Monday Poster Session
Category: Infections and Microbiome
P3434 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following COVID-19 Infection: A Global Population-Based Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yilin Song, MD (she/her/hers)
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Yilin Song, MD1, Thai Hau Koo, MD2, Benjamin Liu, MD3, Linda Zhong, MD4, Tao Bai, MD5, Xiaohua Hou, MD5, Lei Tu, MD5, Gengqing Song, MD6
1University of Maryland Medical Center, Baltimore, MD; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4Nanyang Technological University, Singapore, Singapore; 5Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 6Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Coronavirus disease 2019 (COVID-19) is associated with gastrointestinal (GI) symptoms, potentially due to disturbances in gut microbiota or dysfunction of the renin-angiotensin system. Small intestinal bacterial overgrowth (SIBO) is emerging as a significant GI sequela post-COVID-19 infection. However, large-scale real-world data assessing SIBO risk post-COVID-19 infection across different age groups are limited. This study aimed to evaluate the prevalence and incidence of SIBO post-COVID-19 infection in a global population-based cohort and identify key associated risk factors.
Methods: A retrospective study was conducted with the TriNetX database, encompassing over 275 million de-identified patient records. Adult patients (≥18 years) diagnosed with SIBO post COVID-19 infection after January 1st, 2022, to May 30th, 2024, were included to align with the global adoption of SIBO diagnostic coding time and a 12-month follow-up period. Patients with prior SIBO, concurrent viral infections including influenza, prior surgeries of the GI tract, and inflammatory bowel disease were excluded. Propensity score matching (PSM, 1:1) was adjusted for demographics and SIBO risk factors. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of SIBO within 12 months.
