Monday Poster Session
Category: IBD
P3400 - Inflammatory Bowel Disaster
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JJ
Jenny Joseph, MBBS (she/her/hers)
Norwalk Hospital/Yale University
Norwalk, CT
Presenting Author(s)
Jenny Joseph, MBBS1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Zablon Sewalem, MD, MSc1, Syed Alishan Nasir, MD2, Rakhee Mangla, MD2
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Immune checkpoint inhibitors (ICI) have revolutionized cancer treatment but uncovered a realm of adverse events. Enhanced T cell activity inadvertently leads to self-antigen recognition predominantly at the barrier organs, which results in a plethora of gastrointestinal adverse events that are well documented with treatment guidelines. GI side effects can often be refractory to traditional immunosuppressants and require an experimental approach to management. We present a case of severe ICI enterocolitis where biologic therapy led to colonic improvement but failed to resolve enteritis.
Case Description/
Methods: A 58-year-old man with renal cell cancer on ICI presented with Grade III ICI colitis refractory to oral steroids. Imaging demonstrated enteritis and colonoscopy revealed severe colitis with mucosal ulceration. After three induction doses of infliximab (5 mg/kg), repeat colonoscopy showed excellent response in colitis, yet diarrhea worsened. Repeat imaging showed worsening enteritis and subsequent small bowel endoscopy showed severe mucosal friability, erythema, and ulceration in the ileum (Fig 1A), and biopsies confirmed ICI enteritis. Following failure to respond despite therapeutic infliximab levels, upadacitinib 45 mg and high dose steroids were initiated. Despite more than 40 days of treatment with upadacitinib, he had profuse diarrhea, protein loss enteropathy and malnutrition. Imaging at this stage revealed that the enteritis had extended proximally, and push enteroscopy demonstrated severe mucosal inflammation now affecting the proximal jejunum as well (Fig 1B). Vedolizumab 300mg (3 doses) was added, but diarrhea and malnutrition persisted. Unfortunately, he succumbed to bacteremia from immunosuppression.
Discussion: This case underscores the challenge of treating ICI enteritis. While agents like infliximab and JAK inhibitors have shown efficacy in colitis, they may not adequately target small bowel inflammation. Our patient had a near complete colonic response, but his enteritis continued to worsen, indicating that biologic therapy preferentially addresses inflammation in the colon. Small bowel disease is not only difficult to control in ICI enterocolitis but also in IBD which suggests that small bowel inflammation is either triggered by alternate mechanisms or variable drug bioavailability within the small bowel. Further research is needed to better understand and manage small bowel inflammation in ICI toxicity and IBD.
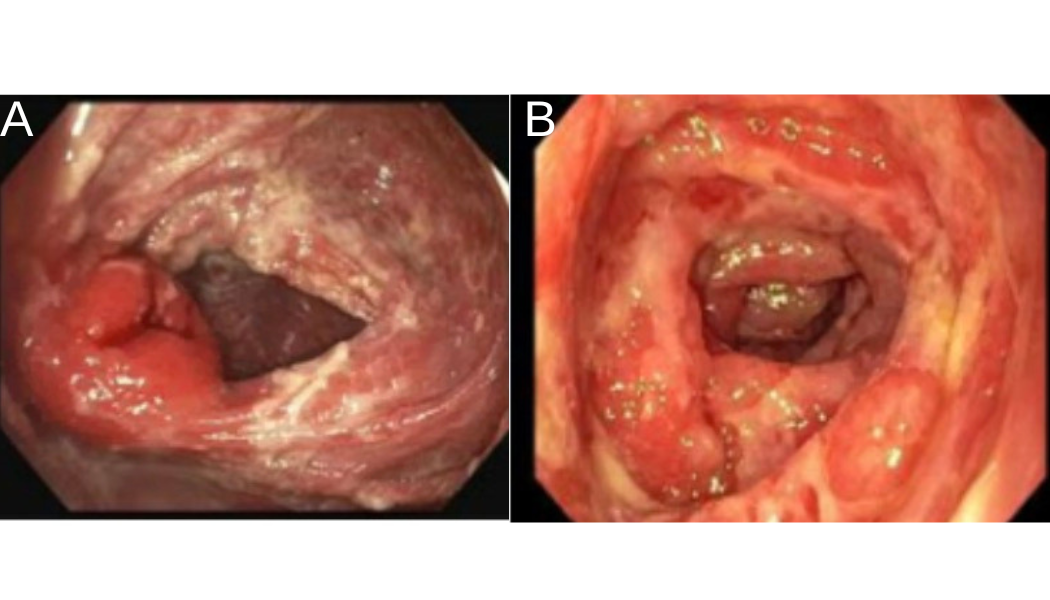
Figure: Figure 1 A. Inflamed ileocecal valve. B. Inflamed jejunum with erosions visualized 8 weeks later
Disclosures:
Jenny Joseph indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Syed Alishan Nasir indicated no relevant financial relationships.
Rakhee Mangla indicated no relevant financial relationships.
