Monday Poster Session
Category: IBD
P3395 - Not All That Heals Is Harmless: A Case of Infliximab-Induced Acute Interstitial Nephritis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Yash P. Ashara, MBBS (he/him/his)
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Yash P. Ashara, MBBS1, Naoshin Khan, MD1, Ahila Manivannan, MD2, Karan Mathur, MD2
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI
Introduction: Treatment of Crohn’s disease (CD) has been revolutionized within the last decade with the discoveries of newer biologics. Anti TNF-alpha therapies such as infliximab have improved functional outcomes in moderate to severe CD. However, given its immune modulatory effects, it has been associated with many adverse effects including infusion reactions, infections, and renal disorders. We present a rare case of biopsy proven acute interstitial nephritis (AIN) in CD treated with infliximab, highlighting the need for clinical suspicion of unexplained renal dysfunction with biologic therapy.
Case Description/
Methods: A 24-year-old male with a 13-year history of stricturing and fistulizing CD requiring multiple surgical interventions presented to the hospital from clinic due to worsening acute kidney injury (AKI). The patient had been on Infliximab for 4 years but was placed on hold for a few months due to inter-abdominal abscesses requiring antibiotics and surgical treatment. Infliximab was subsequently restarted. However, within two months of re-starting therapy, creatinine increased to 2.11 from normal and peaked at 4.85 in 7 months. At the time, differential included obstructive uropathy secondary to enteric hyperoxaluria, renal artery thrombosis, AIN, and amyloidosis. Work-up included renal ultrasound with doppler which showed no stones or thrombosis. Serum protein electrophoresis was negative as well. Due to unclear etiology, renal biopsy was performed which showed chronic active tubulointerstitial nephritis which was attributed to Infliximab. The patient was subsequently treated with high dose prednisone with tapering which improved renal function to 2.14. The decision was made to transition patient to Ustekinumab for further management of CD.
Discussion: AKI secondary to AIN can present with nonspecific symptoms in setting of abrupt deterioration of renal function. There have been rare instances of AKI associated with infliximab, likely linked to nephritis or vasculitis. In this case, the temporal relationship between infliximab re-initiation and the onset of renal dysfunction, along with histopathologic confirmation of AIN, strongly supports a causal association. Possible mechanism could be due to hypersensitivity reaction or immune complex deposition. Given the widespread use of biologics, clinician should be aware of AIN. Routine monitoring of renal function, especially during initial months of biologic initiation, may help in early detection.
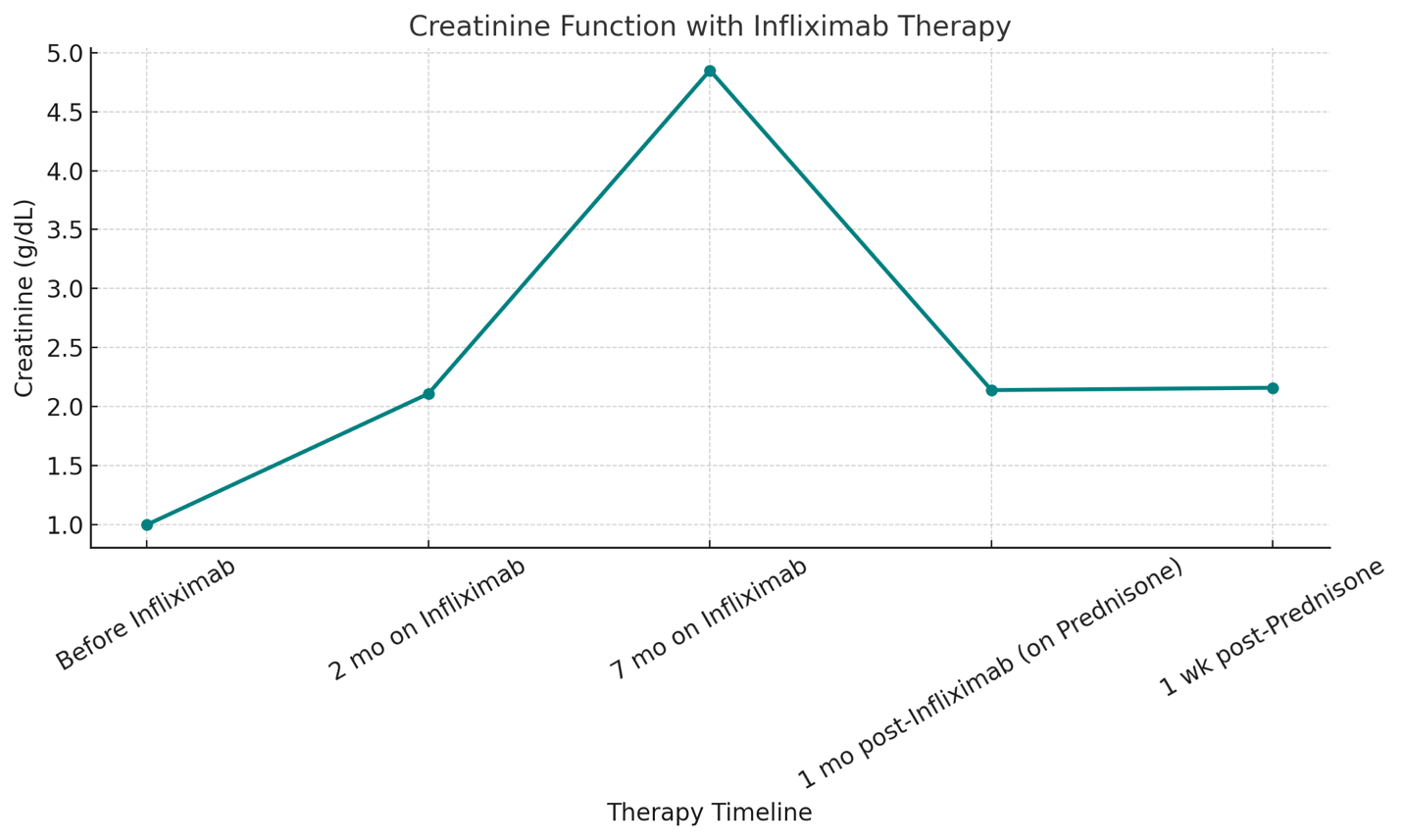
