Monday Poster Session
Category: Infections and Microbiome
P3465 - Colonic Clue to a Hidden Diagnosis: Isolated GI Histoplasmosis in an Unaware HIV Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bassel Dakkak, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Bassel Dakkak, MD1, Leen Kayali, MD1, Ibrahim Shanti, MD1, Abdelwahap Elghezewi, MD2, Hesham Awadh, MD1, Mujtaba Mohamed, MD1
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Barboursville, WV
Introduction: Histoplasmosis is an opportunistic fungal infection primarily affecting immunocompromised individuals, particularly those with AIDS. While pulmonary involvement is most common, gastrointestinal (GI) manifestations are rare and often underrecognized. This case of disseminated histoplasmosis is notable for its presentation with isolated GI symptoms, highlighting the need for awareness of atypical presentations to ensure timely diagnosis and management.
Case Description/
Methods: A 32-year-old man with a history of recurrent esophageal candidiasis presented with fever (103.1°F), nausea, vomiting, and 30-pound weight loss over a year. On arrival, he was tachycardic, with a blood pressure of 137/87 mmHg. Admission labs shown in Table 1. Empiric vancomycin and piperacillin-tazobactam were started for suspected sepsis. Due to pancytopenia and transaminitis, doxycycline was added for possible tick-borne disease which is endemic to the patient's region, and IV fluconazole was added to cover for candidiasis. A CT abdomen/pelvis showed right upper quadrant fat stranding, suggestive of duodenitis or pancreatitis. CMV titers were elevated, though PCR was negative. Human immunodeficiency virus (HIV) enzyme-linked immunosorbent assay (ELISA) was positive, with a viral load of 1,881,584 and CD4 count of 25. Endoscopy revealed gastritis and colonoscopy showed a 13 mm ulcer in the ascending colon and mild inflammation in the transverse colon (Figure 1 A-B). Biopsy showed necrotizing granulomas with positive fungal stains (Figure 1 C-D). Histoplasmosis urine antigen was positive. Lumbar puncture was unremarkable. Subsequently, the patient was started on antiretroviral therapy (bictegravir, emtricitabine, tenofovir) and Amphotericin B, followed by itraconazole. After two months, liver function test normalized, the viral load dropped down, the CD4 count improved, and GI symptoms resolved..
Discussion: Disseminated histoplasmosis poses diagnostic challenges due to its nonspecific presentation. Isolated GI involvement is extremely rare and can mimic other common conditions like inflammatory bowel disease. In such patients, GI histoplasmosis should be considered early, especially prior to initiating immunosuppressive therapy. This case highlights the importance of considering histoplasmosis in patients without known immunosuppression and unexplained GI symptoms, as it may be the first clue to undiagnosed HIV and delays in diagnosis can have serious consequences.
AI was used to refine language only.
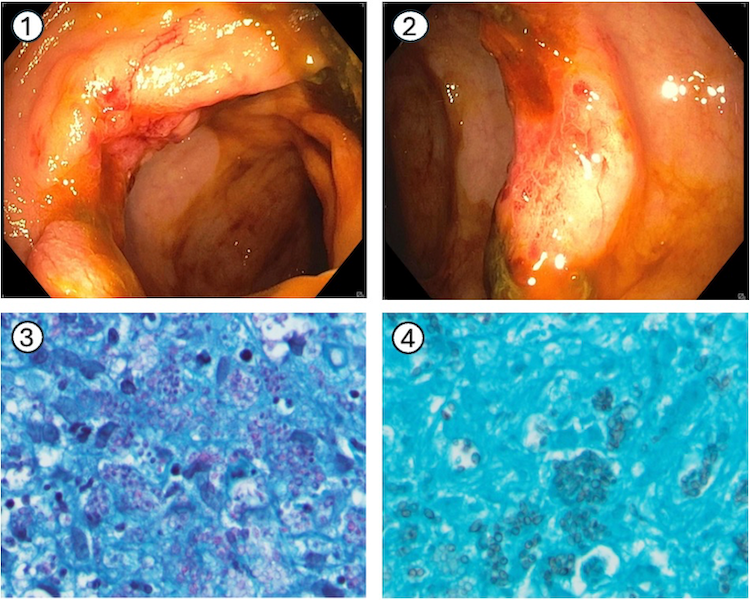
Figure: Table 1. Abnormal Laboratory Findings on Admission.