Results: A total of 1,660,092 COVID-19 patients and 42,322,017 controls were analyzed. SIBO was diagnosed in 353 COVID-19 patients and 3,368 controls without hydrogen breath tests (BT), and in 78 COVID-19 patients and 871 controls using BT. Overall, COVID-19 infection significantly increased the risk of developing SIBO within 12 months post-infection compared to non-infected controls. Specifically, COVID-19 patients aged 60–69 and 70–79 years had the highest SIBO risk at 12 months (0.011% vs. 0.004–0.005% in controls). Elevated SIBO risks were also significant in younger groups at 12 months: ages 30–39 (OR 2.7; 95% CI 1.3–5.8; p=0.002) and 40–49 (OR 2.4; 95% CI 1.1–5.0; p< 0.0001). Additionally, COVID-19 patients had significantly higher rates of GI comorbidities, chronic opioid use, proton pump inhibitor therapy, and antidiarrheal medication use.
Discussion: COVID-19 significantly increases the risk of SIBO within 12-month post-infection, particularly among older adults and patients with specific GI comorbidities or chronic medication use. Prospective studies are warranted to explore underlying mechanisms and develop effective interventions for SIBO prevention and treatment.
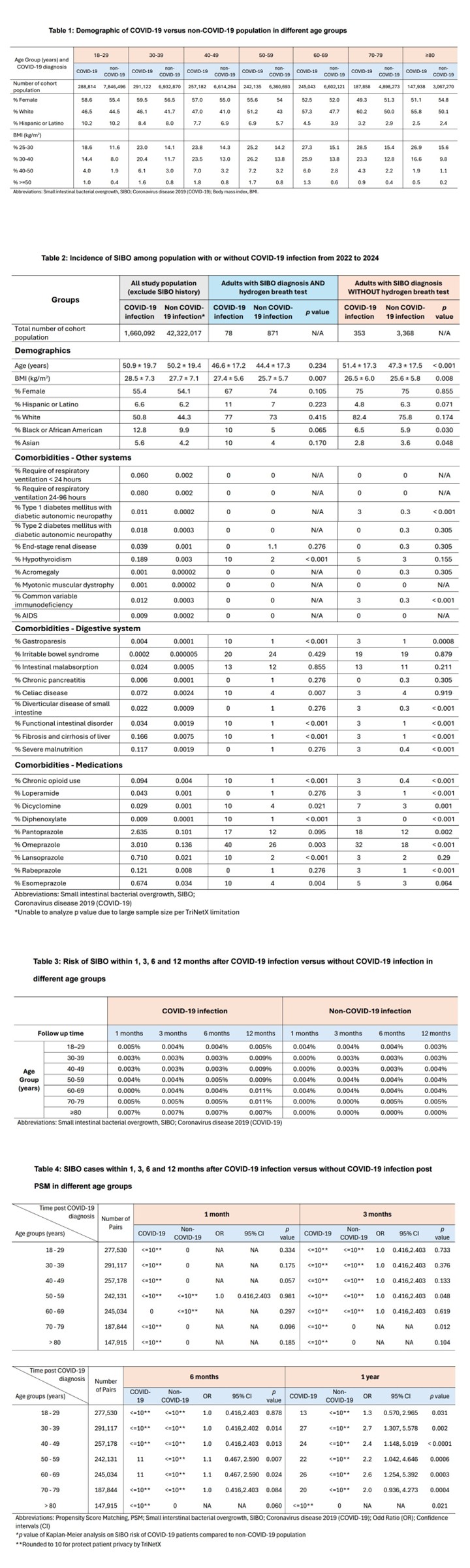
Figure: Table 1: Demographic of COVID-19 versus non-COVID-19 population in different age groups
Table 2: Incidence of SIBO among population with or without COVID-19 infection from 2022 to 2024
Table 3: Risk of SIBO within 1, 3, 6 and 12 months after COVID-19 infection versus without COVID-19 infection in
different age groups
Table 4: SIBO cases within 1, 3, 6 and 12 months after COVID-19 infection versus without COVID-19 infection post
PSM in different age groups
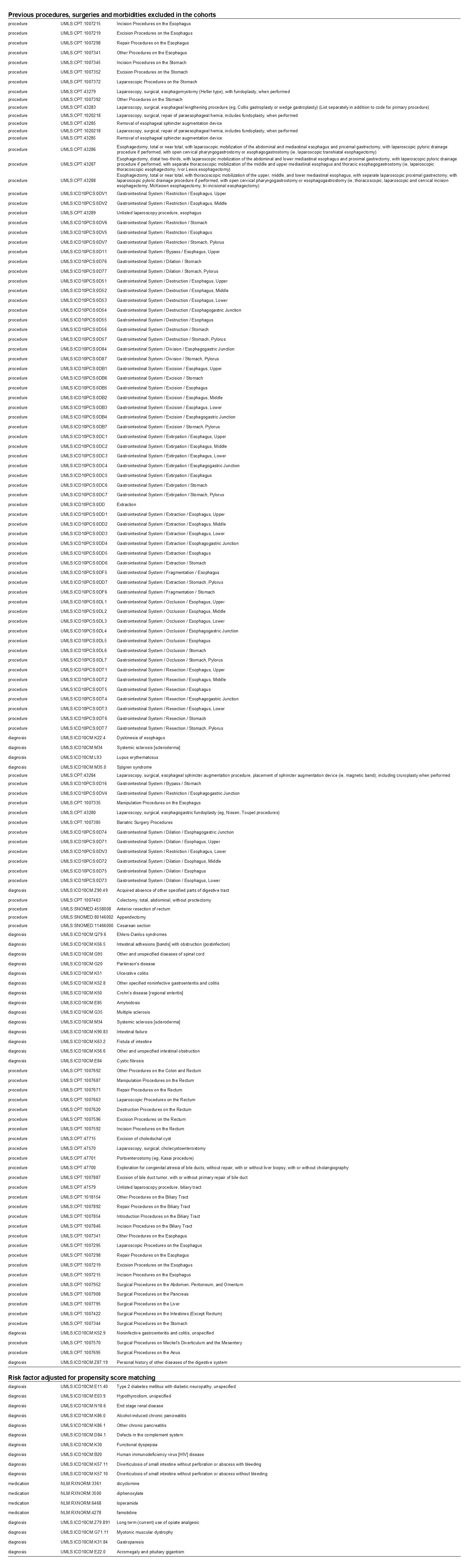
Figure: Supplement 1: Exclusion criteria and risk factors of SIBO for propensity score matching
Disclosures:
Yilin Song indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Linda Zhong indicated no relevant financial relationships.
Tao Bai indicated no relevant financial relationships.
Xiaohua Hou indicated no relevant financial relationships.