Jenny Joseph, MBBS1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Zablon Sewalem, MD, MSc1, Syed Alishan Nasir, MD2, Rakhee Mangla, MD2. P3400 - Inflammatory Bowel Disaster, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Immune checkpoint inhibitors (ICI) have revolutionized cancer treatment but uncovered a realm of adverse events. Enhanced T cell activity inadvertently leads to self-antigen recognition predominantly at the barrier organs, which results in a plethora of gastrointestinal adverse events that are well documented with treatment guidelines. GI side effects can often be refractory to traditional immunosuppressants and require an experimental approach to management. We present a case of severe ICI enterocolitis where biologic therapy led to colonic improvement but failed to resolve enteritis.
Case Description/
Methods: A 58-year-old man with renal cell cancer on ICI presented with Grade III ICI colitis refractory to oral steroids. Imaging demonstrated enteritis and colonoscopy revealed severe colitis with mucosal ulceration. After three induction doses of infliximab (5 mg/kg), repeat colonoscopy showed excellent response in colitis, yet diarrhea worsened. Repeat imaging showed worsening enteritis and subsequent small bowel endoscopy showed severe mucosal friability, erythema, and ulceration in the ileum (Fig 1A), and biopsies confirmed ICI enteritis. Following failure to respond despite therapeutic infliximab levels, upadacitinib 45 mg and high dose steroids were initiated. Despite more than 40 days of treatment with upadacitinib, he had profuse diarrhea, protein loss enteropathy and malnutrition. Imaging at this stage revealed that the enteritis had extended proximally, and push enteroscopy demonstrated severe mucosal inflammation now affecting the proximal jejunum as well (Fig 1B). Vedolizumab 300mg (3 doses) was added, but diarrhea and malnutrition persisted. Unfortunately, he succumbed to bacteremia from immunosuppression.
Discussion: This case underscores the challenge of treating ICI enteritis. While agents like infliximab and JAK inhibitors have shown efficacy in colitis, they may not adequately target small bowel inflammation. Our patient had a near complete colonic response, but his enteritis continued to worsen, indicating that biologic therapy preferentially addresses inflammation in the colon. Small bowel disease is not only difficult to control in ICI enterocolitis but also in IBD which suggests that small bowel inflammation is either triggered by alternate mechanisms or variable drug bioavailability within the small bowel. Further research is needed to better understand and manage small bowel inflammation in ICI toxicity and IBD.
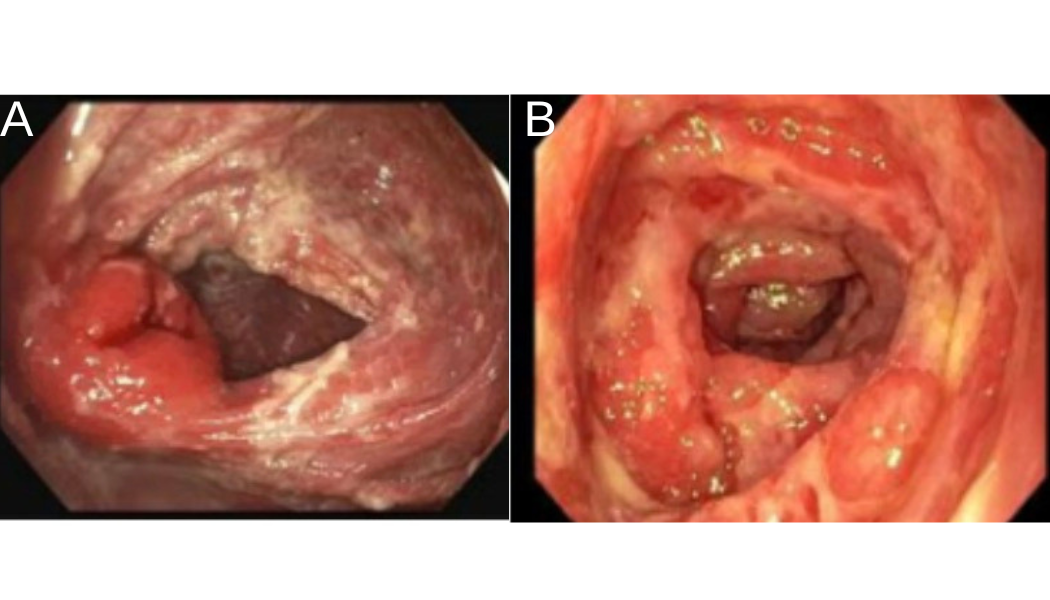
Figure: Figure 1 A. Inflamed ileocecal valve. B. Inflamed jejunum with erosions visualized 8 weeks later
Disclosures:
Jenny Joseph indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Syed Alishan Nasir indicated no relevant financial relationships.
Rakhee Mangla indicated no relevant financial relationships.
Jenny Joseph, MBBS1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Zablon Sewalem, MD, MSc1, Syed Alishan Nasir, MD2, Rakhee Mangla, MD2. P3400 - Inflammatory Bowel Disaster, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
