Monday Poster Session
Category: IBD
P3378 - A Macroscopic Mystery: An Atypical Presentation of Microscopic Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Richard Pearce, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Richard Pearce, MD, Scott Manski, MD
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Collagenous colitis (CC), a subtype of microscopic colitis, typically presents with chronic, non-bloody, watery diarrhea with a predilection towards an older, female, population. While appearing endoscopically unremarkable, histologic findings are notable for a thickened subepithelial collagen band. We present a rare case of CC with endoscopic mucosal inflammation.
Case Description/
Methods: A 78-year-old woman presented with non-bloody diarrhea, urgency, incontinence, abdominal pain, and weight loss. Workup for additional etiologies of diarrhea (TSH, celiac panel, fecal elastase, stool infectious studies) were unremarkable. An index colonoscopy revealed diffuse pancolonic inflammation. Pathology revealed focal surface erosion/denudation as well as thickening of a subepithelial collagen band felt to be consistent with CC. Budesonide and cholestyramine offered limited relief.
In the setting of persistent symptoms and fecal calprotectin elevation to 2410mcg/gm, vedolizumab was initiated. Despite dose escalation to every 4 weeks, vedolizumab yielded only a transient improvement in symptoms. A follow-up colonoscopy again showed diffuse endoscopic colonic congestion with a thickened collagen band on histology. Despite use of vedolizumab, colestipol 4gm, budesonide 9mg, and anti-diarrheals, the patient remained symptomatic with multiple bowel movements per day.
The patient was subsequently changed to infliximab. She experienced a rapid, sustained, symptom resolution with normalized bowel frequency and resolution of urgency and incontinence. A follow up calprotectin improved to 67mcg/gm.
Discussion: This case illustrates an unusual presentation of CC with endoscopic inflammation, which deviates from the classic profile of this disease. The patient’s index colonoscopy did not clearly document pseudomembranes in the findings; however review of the endoscopic images suggests their presence. Ultimately, the patient was diagnosed with an atypical presentation of inflammatory bowel disease. This case underscores the importance of recognizing atypical features of collagenous colitis and maintaining a high index of suspicion for overlapping or evolving diagnoses, particularly in those who fail conventional therapy. This case also elevates the discussion of microscopic colitis as part of a spectrum of chronic inflammatory bowel diseases.
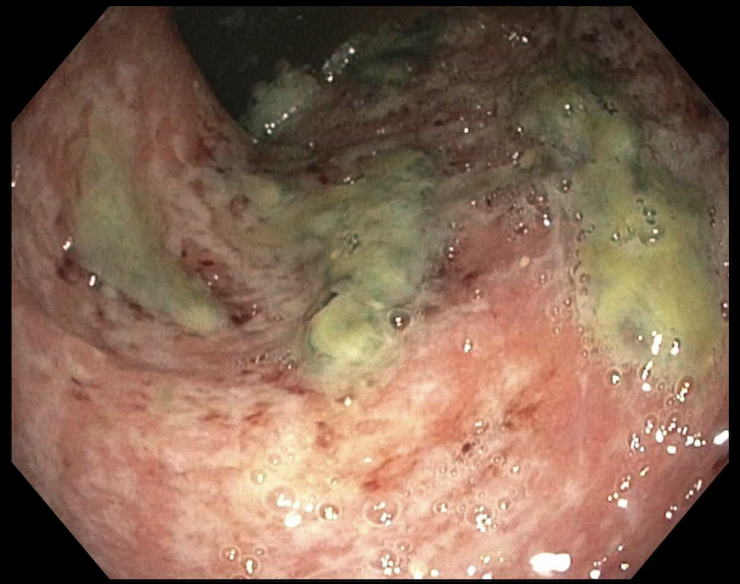
Figure: Index colonoscopy with mucosal inflammation and possible pseudomembranes
Disclosures:
Richard Pearce indicated no relevant financial relationships.
Scott Manski indicated no relevant financial relationships.