WBC- White Blood Cell count/ AST- Aspartate Aminotransferase/ ALT - Alanine Aminotransferase/ ALP - Alkaline phosphatase/ HIV- Human Immunodeficiency Virus
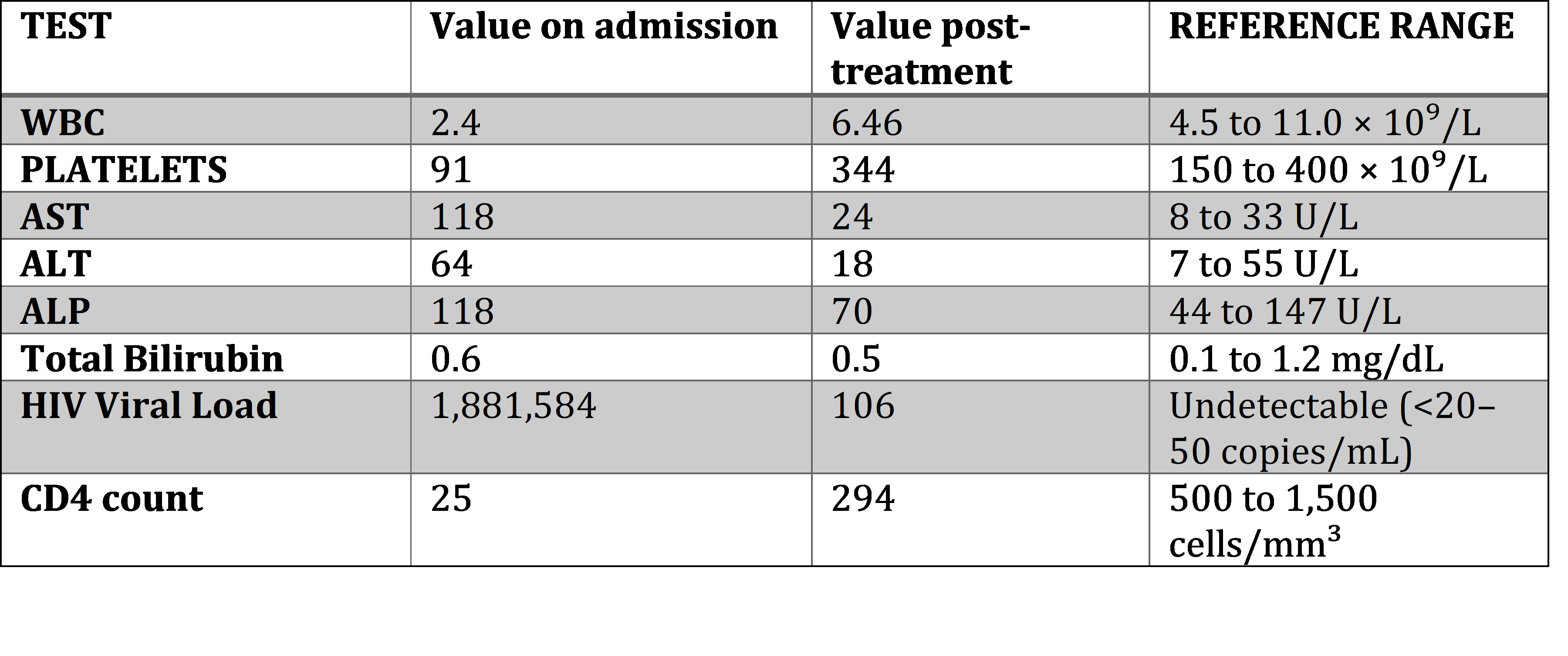
Figure: Figure 1. Endoscopic and histopathologic findings
A-B: Colonoscopy images showing inflamed, erythematous mucosa with ulceration.
C-D: Periodic acid–Schiff (PAS) staining demonstrating intracellular yeast forms within necrotizing granulomas and Grocott’s methenamine silver (GMS) stain highlighting numerous fungal organisms consistent with Histoplasma capsulatum.
Disclosures:
Bassel Dakkak indicated no relevant financial relationships.
Leen Kayali indicated no relevant financial relationships.
