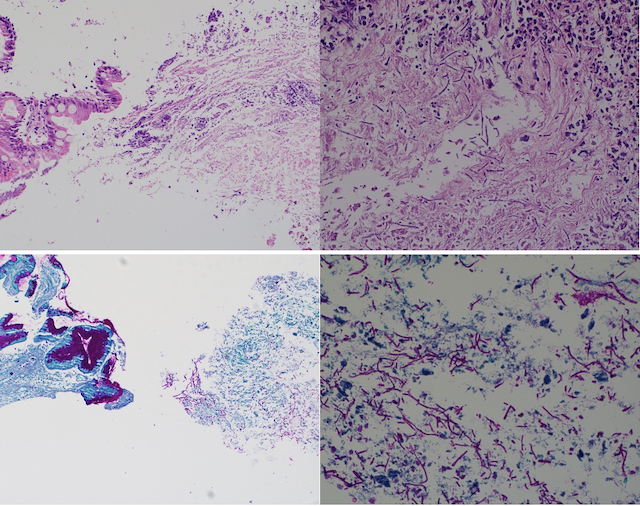
Figure: Figure 2. Histology H&E and PAS of gastric mucosa with intestinal metaplasia adjacent to necroinflammatory debris with abundant pseudohyphae consistent with Candida
Disclosures:
Garrett Teskey indicated no relevant financial relationships.
Wesley Chow indicated no relevant financial relationships.
Sevag Hamamah indicated no relevant financial relationships.
Steven Gauerke indicated no relevant financial relationships.
Faizi Hai indicated no relevant financial relationships.
Garrett Teskey, DO1, Wesley Chow, MD2, Sevag Hamamah, DO2, Steven Gauerke, MD2, Faizi Hai, MD2. P3498 - Beyond Colonization: A Rare Case of Invasive Gastric Candidiasis Without Traditional Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Scripps Mercy Hospital, Yorba Linda, CA; 2Scripps Mercy Hospital, San Diego, CA
Introduction: Gastric candidiasis is a rare fungal infection of the stomach that typically arises with immunosuppression, critical illness, or mucosal disruption. Symptoms such as abdominal pain, nausea, vomiting, or gastrointestinal bleeding are nonspecific. We report a case of an 89-year-old immunocompetent male presenting with acute upper gastrointestinal bleeding, in whom gastric ulcers were found to be due to candidiasis on biopsy.
Case Description/
Methods: An 89-year-old male with diabetes, hypertension, and iron deficiency anemia presented with two syncopal episodes, coffee-ground emesis, melena, and abdominal pain. He denied prior NSAID use. One month earlier, he underwent cholecystectomy for gangrenous cholecystitis; no cultures were obtained. On examination, he was hypertensive with conjunctival pallor, dry mucous membranes, and mild diffuse abdominal tenderness. Labs showed leukocytosis of 22.3, normocytic anemia of 8.9, and elevated inflammatory markers. HIV was negative. Abdominal CT revealed ascending colon wall thickening. Blood cultures grew ESBL-producing E. coli, and stool was positive for C. diff. He was treated with meropenem and oral vancomycin. Upper endoscopy showed multiple large deep cratered gastric ulcers with dark adherent material on both curvatures and normal esophagus and duodenum. Biopsies revealed marked chronic active gastritis with ulceration, intestinal metaplasia, and necroinflammatory debris with abundant fungal pseudohyphae on PAS staining. Gastrin, chromogranin, H. pylori, CMV, and AFB stains were negative. Fluconazole was initiated, but despite clinical improvement the patient unexpectedly passed away and autopsy was declined.
Discussion: Pathologic gastric candidiasis is rare in immunocompetent hosts. Although Candida species can be part of normal gastrointestinal flora, mucosal injury can allow pathogenic transition. This patient lacked classic risk factors like HIV, malignancy, or prolonged antibiotic or antacid use, but age and diabetes may have contributed to relative immunosuppression. Diagnosing gastrointestinal candidiasis is challenging, as blood cultures often fail to detect Candida. Endoscopic biopsy and histopathology are critical for diagnosis. In this case the necrosis with fungal pseudohyphae suggests true infection over colonization. Prompt recognition is essential, as gastric candidiasis carries high morbidity and mortality. This case highlights the need to consider fungal infections in atypical gastric ulcers, even without overt immunosuppression.
