Monday Poster Session
Category: IBD
P3388 - De Novo Crohn’s Disease Following SCT
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rachel DJ Cruz Nieves, MD (she/her/hers)
University of Virginia
Charlottesville, VA
Presenting Author(s)
Rachel DJ. Cruz Nieves, MD1, Neha Rajpal, MD1, Madison Karabinus, DO1, Andrew Copland, MD2, Christopher Moskaluk, MD, PhD1
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
Introduction: Graft-versus-host disease (GVHD) is a possible complication of allogeneic stem cell transplant (ASCT). It occurs due to a T cell-mediated response from the donor bone marrow against the host. Histologic evidence of GI GVHD includes epithelial cell apoptosis without signs of chronic changes such as forking. Similarly, Crohn’s disease and other inflammatory bowel diseases are also due to T cell-mediated destruction of host cells. Histology of Crohn’s disease includes crypt architectural distortion and signs of chronic inflammation such as remodeling and metaplasia.
Case Description/
Methods: We present a case report of de novo Crohn's disease in a 22-year-old woman with aplastic anemia who received an allogeneic stem cell transplant (SCT). One year following the SCT, she developed abdominal pain, nausea, vomiting, and weight loss, prompting clinical suspicion of gastrointestinal (GI) graft-versus-host disease (GVHD). She was treated with ruxolitinib for 10 months; however, her symptoms persisted, and she developed refractory diarrhea, prompting hospitalization and an inpatient GI consultation. Routine stool studies were negative. Colonoscopy revealed patchy moderate inflammation characterized by erythema and shallow ulcerations throughout the entire colon, and localized pseudo-polyps in the sigmoid colon. Biopsies demonstrated a marked increase in chronic inflammation involving the mucosal lamina propria and submucosa, including chronic changes such as glandular forking, as well as active inflammation with neutrophilic cryptitis— consistent with inflammatory bowel disease (IBD). Terminal ileum biopsy demonstrated pyloric metaplasia, again more typical of Crohn’s disease than GVHD. While GVHD is histologically characterized by effacement of the crypt epithelium via apoptosis, crypt remodeling is not typically seen and is more indicative of IBD.The patient was subsequently initiated on budesonide, with improvement in her symptoms, and planned initiation of vedolizumab in the outpatient setting.
Discussion: This case demonstrates how histopathology can be critical in establishing a diagnosis in patients who develop GI symptoms following SCT, particularly when clinical symptoms and endoscopic findings amongst common mimickers of GI-GVHD can be difficult to distinguish from the disease itself. Furthermore, although there have been several reported cases of potential treatment of Crohn’s disease with SCT, here we report a case of de novo Crohn’s disease that may have been influenced by SCT.
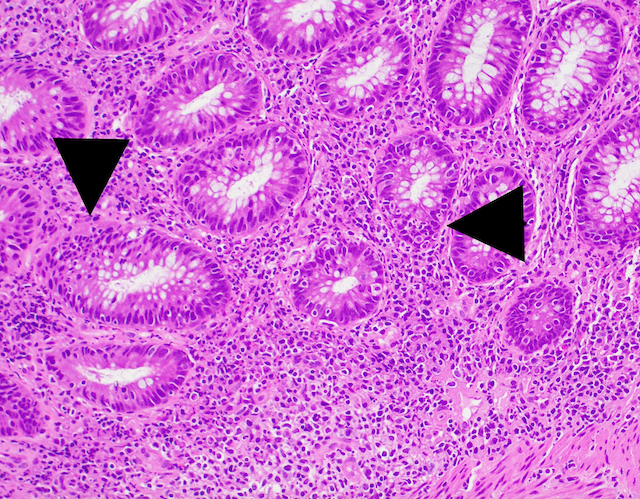
Figure: Several foci of neutrophilic cryptitis (black arrowheads). This type of inflammation, along with the increased chronic inflammation is typical of IBD and not GVHD.
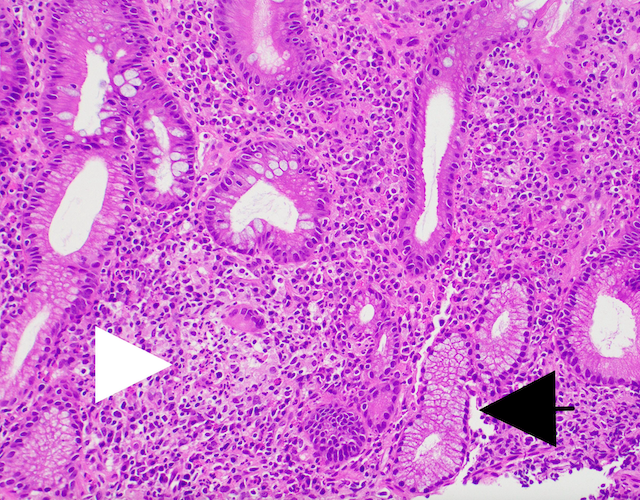
Figure: Terminal ileum (TI) displaying pyloric metaplasia (black arrowhead). This type of metaplasia is typical of Crohn’s disease and not GVHD. The TI shows a crypt destroyed by active inflammation (white arrowhead) which is typical of IBD and not GVHD.
Disclosures:
Rachel Cruz Nieves indicated no relevant financial relationships.
Neha Rajpal indicated no relevant financial relationships.
Madison Karabinus indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Christopher Moskaluk indicated no relevant financial relationships.