Ibrahim Shanti indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Hesham Awadh indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Bassel Dakkak, MD1, Leen Kayali, MD1, Ibrahim Shanti, MD1, Abdelwahap Elghezewi, MD2, Hesham Awadh, MD1, Mujtaba Mohamed, MD1. P3465 - Colonic Clue to a Hidden Diagnosis: Isolated GI Histoplasmosis in an Unaware HIV Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Barboursville, WV
Introduction: Histoplasmosis is an opportunistic fungal infection primarily affecting immunocompromised individuals, particularly those with AIDS. While pulmonary involvement is most common, gastrointestinal (GI) manifestations are rare and often underrecognized. This case of disseminated histoplasmosis is notable for its presentation with isolated GI symptoms, highlighting the need for awareness of atypical presentations to ensure timely diagnosis and management.
Case Description/
Methods: A 32-year-old man with a history of recurrent esophageal candidiasis presented with fever (103.1°F), nausea, vomiting, and 30-pound weight loss over a year. On arrival, he was tachycardic, with a blood pressure of 137/87 mmHg. Admission labs shown in Table 1. Empiric vancomycin and piperacillin-tazobactam were started for suspected sepsis. Due to pancytopenia and transaminitis, doxycycline was added for possible tick-borne disease which is endemic to the patient's region, and IV fluconazole was added to cover for candidiasis. A CT abdomen/pelvis showed right upper quadrant fat stranding, suggestive of duodenitis or pancreatitis. CMV titers were elevated, though PCR was negative. Human immunodeficiency virus (HIV) enzyme-linked immunosorbent assay (ELISA) was positive, with a viral load of 1,881,584 and CD4 count of 25. Endoscopy revealed gastritis and colonoscopy showed a 13 mm ulcer in the ascending colon and mild inflammation in the transverse colon (Figure 1 A-B). Biopsy showed necrotizing granulomas with positive fungal stains (Figure 1 C-D). Histoplasmosis urine antigen was positive. Lumbar puncture was unremarkable. Subsequently, the patient was started on antiretroviral therapy (bictegravir, emtricitabine, tenofovir) and Amphotericin B, followed by itraconazole. After two months, liver function test normalized, the viral load dropped down, the CD4 count improved, and GI symptoms resolved..
Discussion: Disseminated histoplasmosis poses diagnostic challenges due to its nonspecific presentation. Isolated GI involvement is extremely rare and can mimic other common conditions like inflammatory bowel disease. In such patients, GI histoplasmosis should be considered early, especially prior to initiating immunosuppressive therapy. This case highlights the importance of considering histoplasmosis in patients without known immunosuppression and unexplained GI symptoms, as it may be the first clue to undiagnosed HIV and delays in diagnosis can have serious consequences.
AI was used to refine language only.
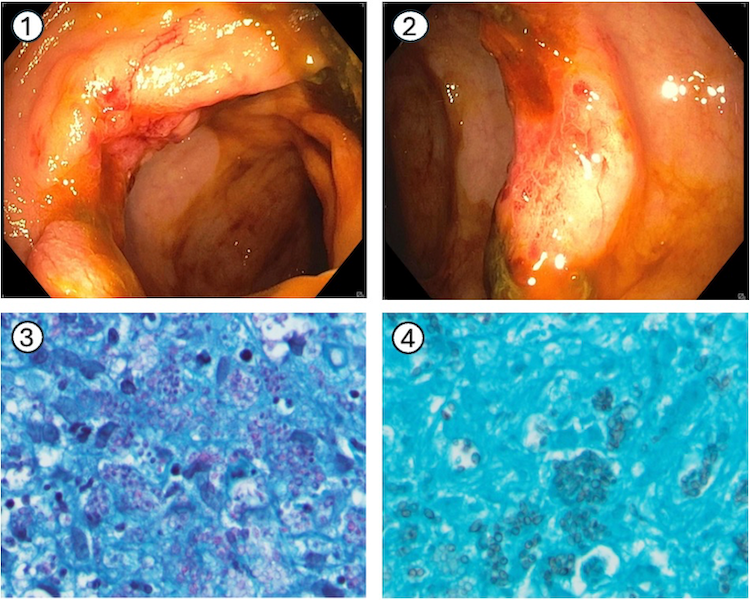
Figure: Table 1. Abnormal Laboratory Findings on Admission.
