Monday Poster Session
Category: Infections and Microbiome
P3427 - An Outbreak of Shigellosis Among People Experiencing Homelessness and Opioid Use Disorder in Philadelphia, PA
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JS
Joshua Samudre, MD (he/him/his)
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Joshua Samudre, MD1, Lindsay A. Matthews, MD2, Christa Smaltz, MD3, Holly Greenwald, MD1
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3Temple University, Philadelphia, PA
Introduction: During the fall and winter of 2023-2024, there was an outbreak of Shigellosis in the greater Philadelphia area, disproportionately affecting vulnerable populations facing housing instability and those with opioid use disorder. We aim to characterize this outbreak in the present study.
Methods: We performed a retrospective chart review of 67 patients seen at our tertiary care with confirmed Shigella infection. Data collected included diagnostic modalities, housing status, opioid use disorder and injection behaviors, and endoscopic and imaging data.
Results: Of 67 patients, 40 (59.7%) were men. 21 (31.3%) had positive blood cultures, 32 (47.8%) had positive stool culture, and 25 (37.3%) had positive PCR GI pathogen panel. The PCR-based GI pathogen panel was the only positive testing in 19 (28.3%). 45 patients (67.1%) had housing insecurity. 45 (67.1%) had opioid use disorder, with 35 (52.2%) with injection behaviors. Of the 46 patients (68.6%) with abdominal imaging, 19 (41.3%) had small bowel involvement, 24 (52.1%) had pancolitis, 2 (4.3%) had right-sided only disease, 8 (17.4%) had left-sided disease, and 7 (15.2%) had inflammation confined to the rectosigmoid area. 5 (7.5%) of patients had lower endoscopy (flexible sigmoidoscopy or colonoscopy), and 4 patients (6.0%) were treated with steroids for presumed inflammatory bowel disease (IBD) prior to the diagnosis of Shigellosis. There was 1 death (CFR 1.5%).
Discussion: Our cohort had a substantial rate of bacteremia, particularly among those with opioid and injection drug use. We postulate this could be due to either direct inoculation from IV drug use, or through open wounds from drug use. Infectious etiologies remain an important consideration when evaluating a patient with bloody diarrhea, especially with the risk factors identified in our study of drug use and housing insecurity. Importantly, PCR-based GI pathogen panels identified over 28% of cases missed by conventional cultures. Increased availability of PCR panels, especially in-house testing, has the potential to significantly impact patient care. In our cohort, 4 patients were treated for presumed IBD, highlighting the need to consider invasive infectious diarrhea prior to initiating steroids. Immunosuppression in the setting of active Shigellosis can worsen outcomes and delay appropriate therapy. Because of the infectious nature and high rates of bacteremia with Shigellosis, the need for accurate and swift diagnosis is paramount.
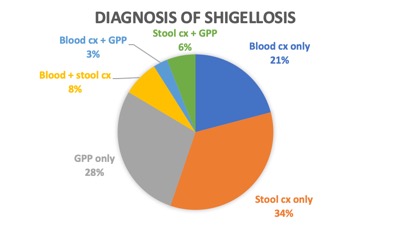
Figure: Diagnostic results during the fall and winter of 2023-2024 Shigellosis outbreak in the greater Philadelphia area
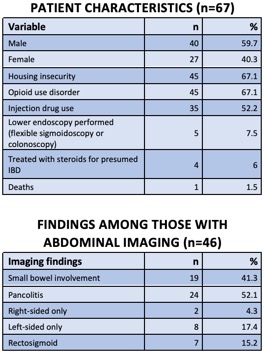
Figure: Patient characteristics and abdominal imaging findings among the study cohort
Disclosures:
Joshua Samudre indicated no relevant financial relationships.
Lindsay Matthews indicated no relevant financial relationships.
Christa Smaltz indicated no relevant financial relationships.
Holly Greenwald indicated no relevant financial relationships.