Lei Tu indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Yilin Song, MD1, Thai Hau Koo, MD2, Benjamin Liu, MD3, Linda Zhong, MD4, Tao Bai, MD5, Xiaohua Hou, MD5, Lei Tu, MD5, Gengqing Song, MD6. P3434 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following COVID-19 Infection: A Global Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4Nanyang Technological University, Singapore, Singapore; 5Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 6Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Coronavirus disease 2019 (COVID-19) is associated with gastrointestinal (GI) symptoms, potentially due to disturbances in gut microbiota or dysfunction of the renin-angiotensin system. Small intestinal bacterial overgrowth (SIBO) is emerging as a significant GI sequela post-COVID-19 infection. However, large-scale real-world data assessing SIBO risk post-COVID-19 infection across different age groups are limited. This study aimed to evaluate the prevalence and incidence of SIBO post-COVID-19 infection in a global population-based cohort and identify key associated risk factors.
Methods: A retrospective study was conducted with the TriNetX database, encompassing over 275 million de-identified patient records. Adult patients (≥18 years) diagnosed with SIBO post COVID-19 infection after January 1st, 2022, to May 30th, 2024, were included to align with the global adoption of SIBO diagnostic coding time and a 12-month follow-up period. Patients with prior SIBO, concurrent viral infections including influenza, prior surgeries of the GI tract, and inflammatory bowel disease were excluded. Propensity score matching (PSM, 1:1) was adjusted for demographics and SIBO risk factors. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of SIBO within 12 months.
Results: A total of 1,660,092 COVID-19 patients and 42,322,017 controls were analyzed. SIBO was diagnosed in 353 COVID-19 patients and 3,368 controls without hydrogen breath tests (BT), and in 78 COVID-19 patients and 871 controls using BT. Overall, COVID-19 infection significantly increased the risk of developing SIBO within 12 