WBC- White Blood Cell count/ AST- Aspartate Aminotransferase/ ALT - Alanine Aminotransferase/ ALP - Alkaline phosphatase/ HIV- Human Immunodeficiency Virus
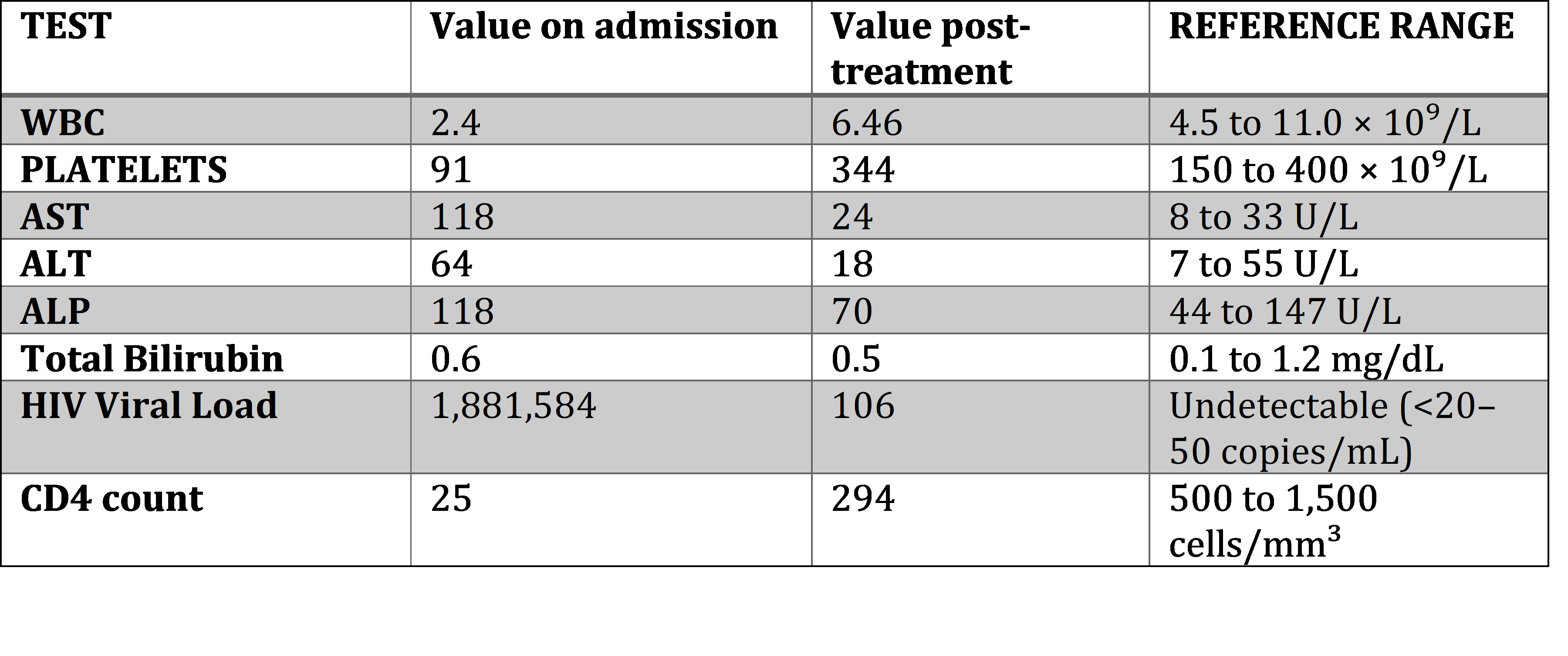
Figure: Figure 1. Endoscopic and histopathologic findings
A-B: Colonoscopy images showing inflamed, erythematous mucosa with ulceration.
C-D: Periodic acid–Schiff (PAS) staining demonstrating intracellular yeast forms within necrotizing granulomas and Grocott’s methenamine silver (GMS) stain highlighting numerous fungal organisms consistent with Histoplasma capsulatum.
Disclosures:
Bassel Dakkak indicated no relevant financial relationships.
Leen Kayali indicated no relevant financial relationships.
Ibrahim Shanti indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Hesham Awadh indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Bassel Dakkak, MD1, Leen Kayali, MD1, Ibrahim Shanti, MD1, Abdelwahap Elghezewi, MD2, Hesham Awadh, MD1, Mujtaba Mohamed, MD1. P3465 - Colonic Clue to a Hidden Diagnosis: Isolated GI Histoplasmosis in an Unaware HIV Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