Figure: Line Chart of Renal Function
Disclosures:
Yash Ashara indicated no relevant financial relationships.
Naoshin Khan indicated no relevant financial relationships.
Ahila Manivannan indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Yash P. Ashara, MBBS1, Naoshin Khan, MD1, Ahila Manivannan, MD2, Karan Mathur, MD2. P3395 - Not All That Heals Is Harmless: A Case of Infliximab-Induced Acute Interstitial Nephritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI
Introduction: Treatment of Crohn’s disease (CD) has been revolutionized within the last decade with the discoveries of newer biologics. Anti TNF-alpha therapies such as infliximab have improved functional outcomes in moderate to severe CD. However, given its immune modulatory effects, it has been associated with many adverse effects including infusion reactions, infections, and renal disorders. We present a rare case of biopsy proven acute interstitial nephritis (AIN) in CD treated with infliximab, highlighting the need for clinical suspicion of unexplained renal dysfunction with biologic therapy.
Case Description/
Methods: A 24-year-old male with a 13-year history of stricturing and fistulizing CD requiring multiple surgical interventions presented to the hospital from clinic due to worsening acute kidney injury (AKI). The patient had been on Infliximab for 4 years but was placed on hold for a few months due to inter-abdominal abscesses requiring antibiotics and surgical treatment. Infliximab was subsequently restarted. However, within two months of re-starting therapy, creatinine increased to 2.11 from normal and peaked at 4.85 in 7 months. At the time, differential included obstructive uropathy secondary to enteric hyperoxaluria, renal artery thrombosis, AIN, and amyloidosis. Work-up included renal ultrasound with doppler which showed no stones or thrombosis. Serum protein electrophoresis was negative as well. Due to unclear etiology, renal biopsy was performed which showed chronic active tubulointerstitial nephritis which was attributed to Infliximab. The patient was subsequently treated with high dose prednisone with tapering which improved renal function to 2.14. The decision was made to transition patient to Ustekinumab for further management of CD.
Discussion: AKI secondary to AIN can present with nonspecific symptoms in setting of abrupt deterioration of renal function. There have been rare instances of AKI associated with infliximab, likely linked to nephritis or vasculitis. In this case, the temporal relationship between infliximab re-initiation and the onset of renal dysfunction, along with histopathologic confirmation of AIN, strongly supports a causal association. Possible mechanism could be due to hypersensitivity reaction or immune complex deposition. Given the widespread use of biologics, clinician should be aware of AIN. Routine monitoring of renal function, especially during initial months of biologic initiation, may help in early detection.