months post-infection compared to non-infected controls. Specifically, COVID-19 patients aged 60–69 and 70–79 years had the highest SIBO risk at 12 months (0.011% vs. 0.004–0.005% in controls). Elevated SIBO risks were also significant in younger groups at 12 months: ages 30–39 (OR 2.7; 95% CI 1.3–5.8; p=0.002) and 40–49 (OR 2.4; 95% CI 1.1–5.0; p< 0.0001). Additionally, COVID-19 patients had significantly higher rates of GI comorbidities, chronic opioid use, proton pump inhibitor therapy, and antidiarrheal medication use.
Discussion: COVID-19 significantly increases the risk of SIBO within 12-month post-infection, particularly among older adults and patients with specific GI comorbidities or chronic medication use. Prospective studies are warranted to explore underlying mechanisms and develop effective interventions for SIBO prevention and treatment.
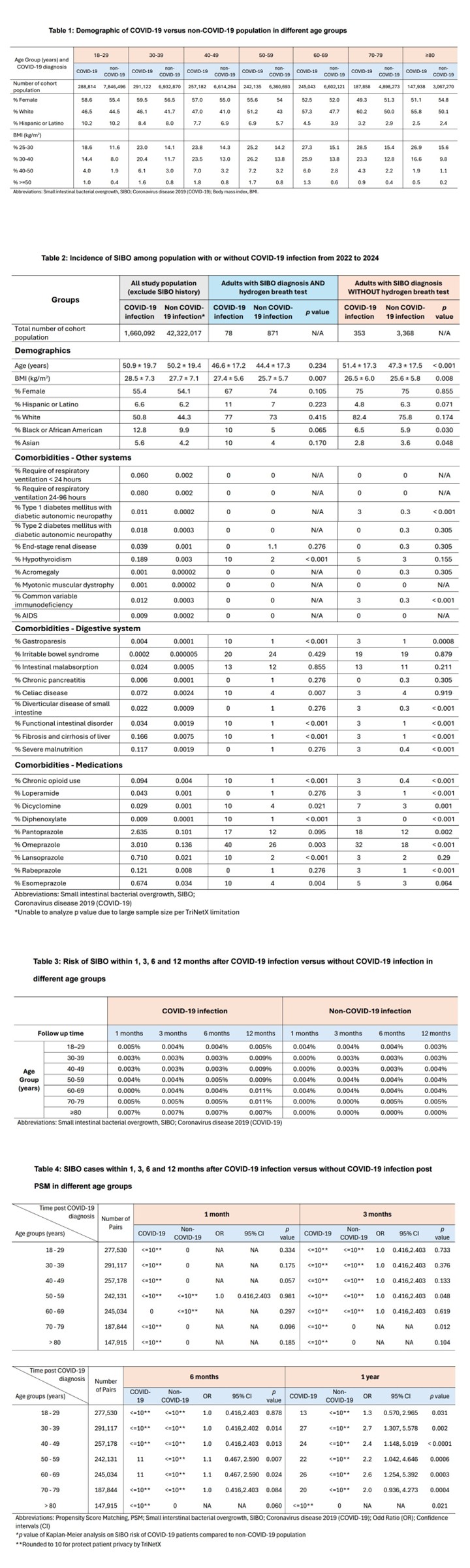
Figure: Table 1: Demographic of COVID-19 versus non-COVID-19 population in different age groups
Table 2: Incidence of SIBO among population with or without COVID-19 infection from 2022 to 2024
Table 3: Risk of SIBO within 1, 3, 6 and 12 months after COVID-19 infection versus without COVID-19 infection in
different age groups
Table 4: SIBO cases within 1, 3, 6 and 12 months after COVID-19 infection versus without COVID-19 infection post
PSM in different age groups
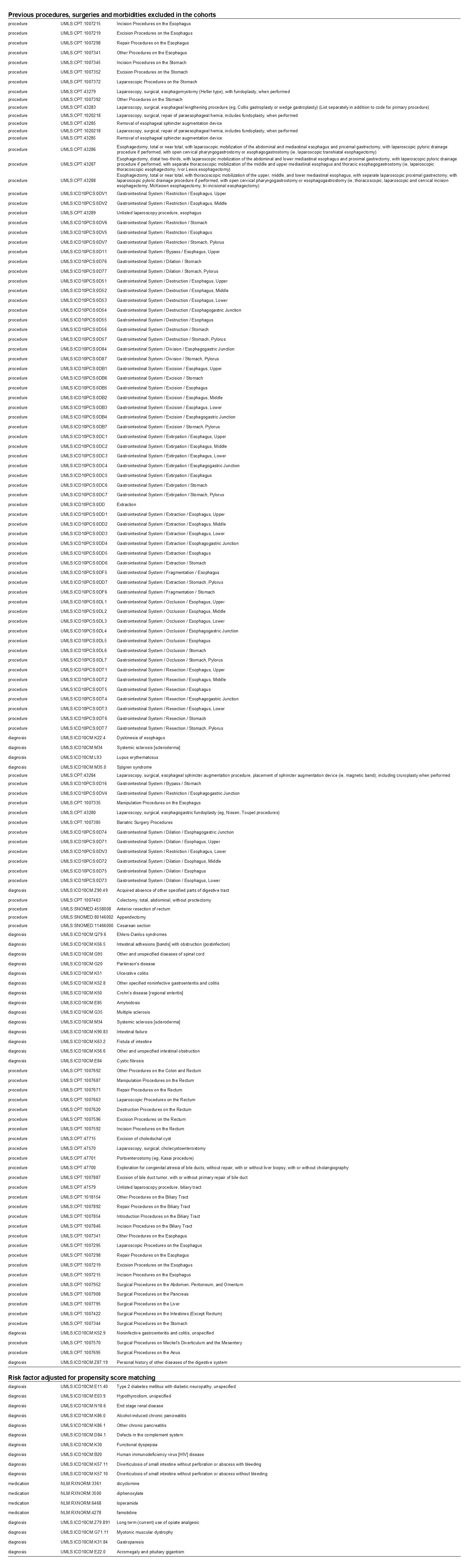
Figure: Supplement 1: Exclusion criteria and risk factors of SIBO for propensity score matching
Disclosures:
Yilin Song indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Linda Zhong indicated no relevant financial relationships.
Tao Bai indicated no relevant financial relationships.
Xiaohua Hou indicated no relevant financial relationships.
Lei Tu indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Yilin Song, MD1, Thai Hau Koo, MD2, Benjamin Liu, MD3, Linda Zhong, MD4, Tao Bai, MD5, Xiaohua Hou, MD5, Lei Tu, MD5, Gengqing Song, MD6. P3434 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following COVID-19 Infection: A Global Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