Joshua Samudre, MD1, Lindsay A. Matthews, MD2, Christa Smaltz, MD3, Holly Greenwald, MD1. P3427 - An Outbreak of Shigellosis Among People Experiencing Homelessness and Opioid Use Disorder in Philadelphia, PA, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3Temple University, Philadelphia, PA
Introduction: During the fall and winter of 2023-2024, there was an outbreak of Shigellosis in the greater Philadelphia area, disproportionately affecting vulnerable populations facing housing instability and those with opioid use disorder. We aim to characterize this outbreak in the present study.
Methods: We performed a retrospective chart review of 67 patients seen at our tertiary care with confirmed Shigella infection. Data collected included diagnostic modalities, housing status, opioid use disorder and injection behaviors, and endoscopic and imaging data.
Results: Of 67 patients, 40 (59.7%) were men. 21 (31.3%) had positive blood cultures, 32 (47.8%) had positive stool culture, and 25 (37.3%) had positive PCR GI pathogen panel. The PCR-based GI pathogen panel was the only positive testing in 19 (28.3%). 45 patients (67.1%) had housing insecurity. 45 (67.1%) had opioid use disorder, with 35 (52.2%) with injection behaviors. Of the 46 patients (68.6%) with abdominal imaging, 19 (41.3%) had small bowel involvement, 24 (52.1%) had pancolitis, 2 (4.3%) had right-sided only disease, 8 (17.4%) had left-sided disease, and 7 (15.2%) had inflammation confined to the rectosigmoid area. 5 (7.5%) of patients had lower endoscopy (flexible sigmoidoscopy or colonoscopy), and 4 patients (6.0%) were treated with steroids for presumed inflammatory bowel disease (IBD) prior to the diagnosis of Shigellosis. There was 1 death (CFR 1.5%).
Discussion: Our cohort had a substantial rate of bacteremia, particularly among those with opioid and injection drug use. We postulate this could be due to either direct inoculation from IV drug use, or through open wounds from drug use. Infectious etiologies remain an important consideration when evaluating a patient with bloody diarrhea, especially with the risk factors identified in our study of drug use and housing insecurity. Importantly, PCR-based GI pathogen panels identified over 28% of cases missed by conventional cultures. Increased availability of PCR panels, especially in-house testing, has the potential to significantly impact patient care. In our cohort, 4 patients were treated for presumed IBD, highlighting the need to consider invasive infectious diarrhea prior to initiating steroids. Immunosuppression in the setting of active Shigellosis can worsen outcomes and delay appropriate therapy. Because of the infectious nature and high rates of bacteremia with Shigellosis, the need for accurate and swift diagnosis is paramount.
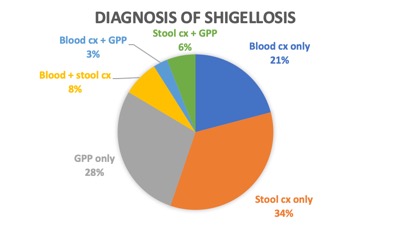
Figure: Diagnostic results during the fall and winter of 2023-2024 Shigellosis outbreak in the greater Philadelphia area
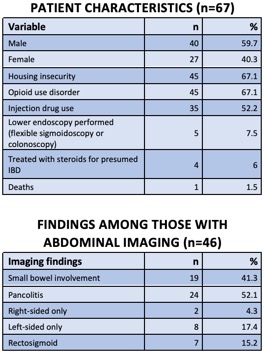
Figure: Patient characteristics and abdominal imaging findings among the study cohort
Disclosures:
Joshua Samudre indicated no relevant financial relationships.
Lindsay Matthews indicated no relevant financial relationships.
Christa Smaltz indicated no relevant financial relationships.
Holly Greenwald indicated no relevant financial relationships.
Joshua Samudre, MD1, Lindsay A. Matthews, MD2, Christa Smaltz, MD3, Holly Greenwald, MD1. P3427 - An Outbreak of Shigellosis Among People Experiencing Homelessness and Opioid Use Disorder in Philadelphia, PA, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