Rachel DJ. Cruz Nieves, MD1, Neha Rajpal, MD1, Madison Karabinus, DO1, Andrew Copland, MD2, Christopher Moskaluk, MD, PhD1. P3388 - <i>De Novo</i> Crohn’s Disease Following SCT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
Introduction: Graft-versus-host disease (GVHD) is a possible complication of allogeneic stem cell transplant (ASCT). It occurs due to a T cell-mediated response from the donor bone marrow against the host. Histologic evidence of GI GVHD includes epithelial cell apoptosis without signs of chronic changes such as forking. Similarly, Crohn’s disease and other inflammatory bowel diseases are also due to T cell-mediated destruction of host cells. Histology of Crohn’s disease includes crypt architectural distortion and signs of chronic inflammation such as remodeling and metaplasia.
Case Description/
Methods: We present a case report of de novo Crohn's disease in a 22-year-old woman with aplastic anemia who received an allogeneic stem cell transplant (SCT). One year following the SCT, she developed abdominal pain, nausea, vomiting, and weight loss, prompting clinical suspicion of gastrointestinal (GI) graft-versus-host disease (GVHD). She was treated with ruxolitinib for 10 months; however, her symptoms persisted, and she developed refractory diarrhea, prompting hospitalization and an inpatient GI consultation. Routine stool studies were negative. Colonoscopy revealed patchy moderate inflammation characterized by erythema and shallow ulcerations throughout the entire colon, and localized pseudo-polyps in the sigmoid colon. Biopsies demonstrated a marked increase in chronic inflammation involving the mucosal lamina propria and submucosa, including chronic changes such as glandular forking, as well as active inflammation with neutrophilic cryptitis— consistent with inflammatory bowel disease (IBD). Terminal ileum biopsy demonstrated pyloric metaplasia, again more typical of Crohn’s disease than GVHD. While GVHD is histologically characterized by effacement of the crypt epithelium via apoptosis, crypt remodeling is not typically seen and is more indicative of IBD.The patient was subsequently initiated on budesonide, with improvement in her symptoms, and planned initiation of vedolizumab in the outpatient setting.
Discussion: This case demonstrates how histopathology can be critical in establishing a diagnosis in patients who develop GI symptoms following SCT, particularly when clinical symptoms and endoscopic findings amongst common mimickers of GI-GVHD can be difficult to distinguish from the disease itself. Furthermore, although there have been several reported cases of potential treatment of Crohn’s disease with SCT, here we report a case of de novo Crohn’s disease that may have been influenced by SCT.
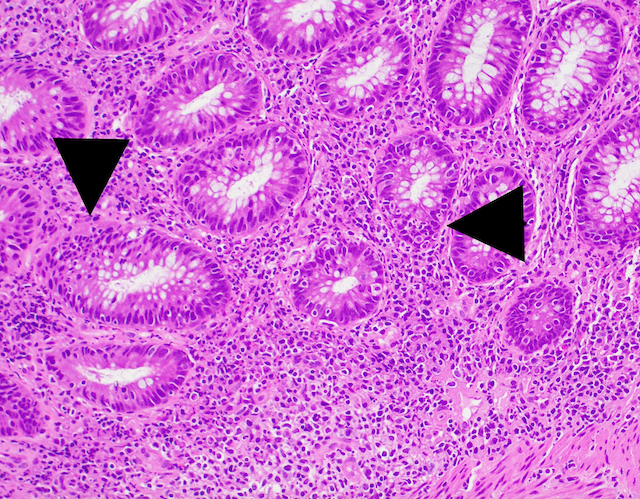
Figure: Several foci of neutrophilic cryptitis (black arrowheads). This type of inflammation, along with the increased chronic inflammation is typical of IBD and not GVHD.
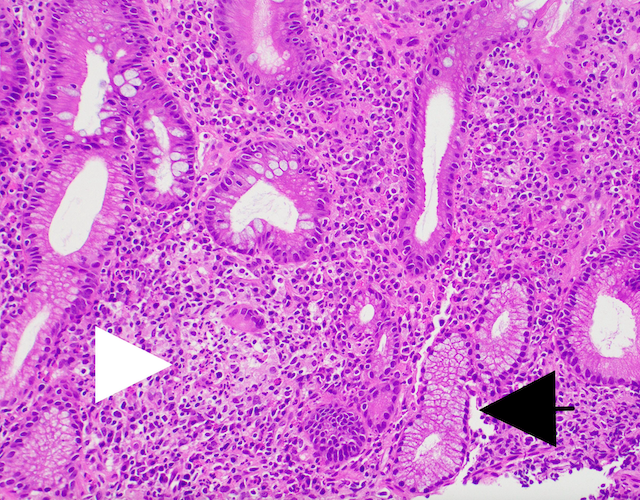
Figure: Terminal ileum (TI) displaying pyloric metaplasia (black arrowhead). This type of metaplasia is typical of Crohn’s disease and not GVHD. The TI shows a crypt destroyed by active inflammation (white arrowhead) which is typical of IBD and not GVHD.
Disclosures:
Rachel Cruz Nieves indicated no relevant financial relationships.
Neha Rajpal indicated no relevant financial relationships.
Madison Karabinus indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Christopher Moskaluk indicated no relevant financial relationships.
Rachel DJ. Cruz Nieves, MD1, Neha Rajpal, MD1, Madison Karabinus, DO1, Andrew Copland, MD2, Christopher Moskaluk, MD, PhD1. P3388 - <i>De Novo</i> Crohn’s Disease Following SCT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