Richard Pearce, MD, Scott Manski, MD. P3378 - A Macroscopic Mystery: An Atypical Presentation of Microscopic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Collagenous colitis (CC), a subtype of microscopic colitis, typically presents with chronic, non-bloody, watery diarrhea with a predilection towards an older, female, population. While appearing endoscopically unremarkable, histologic findings are notable for a thickened subepithelial collagen band. We present a rare case of CC with endoscopic mucosal inflammation.
Case Description/
Methods: A 78-year-old woman presented with non-bloody diarrhea, urgency, incontinence, abdominal pain, and weight loss. Workup for additional etiologies of diarrhea (TSH, celiac panel, fecal elastase, stool infectious studies) were unremarkable. An index colonoscopy revealed diffuse pancolonic inflammation. Pathology revealed focal surface erosion/denudation as well as thickening of a subepithelial collagen band felt to be consistent with CC. Budesonide and cholestyramine offered limited relief.
In the setting of persistent symptoms and fecal calprotectin elevation to 2410mcg/gm, vedolizumab was initiated. Despite dose escalation to every 4 weeks, vedolizumab yielded only a transient improvement in symptoms. A follow-up colonoscopy again showed diffuse endoscopic colonic congestion with a thickened collagen band on histology. Despite use of vedolizumab, colestipol 4gm, budesonide 9mg, and anti-diarrheals, the patient remained symptomatic with multiple bowel movements per day.
The patient was subsequently changed to infliximab. She experienced a rapid, sustained, symptom resolution with normalized bowel frequency and resolution of urgency and incontinence. A follow up calprotectin improved to 67mcg/gm.
Discussion: This case illustrates an unusual presentation of CC with endoscopic inflammation, which deviates from the classic profile of this disease. The patient’s index colonoscopy did not clearly document pseudomembranes in the findings; however review of the endoscopic images suggests their presence. Ultimately, the patient was diagnosed with an atypical presentation of inflammatory bowel disease. This case underscores the importance of recognizing atypical features of collagenous colitis and maintaining a high index of suspicion for overlapping or evolving diagnoses, particularly in those who fail conventional therapy. This case also elevates the discussion of microscopic colitis as part of a spectrum of chronic inflammatory bowel diseases.
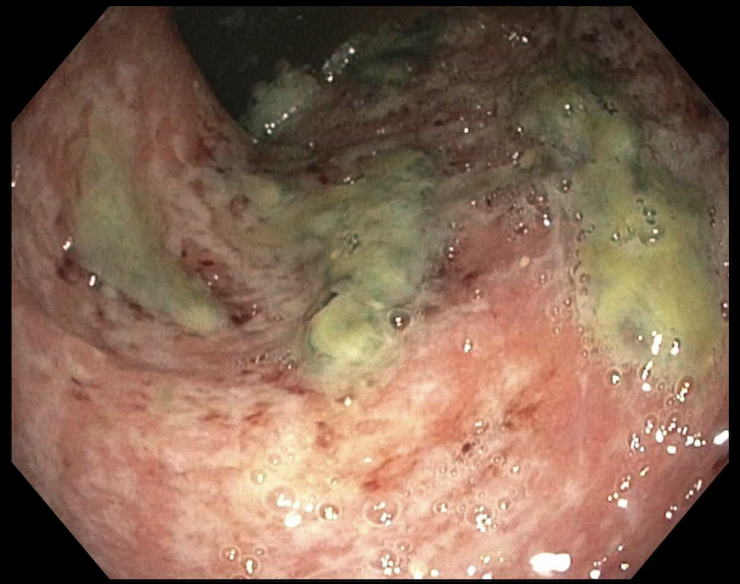
Figure: Index colonoscopy with mucosal inflammation and possible pseudomembranes
Disclosures:
Richard Pearce indicated no relevant financial relationships.
Scott Manski indicated no relevant financial relationships.
Richard Pearce, MD, Scott Manski, MD. P3378 - A Macroscopic Mystery: An Atypical Presentation of Microscopic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