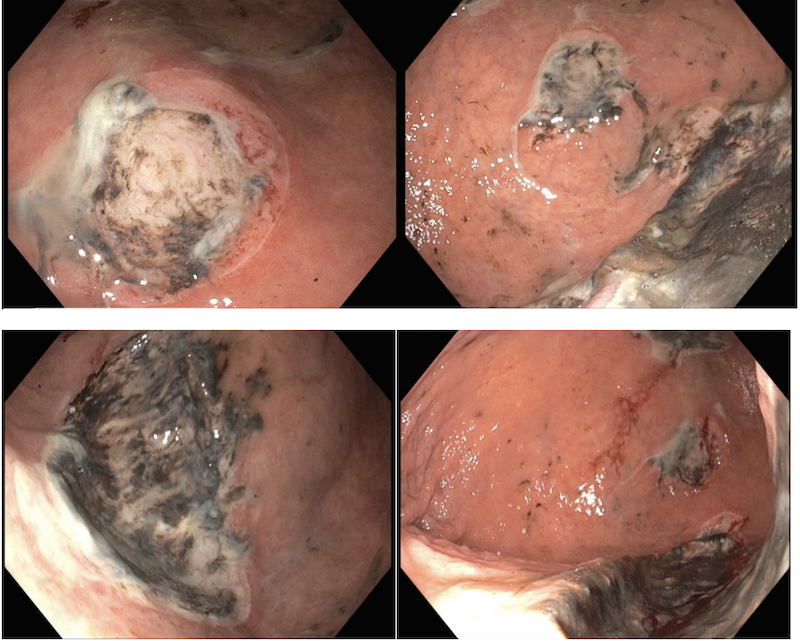
Figure: Figure 1. Endoscopy with multiple large deep cratered ulcers with adherent dark material
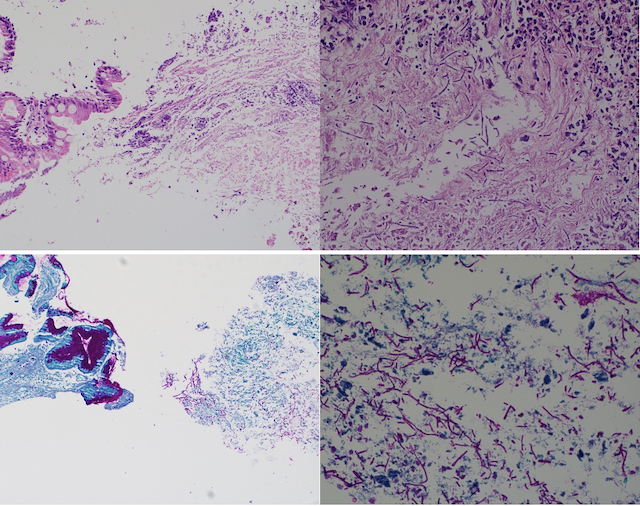
Figure: Figure 2. Histology H&E and PAS of gastric mucosa with intestinal metaplasia adjacent to necroinflammatory debris with abundant pseudohyphae consistent with Candida
Disclosures:
Garrett Teskey indicated no relevant financial relationships.
Wesley Chow indicated no relevant financial relationships.
Sevag Hamamah indicated no relevant financial relationships.
Steven Gauerke indicated no relevant financial relationships.
Faizi Hai indicated no relevant financial relationships.
Garrett Teskey, DO1, Wesley Chow, MD2, Sevag Hamamah, DO2, Steven Gauerke, MD2, Faizi Hai, MD2. P3498 - Beyond Colonization: A Rare Case of Invasive Gastric Candidiasis Without Traditional Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