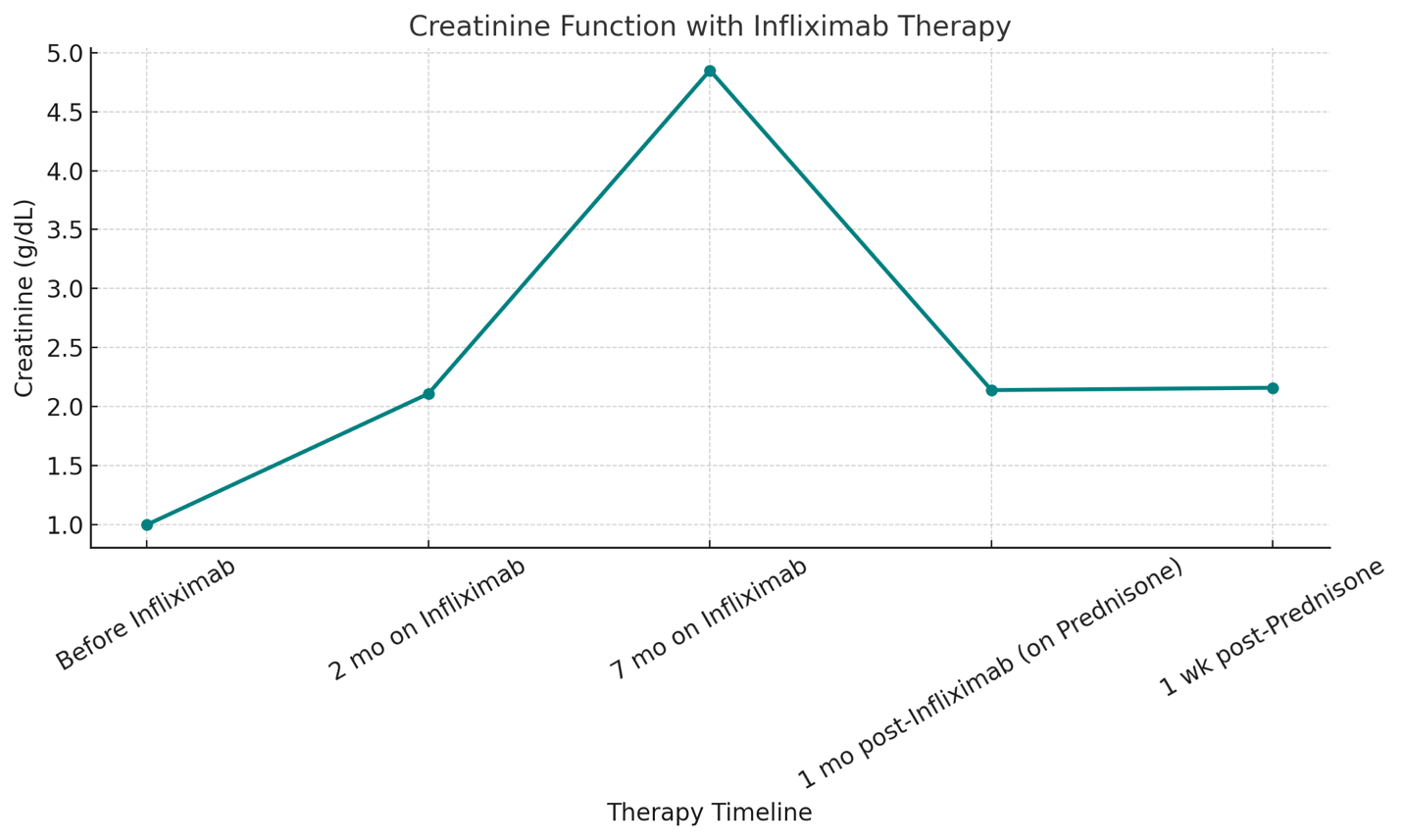
Figure: Line Chart of Renal Function
Disclosures:
Yash Ashara indicated no relevant financial relationships.
Naoshin Khan indicated no relevant financial relationships.
Ahila Manivannan indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Yash P. Ashara, MBBS1, Naoshin Khan, MD1, Ahila Manivannan, MD2, Karan Mathur, MD2. P3395 - Not All That Heals Is Harmless: A Case of Infliximab-Induced Acute Interstitial Nephritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
